The Great East Japan Earthquake [GEJE] occurred at 14:46 on March 11, 2011 (Japanese Standard Time). At a magnitude of 9.0, it was the fourth largest earthquake in the world since 1900. 1 A tsunami, with an estimated maximum height of 37.9 m from sea level, struck the Pacific coast of East Japan immediately after the earthquake and caused devastating damage.Reference Nagamatsu, Maekawa, Ujike, Hashimoto and Fuke 2 , Reference Satomi 3 On February 10, 2014, the human cost of the GEJE totaled 15 884 deaths and 2636 missing persons. Of these, 9537 deaths and 1283 missing persons were in Miyagi Prefecture (population approximately 2.2 million). 4 Most of the victims (92.5%) drowned,Reference Nagamatsu, Maekawa, Ujike, Hashimoto and Fuke 2 and many people were exposed to cold seawater during the tsunami. However, the rescuers could not reach the coast because the tsunami warning remained in effect for 51 hours after the earthquake, 5 hindering rescue operations. The rescue operations started in the inland areas and gradually spread to the coastal areas. It took approximately 3 days before the rescue operation was started throughout Miyagi Prefecture.
Patients who suffered lethal or serious injuries were transported to emergency hospitals by ambulances or Japan Self-Defense Forces helicopters. Patients who were alert and had no abnormal vital signs either walked to hospitals, if possible, or were transported to nearby hospitals by ambulance. In Japan, hospitals are legally defined as medical institutions with 20 or more beds, and clinics are those with less than 20. Emergency facilities are classified into 3 levels based on resources, administration, staff, and education. Primary emergency facilities provide care for walk-in patients, secondary emergency facilities provide in-hospital care for acute illnesses and trauma, and tertiary emergency facilities (called emergency medical service centers 6 ) provide total care for critically ill and severely traumatized patients.Reference Ishida, Ohta, Katsurada and Sugimoto 7 , Reference Tanigawa and Tanaka 8 After the earthquake, 72 secondary and tertiary emergency hospitals in Miyagi Prefecture received injured patients.Reference Kudo, Furukawa and Nakagawa 9 These hospitals included 14 that were designated disaster base hospitals by the Ministry of Health, Labour and Welfare [MHLW] to provide disaster medicine. In particular, the emergency departments at hospitals on the Pacific coast saw a surge in the number of patients. At the time of the earthquake, the temperature in the city of Sendai, in Miyagi Prefecture, was 4.8ºC, and the water temperature along the Pacific coast of the Tohoku region was 5º to 10ºC. 5 The lowest temperature of the day in Kesennuma (the coastal area of Miyagi Prefecture) was −3.8ºC. 5 People who escaped from the tsunami had to live in shelters without heaters and fuel. Many people were thought to have developed hypothermia due to exposure to the cold environment (cold seawater and cold air).
Accidental hypothermia is generally defined as a core temperature of less than 35ºC.Reference Brown, Brugger, Boyd and Paal 10 - Reference Lloyd 12 The severity of accidental hypothermia is classified as mild (from 32ºC to <35ºC), moderate (from 28ºC to <32ºC), and severe (<28ºC).Reference Kempainen and Brunette 13 - Reference Epstein and Anna 15 Different treatment methods are used, depending on the patient’s temperature. Passive external rewarming, using a blanket to cover the patient’s body, is effective to treat mild hypothermia. For moderate to severe hypothermia, active external rewarming using electric devices, such as a fan humidifier and hyperthermic irrigation, is often used.Reference Epstein and Anna 15 In addition, the administration of warm fluids is recommended for treating hypothermia because it is a simple technique that lacks complications.Reference Howard and Bessen 11
On immersion in cold water, heat is conducted away from the human body rapidly. In fact, the thermal conductivity of water is approximately 20 to 30 times higher than that of air.Reference Howard and Bessen 11 , Reference Molnar 16 Approximately 50% of people exposed to water temperatures from 5ºC to 10ºC for 1 to 2 hours die.Reference Molnar 16 Therefore, it is assumed that victims of tsunami disasters in winter may suffer from accidental hypothermia. However, to our knowledge, no research to date has reported on hypothermia during tsunami disasters.
