Introduction
Binder's syndrome or maxillonasal dysplasia is a rare congenital malformation characterised by flattening of the facial profile due to under-development of the midfacial skeleton.Reference Olow-Nordenram, Sjöberg and Thilander1 The condition has a range of severity and expression, but its characteristic features are a retruded midface, a flat nose tip and alae, crescent-shaped nostrils, short columella, an absent or short anterior nasal spine, a convex upper lip, and a poorly developed broad philtrum,Reference Draf, Bockmühl and Hoffmann2,Reference Holmström3 with a fossa-like deep fold between the upper lip and base of the nose.Reference Delaire, Tessier, Tulasne and Resche4,Reference Ferguson and Thompson5 The maxilla lacks normal anteroposterior growth and is attached to a short anterior cranial base, resulting in maxillary retrusion.Reference Olow-Nordenram, Sjöberg and Thilander1,Reference Horswell, Holmes, Levant and Barnett6 Maxillary hypoplasia also leads to relative prognathism and, in severe cases, type III dental malocclusion.Reference Olow-Nordenram, Sjöberg and Thilander1,Reference Holmström3 Before the classical description by Binder in 1962,Reference Binder7 it was described as ‘dish face deformity’ by Coughlin (1925) and Ragnell (1952).Reference Coughlin8,Reference Ragnell9 Binder described six specific features in his report on three unrelated children: an arhinoid face, intermaxillary hypoplasia, an abnormal position of nasal bones, atrophy of nasal mucosa, reduced or absent anterior nasal spine, and absence of a frontal sinus (not obligatory).Reference Binder7
Its aetiology is unclear, with Noyes proposing that it results from birth traumaReference Noyes10 and Hopkin concluding it to be a result of developmental insult.Reference Hopkin11 Binder considered the defect a form of arhinocephalic malformation,Reference Binder7 whereas Holmström proposed an inhibition of the ossification centre that would normally form the lateral and inferior borders of the pyriform aperture during the fifth to sixth gestational week.Reference Holmström3 The majority of cases are sporadic, although there may be some role of hereditary factors, as familial occurrences are reported to range from 16 per centReference Holmström3,Reference Roy-Doray, Geraudel, Alembik and Stoll12 to 36 per cent.Reference Olow-Nordenram and Valentin13 It may be a result of autosomal recessive inheritance with incomplete penetrance, or genetically multifactorial inheritance with environmental influences.Reference Olow-Nordenram and Valentin13,Reference Gorlin and Pindborg14 There may also be associated cleft palate or vertebral abnormalities. There is no gender predilection, and males and females are equally affected.Reference Draf, Bockmühl and Hoffmann2,Reference Olow-Nordenram and Valentin13
Treatment suggestions over the years have included bone and cartilage grafts,Reference Draf, Bockmühl and Hoffmann2,Reference Ragnell9,Reference Converse15–Reference Bhatt, Vyas, Tandale, Panse, Bakshi and Srivastava18 Silastic™ grafts to the nose and maxilla,Reference Sajjadian, Naghshineh and Rubinstein19–Reference Holmes, Lee, Greensmith, Heggie and Meara22 naso-orbito-maxillary advancements,Reference Converse, Horowitz, Valauri and Montandon16 LeFort I and II osteotomies,Reference Converse, Horowitz, Valauri and Montandon16,Reference Obwegeser17,Reference Henderson and Jackson21 nasal septal advancements,Reference Holmström and Gewalli23 and various techniques to lengthen the columella.Reference Hopkin11,Reference Holmström24,Reference Dingman and Walter25 Most recent authors believe that the majority of cases do not require LeFort osteotomies, and orthodontic treatment is usually sufficient as a conjunct to nasal surgery.Reference Draf, Bockmühl and Hoffmann2,Reference Holmström24,Reference Losken, Morris and Uys26,Reference Jackson, Moos and Sharpe27 However, there is still controversy regarding the optimal age for surgery, and the most appropriate procedure for achieving long-term favourable functional and aesthetic outcomes.
