Echocardiography is a well-established diagnostic tool that provides reliable anatomic, functional, and hemodynamic data at the bedside. Reference Li, Mack and Rusk1,Reference Trambaiolo, Papetti and Posteraro2 It is somewhat expensive and requires a skilled sonographer to record, and an experienced cardiologist to interpret. Reference Trambaiolo, Papetti and Posteraro2 It is commonly used for initial diagnosis, ongoing clinical surveillance, and to support medical decision making in CHD. Reference Li, Mack and Rusk1 The Intersocietal Accreditation Commission recommends a minimum of 45 to 60 minutes to complete an echocardiogram. 3 The time and personnel required for standard paediatric echocardiography can represent a barrier in outpatient settings like rural paediatric cardiology outreach clinics, in which such resources are limited. When diagnostic goals are straightforward and limited, complete echocardiography may not be necessary, and there may be a role for focused cardiac ultrasound (FCU) using a miniaturised ultrasound device. Reference Spencer4 According to the American Society of Echocardiography, FCU is an ultrasound examination of the cardiovascular system performed by a physician to recognise specific signs that represent a narrow list of potential diagnoses in specific clinical settings. Reference Spencer, Kimura, Korcarz, Pellikka, Rahko and Siegel5 Expert focused cardiac ultrasound (eFCU) is defined as FCU performed by a level II or III echocardiographer as described by the Core Cardiology Training Symposium 4 Task Force 5. Reference Spencer, Kimura, Korcarz, Pellikka, Rahko and Siegel5,Reference Ryan, Berlacher, Lindner, Mankad, Rose and Wang6 Several studies have demonstrated FCU’s efficacy in identifying cardiac pathology in both children and adults. Reference Li, Mack and Rusk1,Reference Riley, Sable and Prasad7–Reference Khan, Wineinger, Uddin, Mehta, Rubenson and Topol9 While eFCU is not as comprehensive as standard echocardiography, it offers several advantages, including a relatively low cost and greater portability. Image acquisition takes only 2–5 minutes, and the diagnosis is immediate as the person acquiring the images is also interpreting the findings. Reference Mirabel, Celermajer, Beraud, Jouven, Marijon and Hagege10 However, previous studies have demonstrated the lack of spectral Doppler as the most significant limitation of eFCU. Reference Li, Mack and Rusk1,Reference Trambaiolo, Papetti and Posteraro2,Reference Riley, Sable and Prasad7,Reference Cardim, Fernandez Golfin and Ferreira11 Recent advancements to portable ultrasound devices now incorporate spectral Doppler interrogation that was previously unavailable. To our knowledge, feasibility and utility of eFCU with spectral Doppler has not been studied, and there are no validated guidelines for its use in follow-up for children with known CHD. The purpose of this study was to determine if eFCU that includes spectral Doppler reliably provides sufficient data to support medical decision making for patients with selected congenital cardiac lesions. Secondary aims included determining if eFCU improves the patient experience and if the addition of eFCU expands capacity in paediatric cardiology outreach clinics at remote sites.
Materials and methods
This was a prospective study conducted at two outreach clinics associated with Children’s Hospital and Medical Center in Omaha, Nebraska. The institutional review board approved the study protocol, and informed consent was obtained from all patients.
The study patients consisted of established patients who were scheduled for a clinic visit and follow-up echocardiogram with a diagnosis of ventricular septal defect, atrial septal defect, atrioventricular septal defect, patent ductus arteriosus, aortic valve stenosis, or pulmonary valve stenosis. Both repaired and unrepaired patients were included. Patients without a prior echocardiogram, those over 21 years old, and patients requiring complete echocardiography prior to an upcoming cardiac surgery were excluded. To assure informed consent, patients were excluded if they were not English speaking.
A novel assessment tool was developed for each cardiac lesion to ensure that key diagnostic objectives were identified with eFCU. The specific diagnostic objectives defined prospectively for each lesion are in Table 1. If the diagnostic objectives were not achieved with eFCU, the study was determined to be unsuccessful, and the patient was sent for a standard echocardiogram. If the diagnostic objectives were identified, the study was deemed successful and the patient did not undergo standard echocardiography. The success rate (percentage of successful eFCU among all eFCU) was calculated. Following the eFCU, the patients’ guardian (or study subject if 19 years of age or older) was asked to complete a questionnaire regarding their experience.
Table 1. Cardiac lesions and the parameters identified with expert focused cardiac ultrasound

ASD = atrial septal defect; AV = aortic valve; LA = left atrium; LV = left ventricle; LVOT = left ventricular outflow tract; MV = mitral valve; PDA = patent ductus arteriosus; PV = pulmonary valve, RA = right atrium; RV = right ventricle; RVOT = right ventricular outflow tract; TV = tricuspid valve; VSD = ventricular septal defect.