During a disaster, individual patients may be treated inadequately because the supply of medical resources available to treat a large number of patients is limited. We previously described the profound imbalance between supply and demand during the 72 hours immediately following the GEJE. The lifeline, logistics, and flow of human resources were almost completely shut down while the medical needs (incoming patients and establishing disaster response systems) reached their peak.Reference Nakagawa 17 , Reference Nakagawa, Furukawa and Konishi 18 Active external rewarming methods, typically used to treat accidental hypothermia, would be difficult to implement with a large influx of patients in the midst of social infrastructure breakdown. This difficulty was largely due to the limited availability of temperature control devices and the required electricity.
The objective of this survey was twofold. The first was to describe the characteristics of patients treated for hypothermia documented after the GEJE. The second was to evaluate the outcomes of hypothermic patients during the post-earthquake disruption of regional social infrastructure.
Methods
Approvals and Inclusion Criteria for Participating Institutions
Approval for these studies was obtained from the ethical review board of Tohoku University Graduate School of Medicine and conducted in accordance with the Japanese ethics guidelines for epidemiologic studies implemented by the MHLW. Each participating hospital was not required to obtain individual institutional review board approvals.
Questionnaires were sent to the 72 secondary or tertiary emergency hospitals in Miyagi Prefecture where the authors are affiliated. We requested that respondents provide only de-identified data from medical records, and we regarded their reply to the questionnaire as their consent to participate. The survey was registered in the University Hospital Medical Information Network Clinical Trials Registry 19 to make the outline and the results publicly available (trial number: UMIN000006709). This survey was administrated from November 1, 2011, to May 30, 2012.
Inclusion Criteria for Hypothermic Patients
This retrospective survey included patients who sought treatment within 72 hours of the GEJE (ie, March 11, 2011 at 2:46 pm to March 14, 2011, at 2:46 pm). Patients with a temperature of less than 36ºC, regardless of the method used to measure temperature, were admitted to the responding hospitals. This survey included patients with a temperature between 35ºC and less than 36ºC, which is not generally considered a state of accidental hypothermia. They were classified as potential hypothermia cases. These patients were included because (1) perioperative hypothermia is defined as a core temperature less than 36.0°CReference Forbes, Eskicioglu and Nathens 20 and (2) the restricted lifeline at hospitals might affect these patients’ outcome. In prospective randomized trials, even mild hypothermia (decrease in core temperature of approximately 2°C) causes severe complications including morbid myocardial outcomes, surgical wound infection, prolonged recovery and hospitalization, shivering, and thermal discomfort.Reference Rajagopalan, Mascha, Na and Sessler 21 , Reference Sessler 22 Therefore, we hypothesized that even very slight hypothermia (35°-35.9°C) might have some impact on the human body.
Variables
The questionnaire requested information about the patients meeting the inclusion criteria and the hospital. The patient-related information included the number of hypothermic patients meeting the inclusion criteria; patient demographics including age and sex; the time the patient arrived; the cause of hypothermia (ie, being struck by the tsunami or not); whether hypothermia developed indoors or outdoors; patient temperature on arrival; the site of temperature measurement; the rewarming method applied; complications; the duration of the patient’s hospitalization; and the patient outcome on discharge.
Respondents from the hospital were asked to classify the patient’s outcome as “no sequelae,” “able to live an independent life despite mild sequelae,” “requiring assistance,” or “death.” A simple classification scheme was chosen because requiring more detailed outcome classifications for a significant number of patients would have been difficult. Regarding the hospital itself, respondents were asked about the availability of the heating system immediately after the earthquake and, if it were disrupted, how long it took for heat to be restored. These measures were used to evaluate if the heating capacity at the hospital might have affected how hypothermic patients were treated.
