Introduction
Autoinflation devices are commonly used for otitis media with effusion (OME) and Eustachian tube dysfunction in the otolaryngology out-patient setting and in general practice. The Politzer method of passive middle-ear pressurisation, by initially hand-held and then electrical devices (Ear Popper; Summit Medical, St Paul, Minnesota, USA), has been used for over a century.Reference Blanshard, Maw and Bawden1 Active methods, as originally proposed by Valsalva in the eighteenth century, were adjusted with the addition of a balloon by Stangerup et al. in the 1990s.Reference Stangerup, Sederberg-Olsen and Balle2 They created a device (Otovent; Abigo Medical, Askim, Sweden) with a natural latex balloon that is actively inflated via a plastic nosepiece using the Valsalva manoeuvre. This produces a defined pressure (600 mm of water) in the nasopharynx, which thus applies pressure to the Eustachian tube. On release, the air from the balloon is pushed back into the nasopharynx for a passive insufflation. Combined active and passive actions aim to enable recovery of normal middle-ear pressurisation. Generally, these involve very safe devices, with few or no complications.3
A 2013 Cochrane review found evidence to indicate that autoinflation device use in children with OME is ‘favourable’, and this has become a widely accepted practice in both adults and children.Reference Perera, Glasziou, Heneghan, McLellan and Williamson4
We present the case of an episode of pneumocephalus and orbital emphysema associated with autoinflation device use in an adult with OME and Eustachian tube dysfunction symptoms, who had previously undergone endoscopic sinus surgery.
Case report
A 73-year-old woman attended the otolaryngology out-patient department in late 2016. She had a three-month history of symptoms in keeping with Eustachian tube dysfunction and right-sided otitis media with effusion following an upper respiratory tract infection. She had previously undergone endoscopic sinus surgery, in 2003, for chronic rhinosinusitis with nasal polyposis. At that time, she underwent septoplasty, bilateral uncinectomies, middle meatal antrostomies, and anterior and posterior ethmoidectomies. She was observed to have widespread polypoidal disease, but no record was made of any concern regarding the procedure. Indeed, her symptoms had been well controlled with medical therapy, and she had experienced no problems for 13 years.
On examination, an effusion was present in the right ear. She had a type B tympanogram and asymmetrical mixed hearing loss on audiometry. Fibre-optic nasendoscopy and post-nasal space examination findings were normal. She was advised to try an Otovent autoinflation device, and was prescribed nasal decongestant and intra-nasal steroid spray.
Several weeks later, she presented to the emergency department with a headache, throbbing in nature and retro-orbital, with an element of photophobia and nausea. This had developed immediately after performing her morning autoinflation routine. Neurological and physical examination findings were normal. An urgent computed tomography (CT) scan of her head was performed. This showed a small locule of gas within the right orbit (Figure 1), and tiny locules of gas within: the basal cisterns (Figure 2), posterior to the clinoid process on the left (Figure 3) and posterior to the left sphenoid sinus adjacent to the left internal carotid artery (Figure 4). There was mild inflammation of the ethmoid sinuses, but no evidence of any bony dehiscence. Fibre-optic nasendoscopy was performed, which showed the post-operative anatomical changes, but no cerebrospinal fluid leak or any sign of rhinosinusitis. Routine blood test results were unremarkable.

Fig. 1. Axial computed tomography image showing orbital emphysema (arrow).

Fig. 2. Axial computed tomography image showing a locule of gas within the basal cisterns (arrow).
Fig. 3. Axial computed tomography image showing a locule of gas posterior to the clinoid process on the left (arrow).

Fig. 4. Axial computed tomography image showing a locule of gas posterior to the left sphenoid sinus adjacent to the left internal carotid artery (arrow).
The images were reviewed by the local tertiary referral neurosurgical centre and a conservative approach was adopted. The patient was admitted and treated with a pneumococcal vaccine, broad-spectrum antibiotics and analgesics. Her symptoms improved with 48 hours. A further CT scan was performed 3 days later, which showed resolution of the pneumocephalus and orbital emphysema, and again there was no evidence of any bony dehiscence. She was discharged with a complete course of antibiotics.
Subsequent follow up in the otolaryngology out-patient clinic six weeks later revealed no residual symptoms and normal endoscopic examination findings.