Imaging was performed with a Sonosite Edge II (Fujifilm Sonosite Inc., Bothell, WA, United States of America) portable ultrasound device. The dimensions of the device are 32.6 cm × 30.7 cm × 6.4 cm, and it weighs 4.18 kg. Images were viewed on a 30.7 cm diagonal liquid crystal display screen. A phased probe with a frequency of 5–1 MHz was used. Two-dimensional, M-mode, colour Doppler, spectral Doppler modes were available. Both still images and image loops were stored internally. The cardiologist and the fellow were trained on the device and trialled the equipment in one outreach clinic prior to subject enrolment.
Patients underwent eFCU by a single experienced paediatric cardiologist who specialises in echocardiography or a single cardiology fellow. The images obtained by the fellow were reviewed by the experienced paediatric cardiologist, and additional images were obtained if deemed necessary by the cardiologist. The images were interpreted live and stored internally for later transfer to the hospital image archiving and communication system (McKesson Cardiology TM 13.1.2, San Francisco, CA, United States of America), and were stored in the patient’s medical record.
To estimate how the use of eFCU increased the capacity of outreach clinic, patient encounters where eFCU could be used was compared to the number of available echocardiography appointments. Based on Intersocietal Accreditation Commission recommendation that 45–60 minutes is allotted for each echocardiogram, our clinic template allows a maximum of nine standard echocardiography appointments per day. Therefore, when the sum of patients with standard echocardiograms and eFCUs exceeded nine in any clinic, each patient who could receive eFCU in lieu of standard echocardiography was considered to expand the clinic capacity (Fig 1). For each of the 11 clinics studied, we compared the number of patients who could be seen in 1 day with and without the addition of eFCU using paired t-test.

Figure 1. Clinic capacity without the addition of eFCU (y + 9) and with eFCU (y + 9 + x). eFCU = expert focused cardiac ultrasound; y = no imaging needed; x = candidate for eFCU.
Results
Forty-two patients met inclusion criteria between August 2017 and June 2018 in 11 outreach clinic visits. The age ranged from 2 months to 19 years of age (mean 5.3 years), 55% female and 45% male. The median length of a scan was 7 minutes (IQR 6-11.2). Based on the guidelines in Table 1, 41 (97.7%) patients were determined to have a successful eFCU (Table 2). There was one unsuccessful exam, making the failure rate 2.3% (95% CI 0.0006–0.1256). Expert focused cardiac ultrasound did not provide complete diagnostic information in one subject with aortic stenosis, and therefore the subject underwent a standard echocardiogram. This eFCU exam failure occurred early in the study, and there was an operator error that resulted in the inability to use continuous wave Doppler to evaluate aortic valve velocity.
Table 2. Expert focused cardiac ultrasound success rate for specified cardiac lesions

n = number of patients.
One additional subject underwent echocardiography following eFCU. This subject had a history of a patent ductus arteriosus, and eFCU did not demonstrate the presence of a patent ductus arteriosus, and this proved to be correct. A complete echocardiogram was appropriately arranged because a pathologic murmur was present which did not reflect the working diagnosis of persistent patent ductus arteriosus. The child was found to have mild pulmonary stenosis. Echocardiography confirmed the eFCU imaging findings of a closed patent ductus arteriosus and was therefore considered, in the limited terms of this investigation, a successful eFCU.
An average of 20 patients was scheduled in each of the 11 outreach clinics analysed. Of these, 13 patients required cardiac imaging in each outreach clinic, and of those 4 were suitable candidates for FCU (Fig 2). The average number of complete echocardiograms performed with the implementation of eFCU was 9. There was a statistically significant difference in the number of patients who could be seen in 1 day without FCU, 15.5 compared to the number of patients who can be seen with eFCU 19 (p < 0.01).

Figure 2. Mean number of patients in the 11 outreach clinics analysed, displaying the numbers requiring and not requiring imaging, and the mean number of patients.
The satisfaction survey (Table 3) was completed by 24 guardians. Of those, 88% felt they had a better understanding of their/their child’s cardiac condition, and one parent remarked, “[I] enjoyed working with the doctor as she performed the exam. [I] liked being able to ask any questions as she worked”. Expert focused cardiac ultrasound was preferred over echocardiography in 75% of respondents with one parent stating that eFCU was “faster, more efficient”. All guardians (100%) felt that they received good clinical care with eFCU, and 67% reported that their clinic visit was enhanced with eFCU. One mother commented that eFCU was “short, sweet and to the point, the focused procedure made the whole experience very smooth”.