Statistical Analysis
The patients with hypothermia were divided into 4 groups: potential hypothermia (temperature between 35ºC and <36ºC), mild hypothermia (temperature between 32ºC and <35ºC), moderate hypothermia (temperature between 28ºC and <32ºC), and severe hypothermia (temperature <28ºC) to compare the demographic data and outcomes. We also compared the causes of hypothermia and whether it developed indoors or outdoors between patients who sought treatment within the first 24 hours after the earthquake and those who arrived 24 to 72 hours after the earthquake.
The software GraphPad PRISM 5 for Mac OS (GraphPad Software Inc) and EZR version 1.11Reference Kanda 23 were used for statistical analysis. The Kruskal-Wallis test or extended Fisher exact test with Bonferroni correction was used to compare groups based on temperature. The Fisher exact test was used to compare the causes of hypothermia, where hypothermia developed, and patient outcomes according to the time that the patient arrived at the hospital. Statistical significance was accepted at P <.05.
Results
Of the 72 emergency hospitals, 64 (88.9%) in Miyagi Prefecture responded to the questionnaire, and 16 of the 64 hospitals provided data pertaining to the admission of hypothermic patients. Information was obtained for 134 patients. Incomplete information was provided for 43 patients, and they were subsequently excluded from the survey. A total of 91 patients from 13 hospitals were included in the analysis. The responding hospitals ranged in size from: 100 to 300 beds (N=5); 301 to 500 beds (N=5); 501 to 1000 beds (N=2); and more than 1000 beds (N=1). Most of the patients were classified as having potential (N=32) or mild hypothermia (N=45). However, a few moderate (N=8) and severe (N=6) cases of hypothermia were reported.
Temperature is not the same as core temperature. The axillary temperature was taken in many of the patients (54/91 patients), and chest skin temperature was taken in 1 patient. A core temperature reading was obtained in 23 patients by measuring the rectal temperature (N=12), tympanic membrane temperature (N=9), or bladder temperature (N=2). No information was provided about the site of the temperature measurement for 13 patients. One severe hypothermic patient experienced cardiopulmonary arrest (CPA) and the return of spontaneous circulation after arrival at hospital.
Institutional Availability of Working Heating Systems
Of the 13 hospitals where hypothermic patients were admitted, 7 hospitals had no usable heating system, 5 had partially functional heating, and only 1 institution had fully functional heating. The usable heating systems was restricted by a stoppage of the electricity or gas supply (N=7) and/or destruction of the heating system (N=6). In the 7 hospitals where the entire heating system was unusable, 1 institution was able to repair it the day of the earthquake, and 4 hospitals (57%) were able to repair the system within 3 days.
Patient Demographics
The mean age of the 91 patients was 61.3±22 years (mean±standard deviation). Forty-one patients were men and 50 were women. The patients’ medical history indicated no preexisting disorder in 45 patients, 18 patients with cardiovascular disease, 10 patients with cerebrovascular disease, 5 patients with respiratory disease, 4 patients with malignant tumor, 5 patients with diabetes mellitus, 2 patients with neuromuscular disease, and 10 patients with other preexisting conditions. Some patients were documented as having 2 or more preexisting disorders.
No significant difference was found in the mean age, duration of hospitalization, and hospital-free days to day 14 [HFD14]Reference Ali, O'Brien and Hoffmann 24 between patients based on the severity of hypothermia. The percentage of patients who were rated 8 or less on the Glasgow Coma Scale [GCS] was statistically higher in those classified as having severe hypothermia than in the potential and mild hypothermia groups (P=.01, .04, respectively, data not shown). The mortality rate in patients based on severity of hypothermia was 6.3% (2 patients) in the potential group, 2.2% (1 patient) in the mild group, 0% in the moderate group, and 16.7% (1 patient) in the severe group (Table).
Table Characteristics of Patients

Abbreviations: GCS, Glascow Coma Scale; HFD, hospital-free days to day 14; and SBP, systolic blood pressure.
a Age, length of stay, and HDF14 are presented as Mean ± standard deviation. HFD14 is the calculated value after subtracting the days of hospitalization from 14. When the value is less than zero or when a patient died during hospitalization, HFD was considered zero. The percentage of patients who scored ≤8 on the GCS was statistically different depending on hypothermia severity. It was higher in the patients with severe hypothermia than in those with potential hypothermia or mild hypothermia (P =.01,.04, respectively).