This study, with a level of evidence of 4 (case series), reports our experience with five children having Binder's syndrome nose deformity, who were operated on in childhood or early adolescence. It examines their outcomes from the patients’ and surgeon's perspective, and assesses whether early surgical intervention is favourable to the child's facial aesthetic and psychological growth. Binder's syndrome being a rare condition, our series of five cases, all with similar approaches and management protocols, could be of value when applied to Binder's syndrome patients of a similar age group.
Materials and methods
Our series includes five patients who presented with Binder's syndrome at our tertiary care centre. Two female patients, aged 8 years and 13 years, and one male patient, aged 13 years, underwent primary procedures. Another female patient, aged 15 years, had undergone primary augmentation rhinoplasty elsewhere, at the age of 6 years. The fifth patient, a 12-year-old female, had undergone primary rhinoplasty at age 9 years.
Their diagnosis was based on characteristic clinical features. No functional complaints were reported. A diagnostic nasal endoscopy was performed for each patient pre-operatively, which revealed no other abnormality. None of the patients had significant dental malocclusion.
All the patients and parents were well counselled regarding: their condition, available options for surgery with their advantages and disadvantages, limitations, possible complications, and expected outcomes. All were keen to undergo surgery. Written informed consent was obtained from both the parents and the patients. Consent was also obtained for the possibility of secondary augmentation surgery at an older age if needed. As this is a retrospective review of the surgical techniques employed, there was no need for Institutional Review Board approval. All procedures conform to the standards of the Declaration of Helsinki.
Open rhinoplasty approach was used for four patients, as our preferred approach. Closed rhinoplasty was performed in one patient, who had a very thin and delicate columella and had previously undergone a primary procedure by the sublabial approach. The surgical procedures performed were tailored to each individual patient and their specific requirements.
All patients were followed up at one, three and six months, and at one year, after surgery. Further follow-up data were available for three patients for 2 years post-surgery and for two patients for 1.5 years post-surgery. Pre- and post-operative photographic documentation of the patients was obtained.