Literature review
A systematic literature search was performed using Embase (1980 to November 2017), Medline (1946 to November 2017) and the Cumulative Index of Nursing and Allied Health Literature (1981 to November 2017). The literature search was performed using the Medical Subject Heading search terms: ‘otitis media with effusion’, ‘secretory otitis media’ and ‘Eustachian tube’, together with ‘autoinflation’ or ‘Otovent’. Further searches were performed using these results with the terms ‘complications’ or ‘pneumocephalus’.
Initially, 13 articles were identified from the database searches. A process of reference reduction was independently undertaken by the authors. The reference sections of all original articles were searched to identify other potentially relevant articles. The process undertaken is schematically presented in Figure 5.
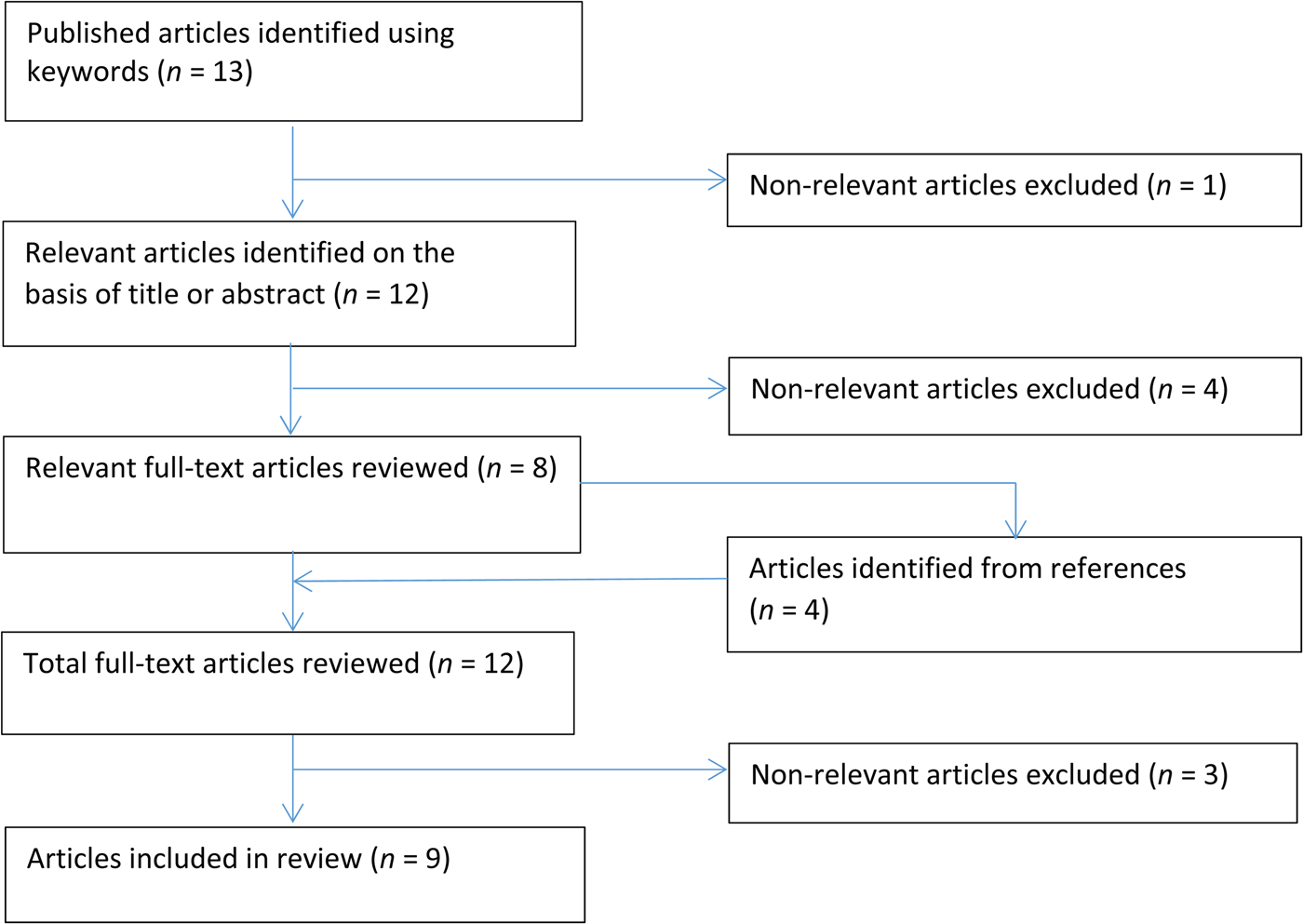
Fig. 5. Flow chart of systematic search and review process conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (‘PRISMA’).