Table 3. Patient satisfaction questionnaire

Discussion
In this investigation, the first to evaluate the utility of eFCU with spectral Doppler capability in paediatric cardiology outreach clinics, we found that eFCU can successfully demonstrate key diagnostic objectives in patients with an atrial septal defect, ventricular septal defect, atrioventricular septal defect, pulmonary stenosis, aortic stenosis, and patent ductus arteriosus. The eFCU effectively provided information to guide continued care for these carefully selected patients. Prior studies have demonstrated the utility of FCU in regions with inadequate resources performed by healthcare providers, including nurses, medical students, and physicians, with varying levels of education. Reference Miner, Purdy and Curtis12–Reference Kirkpatrick, Nguyen and Doan14 Riley et al evaluated FCU in outpatient paediatric clinics and found that it was successful for making decisions in 79% of patients where the majority of the inadequate studies were due to insufficient colour Doppler or lack of spectral Doppler ability. Reference Riley, Sable and Prasad7 Others have also highlighted that the most significant limitation of FCU was the lack of spectral Doppler. Reference Li, Mack and Rusk1,Reference Trambaiolo, Papetti and Posteraro2,Reference Riley, Sable and Prasad7,Reference Cardim, Fernandez Golfin and Ferreira11 The use of spectral Doppler in this study permitted the interrogation of valve stenosis, shunt velocity, estimation of right ventricular pressure, and the presence or absence of outflow tract obstruction. These are crucial measurements used to inform management for children with CHD. We found that continuous wave Doppler is a necessary feature for spectral Doppler interrogation, and as other studies have shown, the absence of this feature limits eFCU’s utility.
Paediatric subspecialty care is generally restricted to larger metropolitan areas with a subsequent demand for subspecialty providers in underserved communities. Our centre provides paediatric cardiac care to approximately 1500 patients with 1750 outreach encounters each year (Fig 3). These additional clinics allow for care of patients living in nine different states. A cardiologist, nurse, and sonographer travel 50–400 miles from our tertiary care centre to the outreach clinic sites. Throughput is of great importance given the time constraints and financial burden of travelling this long distance; however, the number of patients who can be seen is limited by the need for echocardiograms.
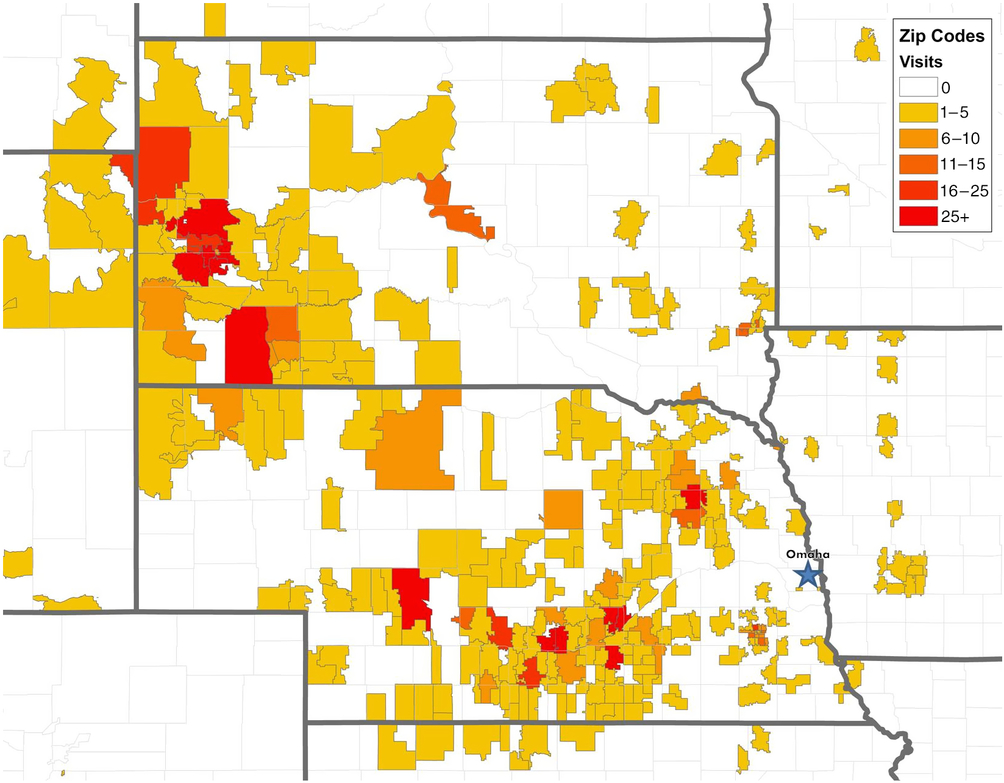
Figure 3. Number of Children’s Hospital and Medical Center paediatric cardiology outreach patient visits per zip code from, June 2017 to June 2018.