Feedback was recorded in terms of overall satisfaction with the surgery and aesthetic outcome, and the psychological and social benefits, based on subjective patient and parent interviews, and was quantified using the Rhinoplasty Outcome Evaluation questionnaire.
Patients and surgical techniques
Case one
A 15-year-old girl (Figure 1) had undergone primary surgery at the age of 6 years by another surgeon, who used silicone implants for augmentation of the dorsum and tip. We observed slight irregularity of the dorsum and flattened dorsum and tip, with retracted, barely visible columella. The patient was a college student and was very conscious about her appearance.
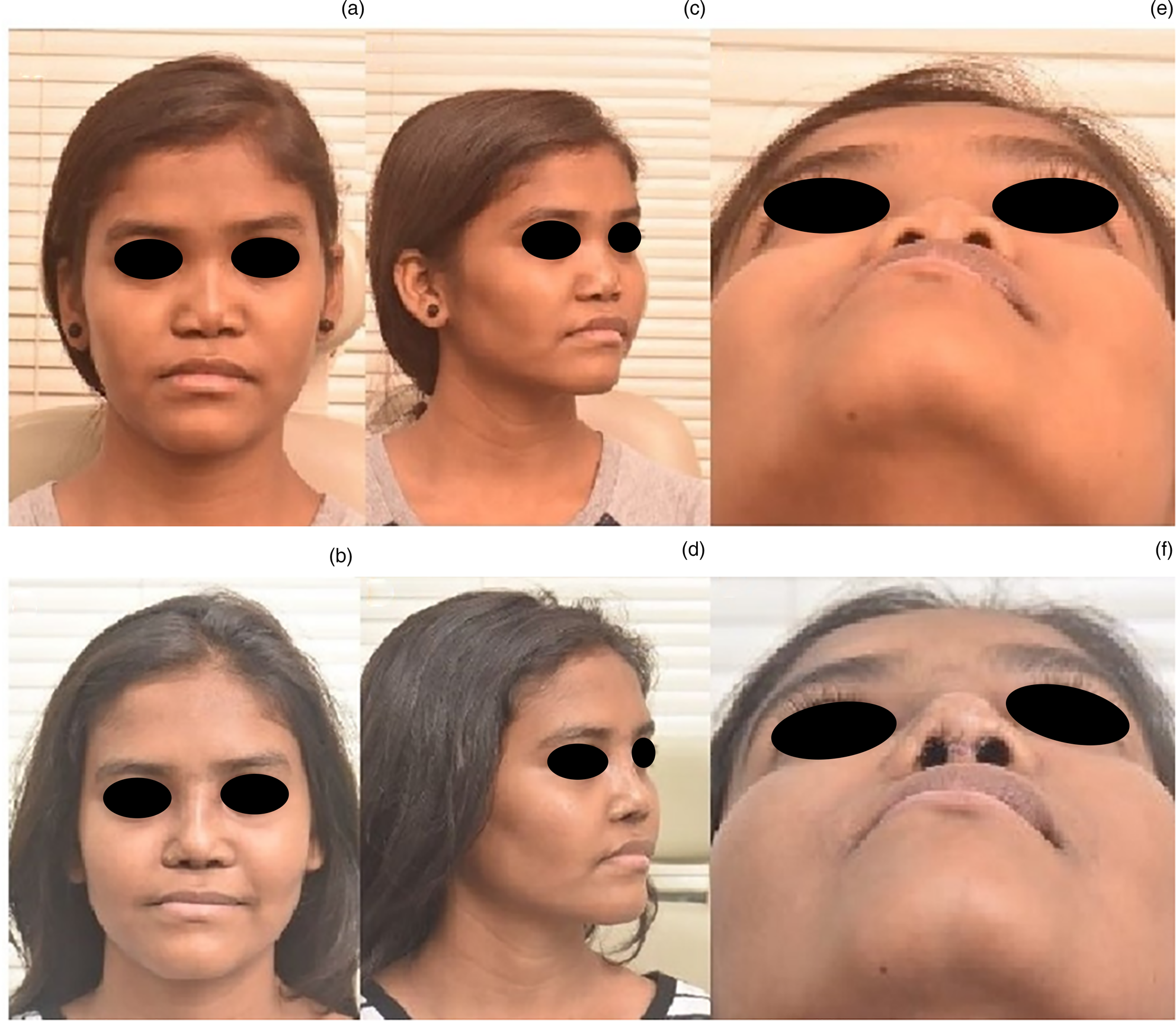
Fig. 1. Comparative pre- and post-operative photographs of a revision case at two years’ follow up: (a) pre-operative frontal view; (b) post-operative frontal view; (c) pre-operative left oblique view; (d) post-operative left oblique view; (e) pre-operative basal view; and (f) post-operative basal view. Published with patient's permission.
Using the open rhinoplasty approach, gaining adequate exposure, two silicone implants were visualised: a straight piece for the dorsum and an L-shaped strut for the tip-columella. We removed both implants. We found that the skin and mucosa were adequately lax after implant removal, allowing tension-free augmentation. We used a two-layered strip of conchal cartilage for augmentation of the dorsum, cartilage wrapped in temporalis fascia for the radix, and an L-shaped strut of costal cartilage for the tip-columella. Bilateral osteotomies were performed to narrow the nasal pyramid.
The patient was happy with the improvement and less conscious of her appearance. It boosted her self-esteem, and her social interactions and academic performance improved. Satisfactory augmentation was possible because of the adequate dorsal skin pocket achieved as a result of the dorsal implant placed in childhood rhinoplasty, emphasising the importance of early intervention.
Case two
This was an eight-year-old girl with Binder's syndrome (Figure 2). We used the open rhinoplasty approach with an L-shaped frame of costal cartilage for the tip, a costal cartilage onlay for dorsum augmentation, strips for the lateral wall, a columella strut from the central section of a rib cartilage graft fixed between the two medial crura over the anterior nasal spine for nasal tip projection, a small shield graft for tip definition, and sublabial conchal onlay grafts for nasal base enhancement.