A total of nine articles were ultimately identified, with no disagreement between the authors during the process of reference reduction.
Discussion
The literature review found no previous description of any serious side effect or complication due to use of the Otovent autoinflation device, including National Institute for Health and Care Excellence and Cochrane reviews.3, Reference Perera, Glasziou, Heneghan, McLellan and Williamson4 Non-serious adverse incidents might include epistaxis, acute otitis media or otalgia, but no statistical difference was found between control and treatment arms in trials.Reference Williamson, Vennik, Harnden, Voysey, Perera and Kelly5
Two cases were found of pneumocephalus relating to the Valsalva manoeuvre, in the absence of an autoinflation device. Firstly, Nakazawa et al. described a case of a young man who had been regularly using the Valsalva manoeuvre and, on presentation with left-sided ear symptoms, was found to have an external auditory canal obstructed by skin ballooning caused by subdermal air.Reference Nakazawa, Watanabe, Oyama, Takahashi and Murakami6 A subsequent CT scan showed pneumocephalus in the extradural space of the posterior fossa and subdermal space of the external auditory canal. A pathological bony defect around the sigmoid sinus was found at mastoidectomy.Reference Nakazawa, Watanabe, Oyama, Takahashi and Murakami6 Secondly, Nyrop et al. presented a patient with a habit of frequent Valsalva manoeuvres and a spontaneous pneumocephalus.Reference Nyrop, Bjerre, Christensen and Jørgensen7
Other case reports were found in which a pathological state in combination with the use of the Valsalva manoeuvre and Eustachian tube catheterisation led to pneumocephalus. Nishikori et al. described a case of a patient with a metastatic ocular deposit, and a history of Valsalva manoeuvre use and Eustachian tube catheterisation, who presented with diplopia and proptosis, and who was found to have extensive orbital emphysema and pneumocephalus.Reference Nishikiori, Akatsuka, Tabuchi, Yamashita and Akisada8 Ishiguro described a patient with a history of craniotomy for meningioma in the left middle fossa, who was subsequently treated with Eustachian tube catheterisation for secretory otitis media, and who developed pneumocephalus.Reference Ishiguro9
• Autoinflation is often recommended for otitis media with effusion and Eustachian tube dysfunction, with few complications or side effects
• The Otovent balloon uses active and passive pressures of up to 600 mm of water to the post-nasal space and Eustachian tube, to facilitate symptom improvement
• This paper describes the first case of pneumocephalus associated with Otovent use, in a patient with a history of sinus surgery
• Caution should be exercised when recommending autoinflation device use to previous sinus surgery patients given the risk of bony defects or weaknesses
In summary, all previous examples of pneumocephalus associated with middle-ear insufflation occurred in the context of a pathological skull base defect or a history of surgical intervention. Our patient had previously undergone endoscopic sinus surgery, but that was some 13 years previously. Hence, theoretically, the patient could have had an undetected breach in the sinus bony cavity, perhaps in the lamina papyracea.
Autoinflation device use is regularly advised for patients visiting the otolaryngology out-patient department, most usually the Otovent device. The devices are most commonly used for otitis media with effusion (OME), but Eustachian tube dysfunction research has become an expanding field. The evidence to date is strongest in children with OME,Reference Stangerup, Sederberg-Olsen and Balle2 but adults are often advised to use an autoinflation device; indeed, it is marketed to treat barotitis associated with air travel.10
In the UK, around 10 500 people undergo some form of sinus surgery per year.11 Given the cumulative population, it is likely that practitioners will encounter patients with Eustachian tube dysfunction or OME and a history of previous functional endoscopic sinus surgery, and may well consider recommending an autoinflation device. We suggest that autoinflation devices are used cautiously in patients with a history of sinus surgery.
Conclusion
This is the first description of pneumocephalus associated with use of an autoinflation device for otitis media with effusion or Eustachian tube dysfunction. Generally speaking, autoinflation devices are used widely with little or no complications or side effects, and are very safe. We suggest, however, that care should be taken in patients who have undergone endoscopic sinus surgery. In this patient group, the sinonasal anatomy has been altered, and there is a theoretical risk of undetected bony defects or weaknesses. The available case studies suggest that patients with the potential for bony breaches are most at risk.
Acknowledgement
The authors would like to thank Janet Bayliss of the Ipswich Hospital Library for her help in the preparation of the literature search.
Competing interests
None declared