Our study shows the addition of eFCU improved outreach clinic throughput by an average of 3.5 additional patients per clinic. Extrapolating these data to include all of our outreach clinics, FCU offers the potential to reach approximately 350 additional patient encounters each year. Although quantitation of the benefit of this in terms of resource utilisation is beyond the scope of this investigation, the potential for increased economy of care in the outreach clinic setting (travel expense, physician time, and cost of testing) appears substantial. Moreover, quality of the patient and family experience is likely impacted favourably by reducing wait times for outreach clinic appointments and/or by reducing the need to travel long distances to the tertiary centre for care. The provider, patient, and family may also benefit from real-time, face-to-face visually supported patient/family-centred educational discussion of eFCU findings. The results of our survey support this contention. The importance of patient satisfaction of a healthcare encounter has become increasingly recognised. A recent systematic review found that providers’ interpersonal skills were strongly associated with patient satisfaction. Reference Batbaatar, Dorjdagva, Luvsannyam, Savino and Amenta15 A provider’s interaction with the patient and family during eFCU has the potential to further enhance the interpersonal connection that families desire during a clinic visit and therefore improve patient satisfaction.
The goal of the study was to evaluate the utility of eFCU in clinic settings with limited echocardiographic resources. The study was not intended to evaluate the accuracy of eFCU as several other studies have demonstrated its reliability. Reference Li, Mack and Rusk1,Reference Riley, Sable and Prasad7,Reference Kini, Mehta and Mazurek8 It is important to recognise that the American Society of Echocardiography recommends that any patient with abnormal findings on FCU that were not previously demonstrated on echocardiography should be referred for a complete echocardiogram. Reference Spencer, Kimura, Korcarz, Pellikka, Rahko and Siegel5 For this reason, we emphasise that eFCU is a useful instrument for follow-up in patients with known, relatively uncomplicated CHD. We recommend ongoing surveillance with complete echocardiography at a minimum of every other visit and prior to surgical planning or when making significant changes to medical therapy. Extrapolation of the results of this study to support the application of eFCU beyond this limited population is not advised without further investigation.
Focused cardiac ultrasound cannot substitute for an echocardiogram or history and physical exam, but can serve as an additional tool in making a clinical assessment. This was demonstrated in our patient who underwent eFCU for evaluation of a previously noted patent ductus arteriosus. Expert focused cardiac ultrasound, when combined with clinical assessment, led to the correct choice of de novo complete echocardiography for re-evaluation of the working diagnosis.
There are limitations to this study. The patients in this investigation were carefully selected to represent a limited spectrum of simple CHD, so the conclusions cannot be extended with confidence to apply eFCU to more complex clinical situations. The accuracy of FCU is dependent on the users’ training in acquisition, analysis, and interpretation. Reference Spencer, Kimura, Korcarz, Pellikka, Rahko and Siegel5 In this study, the primary scanner was an expert in echocardiography with many years of experience. Therefore, our results cannot be extrapolated to infer the utility of eFCU when used by minimally trained providers. In addition, while the physicians were confident with the images obtained, the studies were not over-read by a second echocardiographer to ensure accuracy. The study population in a central Nebraska paediatric cardiology clinic may or may not share key characteristics with other cardiology outreach programmes, and some differences may be relevant to the anticipated success of eFCU. For instance, an outreach clinic providing mostly new cardiac evaluations for previously undiagnosed patients would not necessarily be a good fit with eFCU as applied in this study. Finally, the focus of this investigation was not to validate the accuracy of the imaging against the standard of more classic complete echocardiogram, as other investigators have previously done this, but is limited to a determination of whether or not key data relevant to the established diagnoses can be reliably acquired with eFCU.
Focused cardiac ultrasound successfully identified the features outlined in our novel assessment tool in established patients with atrial septal defect, ventricular septal defect, atrioventricular septal defect, pulmonary stenosis, aortic stenosis, and patent ductus arteriosus. The addition of eFCU in outreach clinics improves productivity by permitting more patients to be seen in 1 day, benefiting both the physician and the family. Patients and families had a positive response to eFCU.
Acknowledgements
We gratefully acknowledge Fujifilm Sonosite, Inc. for use of the equipment. The authors also would like to thank Drs Robert L. Spicer, John D. Kugler, Angela T. Yetman, Hao H. Hsu, and Christopher L. Shaffer for their helpful suggestions.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
The authors have no conflicts of interest relevant to this article to disclose.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the University of Nebraska institutional review board and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the University of Nebraska Medical Center institutional review board.
Disclosure
The authors have no financial relationships relevant to this article to disclose.