Fig. 2. Comparative pre- and post-operative photographs of a primary case at two years’ follow up: (a) pre-operative frontal view; (b) post-operative frontal view; (c) pre-operative right oblique view; (d) post-operative right oblique view; (e) pre-operative basal view; and (f) post-operative basal view. Published with patient's permission.
There was already marked improvement in dorsal height and tip projection. If the patient subsequently requires a secondary augmentation surgery, we will find adequately expanded skin and mucosa resulting from this primary augmentation at a young age, as in our previous experience.
Case three
Case three was 13-year-old girl (Figure 3) studying in 9th grade at school. She reportedly faced teasing and embarrassment at her boarding school, suffered from low self-esteem and depression, and had moved to another school. She was self-conscious about her nose and strongly wished to improve its appearance.

Fig. 3. Comparative pre- and post-operative photographs of a primary case at two years’ follow up: (a) pre-operative frontal view; (b) post-operative frontal view; (c) pre-operative left lateral view; (d) post-operative left lateral view; (e) pre-operative basal view; and (f) post-operative basal view. Published with patient's permission.
We used the open rhinoplasty approach, creating an adequate dorsal and lateral subperiosteal skin pocket. Septal cartilage was found to reach just short of the tip. We harvested conchal cartilage, and used it as a septal extension graft fixed from the caudal edge of the septum to the nasal spine, projecting upwards to the intended tip. Lateral crural steal was performed for narrowing the dome and tip projection, along with inter-domal sutures, bilateral osteotomies, and narrowing of the nasal pyramid. A shield cartilage graft was secured over the tip.
The patient was pleased with her appearance after surgery, and showed improved confidence at home, at school and socially.
Case four
This was a 12-year-old girl (Figure 4) studying in 8th grade at school. She had had a right alar deformity since birth. She underwent her first surgery aged nine years, when dorsal augmentation alone was performed with a costal cartilage graft from the sublabial approach by another surgeon. There was a mild dental overbite.

Fig. 4. Comparative pre- and post-operative photographs of a revision case at 1.5 years’ follow up: (a) pre-operative frontal view; (b) post-operative frontal view; (c) pre-operative right oblique view; (d) post-operative right oblique view; (e) pre-operative basal view; and (f) post-operative basal view. Published with patient's permission.
We performed a closed rhinoplasty, as her columella was very thin and delicate and the nostrils barely visible. We harvested bilateral conchal cartilages, and fashioned an L-shaped strut used as a septal extension graft for the tip-columella.
We layered strips of conchal cartilages for dorsal augmentation; these were covered in fascia to mask irregularities as her skin was thin. Bilateral alar rim grafts were used to support the weak and small alar cartilages. We also performed perinasal fat injections for nasal base augmentation.
This patient also successfully underwent orthodontic treatment for malalignment. She was happy with the result of the surgery.
Case five
Case five was a 13-year-old boy with Binder's syndrome (Figure 5) from a distant state in India. He was growing increasingly conscious of his looks with age and had become reclusive.

Fig. 5. Comparative pre- and post-operative photographs of a primary case at 1.5 years’ follow up: (a) on-table pre-operative right lateral view; (b) on-table post-operative right lateral view; (c) pre-operative frontal view; (d) post-operative frontal view; (e) pre-operative left lateral view; and (f) post-operative left lateral view. Published with patient's permission.
We performed an open rhinoplasty, using autologous rib cartilage as a septal extension graft for the tip-columella, along with thin central strips for dorsal onlay and bilateral alar rim grafts.
This patient, hailing from a distant town, was lost to follow up after 1.5 years. While the on-table result was satisfactory for the surgeon, the patient expressed discontent over the outcome, as he had had higher expectations. He had been well counselled about the limitations of the surgery and the need for a possible future second-stage surgery for the best possible results; however, he expected drastic changes in spite of the counselling. The young mind may have unrealistic expectations, and we would like to stress the importance of counselling every patient and family with this example.