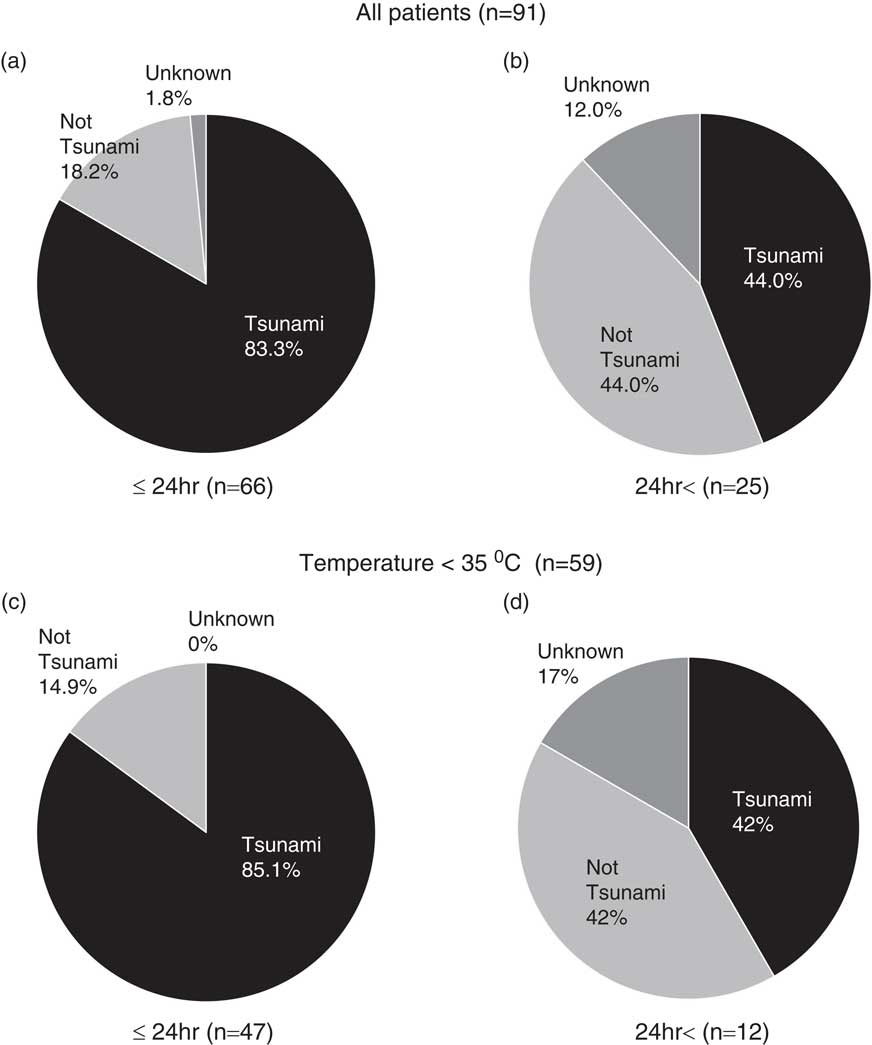
Time of Arrival at the Hospital
Within 24 hours of the earthquake, 66 of the 91 patients sought treatment. The patients included potential (N=19), mild (N=36), moderate (N=7), and severe (N=4) cases of hypothermia. The remaining 25 patients sought treatment between 24 and 72 hours after the earthquake. As with the earlier cases, these patients included potential (N=13), mild (N=9), moderate (N=1), and severe (N=2) cases of hypothermia (Figure 1).