Results
All five patients were operated on by us only once, by the same senior surgeon. Three patients underwent primary rhinoplasty, and two underwent secondary rhinoplasty, having been previously operated on elsewhere with dorsal onlay grafts at six and nine years of age, respectively.
Intra-operatively, we did not encounter tightness of overlying skin or underlying mucosa in any patient. We were able to comfortably undermine the soft tissue at the lip–columellar junction to release and lengthen the columellar skin from the hypoplastic floor in all the patients. No patient needed any additional lengthening procedures such as lip flaps or V–Y plasty.
In the follow-up period, which ranged from 1.5 to 2 years, no loss of cartilage volume, resorption or displacement was noted. All patients had acceptable nasal augmentation and tip projection, and adequate columellar lengthening was achieved.
There were no signs of infection or skin or columella necrosis due to compromised vascularity. None of the patients complained of nasal tip stiffness or graft show (under the skin). No functional complaints and no other surgery related complications were reported. The columellar scar was barely visible and was acceptable to the four patients who underwent open rhinoplasty.
Subjectively, the patients had an improved perspective about their self-image and were pleased with the aesthetic improvement, although the male patient had expected a more drastic change. We asked the patients to complete the Rhinoplasty Outcome Evaluation questionnaire to better quantify the subjective assessment. The Rhinoplasty Outcome Evaluation questionnaire consists of six questions, two for each factor considered important for patient satisfaction; namely, physical, social and emotional factors. All patients had a significant improvement in Rhinoplasty Outcome Evaluation scores, including the patient who had expected a better outcome (Table 1). Overall, the surgery had a positive psychological impact, and the patients reported feeling more confident and less self-conscious at school and at social gatherings.
Table 1. Comparison of pre- and post-operative Rhinoplasty Outcome Evaluation scores

Pt. no. = patient number; ROE = Rhinoplasty Outcome Evaluation questionnaire
Discussion
There is no consensus regarding the preferred surgical technique or the most appropriate age for surgery. As the condition is congenital, the deformities manifest at an early age and are evident from childhood.Reference Draf, Bockmühl and Hoffmann2,Reference Bhatt, Vyas, Tandale, Panse, Bakshi and Srivastava18 Epsteen (in 1958) and MacGregor (in 1970) reported that children with milder facial deformities, as compared with gross and severe ones, find it harder to cope psychologically.Reference Epsteen28,Reference MacGregor29 These children have low self-esteem, are anxious about people's reactions, especially those of the opposite sex in the teenage years, and are socially shy and withdrawn.Reference Lansdown, Lloyd and Hunter30 This leads some authors to advocate early surgical intervention.Reference Draf, Bockmühl and Hoffmann2,Reference Monasterio, Molina and McClintock31 Monasterio and colleagues also stated that an early intervention allows the corrected facial conditions to follow a pattern similar to normal growth.Reference Monasterio, Molina and McClintock31
Another school of thought suggested that an appropriate time for surgery would be after the completion of midfacial growth, which is usually after the mid-teens, as nasomaxillary hypoplasia is primarily a developmental anomaly.Reference Tessier, Tulasne, Delaire and Resche32–Reference Yamani, Ghosh and Tirunagari34 Blanket statements urging caution are common in the literature. However, studies have shown that surgery on the nose and septum in early life does not arrest growth of the nose and midface.Reference Ortiz-Monasterio and Olmedo35,Reference El-Hakim, Crysdale, Abdollel and Farkas36
We observed that an early intervention involving nasal and tip augmentation with or without pyriform augmentation, without performing any maxillary osteotomies, permitted reasonable expansion of skin and soft tissue covering with mucosal lining to grow progressively and normally with the midface. This was also mentioned by Monasterio and colleagues, who believed that the constriction of skin and mucosa in older patients posed a limitation to achieving an optimal result.Reference Monasterio, Molina and McClintock31 It is additionally advantageous if the patient at a later age desires a secondary augmentation, ensuring adequate laxity of skin and mucosa. If this laxity is not adequately achieved we could encounter problems of graft resorption, graft show (through the skin), displacement, and skin necrosis due to compromised vascularity from a tight skin envelope. Tight mucosa would also limit augmentation of the nasal tipReference Monasterio, Molina and McClintock31 and result in an unduly upturned tip.
Four patients had normal dental occlusion and two had undergone orthodontic treatment. According to several studies,Reference Olow-Nordenram, Sjöberg and Thilander1,Reference Bhatt, Vyas, Tandale, Panse, Bakshi and Srivastava18,Reference Carach, Woods and Scott37 changes in most cephalometric variables in maxillary growth parallel those of normal children as they approach adolescence and adulthood, and ‘catch-up’ growth occurs. Given the compensatory proclination of the maxillary incisors,Reference Olow-Nordenram, Sjöberg and Thilander1,Reference Tessier, Tulasne, Delaire and Resche32,Reference Munro, Sinclair and Rudd38 acceptable dental occlusion is achieved in most cases despite mandibular growth exceeding maxillary growth. Orthodontic treatment alone is sufficient in most cases, as the majority have normal or mild malocclusion. In rare scenarios, the patient has class III malocclusion at presentation and would require LeFort I osteotomy.Reference Draf, Bockmühl and Hoffmann2,Reference Posnick and Tompson39 We performed augmentation of perinasal and alar base regions with cartilage chips and fat injections, and achieved improvement of the midfacial profile while avoiding the risks of osteotomies in children, in accordance with the practice and findings of Goh and ChenReference Goh and Chen33 and Watanabe and Matsuo.Reference Watanabe and Matsuo40
The degree of deformity varies in each patient; thus, the appropriate surgery is tailored to their individual requirements, and no standard technique is described, although there are various proposed methods. Historically, bone grafts from the skull and iliac crest were used for augmenting the dorsum and columella, and L-shaped struts and cantilevers were used for nasal support.Reference Coughlin8,Reference Converse, Horowitz, Valauri and Montandon16,Reference Holmström24,Reference Rune and Aberg41,Reference Losken and Morris42 However, it was observed that bone grafts had unpredictable outcomes, including loss of volume, resorption, remodelling (especially with a tight skin covering), nasal tip stiffness and rigidity, which many patients found bothersome, and L-shaped struts were prone to fracture.Reference Holmström and Gewalli23,Reference Holmström24,Reference Monasterio, Molina and McClintock31,Reference Posnick and Tompson39,Reference Rune and Aberg41 Pain at the donor site, especially the iliac crest, was long-lasting with a protracted recovery period.Reference Bhatt, Vyas, Tandale, Panse, Bakshi and Srivastava18
• Binder's syndrome (maxillonasal dysplasia) is a rare congenital entity characterised by midface flattening due to under-development
• There is lack of consensus in the literature about the ideal age and technique for surgery
• A series of five cases are reported; all underwent primary augmentation rhinoplasty at an early age, two also underwent secondary augmentation
• By intervening at a younger age, augmentation of dorsum and nasal tip was easy and unrestricted because of laxity of skin and mucosa
• Further, this primary intervention allowed skin and mucosa to grow with the augmented nose, creating adequate pockets without tension during surgery
• Autologous cartilage gave stable results without complications, and all children reported improved confidence and self-perception
Many authors have also employed alloplastic implants for augmentation and expansion of the soft tissue envelope.Reference Holmes, Lee, Greensmith, Heggie and Meara22,Reference Goh and Chen33,Reference Horswell, Holmes, Barnett and Levant43 However, Silastic implants are associated with complications of chronic inflammation, infection and extrusion,Reference Vuyk and Adamson44–Reference Tian, You, Wang, Zhang, Xu and Lu46 with extrusion rates as high as 10 per cent for dorsal placement to 50 per cent for columellar placement according to one study.Reference Staffel and Shockley45 These patients with a constricted skin envelope are at particular risk of extrusion because of pressure on the tight skin by the unyielding implant, especially in the columella.Reference Lansdown, Lloyd and Hunter30 It also entails a higher cost.