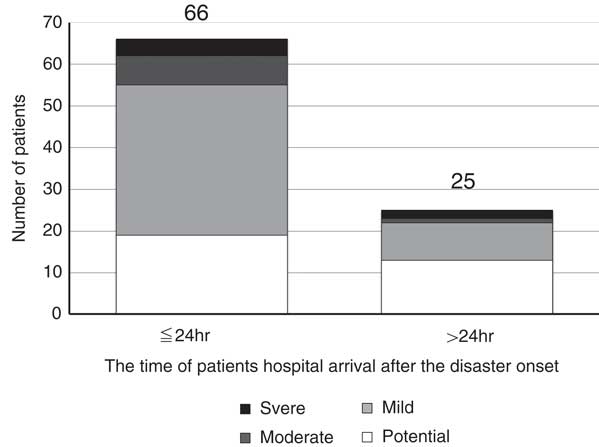
Figure 1 The Number of Patients and Severity of Hypothermia Within 72 Hours of the Earthquake. Patients were divided into 2 groups: those who arrived within 24 h of the earthquake and those who arrived later than 24 h. Many hypothermic patients arrived within 24 h.
Causes of Hypothermia and Where It Developed
We defined hypothermia caused by the tsunami as patients who reported being partially or completely submerged under the tsunami and exposed to cold seawater. Tsunami-related hypothermia was diagnosed in 66 of the 91 patients (72.5%). In 21 patients (23.1%) the cause of hypothermia was something other than the tsunami. In 4 patients (4.4%) the cause of hypothermia was unknown. Of the 21 patients whose hypothermia was caused by something other than the tsunami, in 2 patients the condition developed indoors; in 12 patients it developed outdoors, and in 7 patients the location was unknown. No preexisting disorders were identified in 3 of the patients; however, the remaining 18 patients had a preexisting disorder. These included cerebrovascular disorders (N=8) and 1 patient with a neuromuscular disorder. Five of 11 patients who arrived more than 24 hours after the earthquake had underlying cerebrovascular disorders.
Both in all patients and in those with a temperature of less than 35ºC (ie, patients who met the diagnostic criterion of accidental hypothermia), the percentage of patients with hypothermia caused by the tsunami was higher in those who sought treatment within 24 hours of the earthquake compared with those who sought treatment in 24 to 72 hours after the earthquake (83.3% vs 44.0% in all patients, P <.001, Figure 2A, 2B; 85.1% vs 42% in those with temperatures <35ºC, P=.002, Figure 2C, 2D). In the first 24 hours after the earthquake, 56% (N=37) of patients developed hypothermia outdoors, while only 35% (N=23) developed hypothermia indoors. In contrast, more than 24 hours after the earthquake, 76% of cases (N=19) were acquired indoors and only 16% (N=4) developed outdoors (Figure 3A, 3B). Both in all patients and in those with temperatures less than 35ºC, the percentage of patients who developed hypothermia outdoors was significantly higher within 24 hours of the earthquake than 24 to 72 hours after the earthquake (56% vs 16% in all patients, P=0.001, Figure 3A, 3B; 68% vs 17%, <35ºC, P=.002, Figure 3C, 3D).

Figure 2 Comparing the Causes of Hypothermia in Patients Seeking Treatment Within 72 Hours of the Earthquake. A, Causes of hypothermia in patients seeking treatment within 24 h of the earthquake (N=66). B, Causes of hypothermia in patients seeking treatment 24 to 72 hours after the earthquake (N=25). Percentage of patients with hypothermia caused by the tsunami was significantly higher in those seeking treatment within 24 h compared with those seeking treatment in 24 to 72 h after the earthquake (P<.001). C, Causes of hypothermia in patients with a temperature <35ºC (N=47) seeking treatment within 24 h of the earthquake. D, Causes of hypothermia in patients with a temperature <35ºC (N=12) seeking treatment 24 to 72 h after the earthquake. The percentage of patients seeking treatment within 24 h was significantly higher than those seeking treatment in 24 to 72 h after the earthquake (P=.002).