Cartilage grafts have been found to be nearly ideal as implantation material in rhinoplasty.Reference Draf, Bockmühl and Hoffmann2,Reference Monasterio, Molina and McClintock31,Reference Porter47 They are non-immunogenic and hence have no complications of immune reaction or extrusion;Reference Vuyk and Adamson44 they tend to maintain volume and cause less stiffness of the dorsum, with a softer more natural-feeling tip;Reference Draf, Bockmühl and Hoffmann2,Reference Monasterio, Molina and McClintock31,Reference Goh and Chen33 and they are known to be pliable when they need to be moulded, and yet are resilient enough for firm support and contouring.Reference Collawn, Fix, Moore and Vasconez48,Reference Tardy, Denneny and Fritsch49 Unlike bone, they need not be placed in direct contact with bone or cartilage, and unlike alloplasts, they need not be buried deep within soft tissue.Reference Tardy, Denneny and Fritsch49 Moreover, in children, cartilage grafts have shown neochondrogenic potential, and grow as the host organ grows.Reference Tardy, Denneny and Fritsch49–Reference Brent51
We exclusively used autologous cartilage grafts from the rib, concha and septum, with none of the abovementioned complications such as graft infection, resorption, displacement, graft show, or donor site pain or deformity. We used them in a versatile number of ways, as strips, L-shaped struts, or crushed or diced chips, tailored to each patient's requirements. Costal cartilage grafts have been known to undergo variable warping,Reference Fry52,Reference Gibson and Davis53 but using Gibson's principle of balanced cross-section,Reference Gibson and Davis53 we used a central slice of harvested cartilage, prepared in 0.9 per cent sodium chloride prior to fixation. We even used conchal cartilage exclusively to make an L-shaped strut in one patient; this patient had previously already received a costal cartilage graft by another surgeon, and found that it gave a stable support with a good long-term result.
We did not use any columella lengthening procedures like V–Y plasty or lip flaps.Reference Hopkin11,Reference Dingman and Walter25,Reference Jackson, Moos and Sharpe27 Furthermore, sufficient length was achieved by undermining the skin and soft tissue at the lip–columellar junction, which merely retracts into the hypoplastic nasal floor.Reference Holmström24,Reference Tessier, Tulasne, Delaire and Resche32
Ultimately, Lefebvre and Munro noted that post-operative satisfaction among the children was very high, and they showed increased enthusiasm, social activities, self-confidence, and assertiveness with strangers.Reference Lefebvre and Munro54 These patients and their families, if well counselled at the outset, are more accepting of a secondary surgical procedure to enhance the appearance after completion of the growth spurt; thus, long-term follow up is important.
Conclusion
We would like to emphasise that early intervention in Binder's syndrome has advantages for both the patient and the surgeon. Early surgery allows graft placement and augmentation without skin tension, reducing the chances of resorption or graft show (through the skin), because of supple skin and mucosa. It also allows ease of expansion of skin and mucosa with midfacial growth, making a secondary augmentation surgery less challenging for the surgeon. However, the patient and caregivers must be counselled regarding the possibility of a second-stage procedure, after the adolescent growth spurt is complete, for the best possible aesthetic outcome. The use of autologous cartilage grafts from the septum, concha and rib yields good and stable results, without the complications of silicone grafts or bone grafts; however, a longer follow-up period would be ideal.
For the growing child struggling with self-image at an impressionable age, early correction makes them less socially shy and conscious about their appearance, improves self-esteem, and can be of psychological and developmental benefit to the patient.
Acknowledgements
We would like to thank our patients and their guardians for their consent to share their photographs for publication and the betterment of science.
Competing interests
None declared