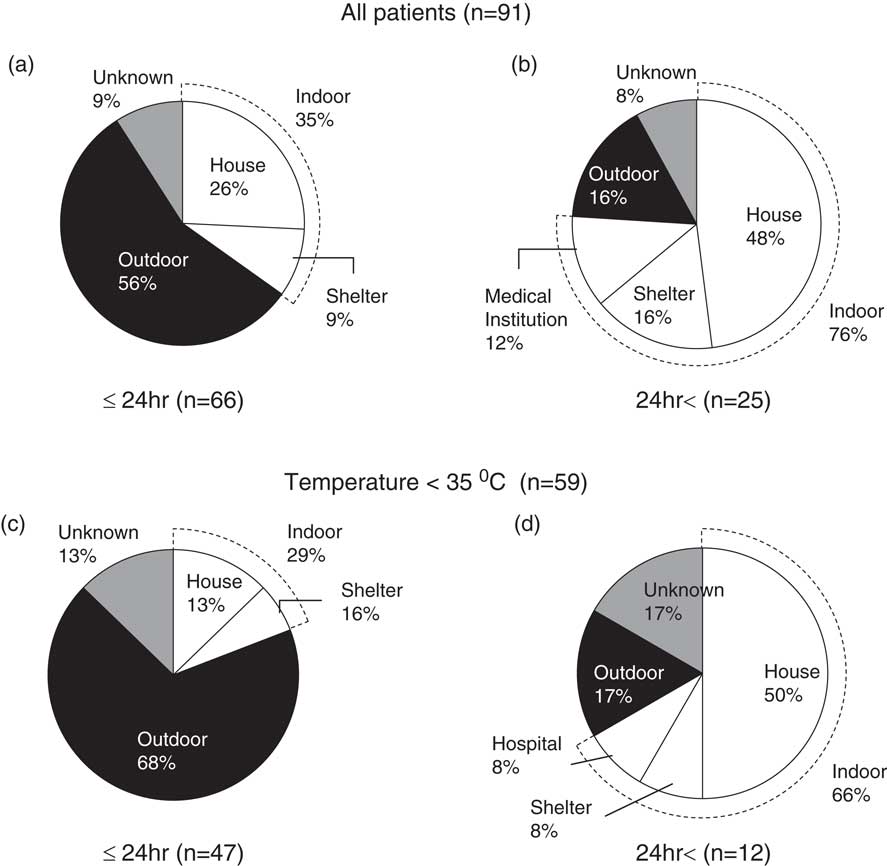
Figure 3 Comparing Where Hypothermia Developed in Patients Seeking Treatment Within 72 Hours of the Earthquake. A, Where hypothermia developed in patients seeking treatment within 24 h of the earthquake (N=66). B, Where hypothermia developed in patients seeking treatment 24 to 72 h after the earthquake (N=25). The percentage of patients who developed hypothermia outdoors was significantly higher in patients seeking treatment within 24 h of the earthquake than in those arriving 24 to 72 h after the earthquake (P=.001). C, Where hypothermia developed in patients with a temperature<35ºC (N=47) seeking treatment within 24 h of the earthquake. D, Where hypothermia developed in patients with a temperature<35ºC (N=12) seeking treatment 24 to 72 h after the earthquake. In patients with a temperature <35ºC, the percentage of patients who developed hypothermia outdoors was significantly higher within 24 h of the earthquake than 24 to 72 h after the earthquake (P=.002).
Rewarming Methods
Passive external rewarming was exclusively used in 27 of 32 patients in the potential hypothermia group, 28 of 45 patients in the mild group, 1 of 8 patients in the moderate group, and none of the 6 severe hypothermia cases. In contrast, active rewarming methods (active external rewarming, warmed fluid infusion, or both) were used in 3 of 32 patients with potential hypothermia, 15 of 45 patients in the mild group, 6 of 8 patients in the moderate group, and 4 of 6 patients with severe hypothermia. Patients who were treated using both passive external rewarming and active rewarming methods were classified as active rewarming patients. The rewarming methods used were unknown in 7 patients (potential N=2, mild N=2, moderate N=1, and severe N=2). Also, 5 patients received a warm fluid infusion, 1 patient in the potential group and 4 patients with mild hypothermia. Of those 5 patients, 1 patient in the mild group was treated exclusively using a warm fluid infusion, and the other 4 patients were treated concurrently with passive external rewarming methods. None of the patients was rewarmed with more invasive methods (eg, body cavity lavage or extracorporeal circulation).
Outcomes
Follow-up of the patients treated for hypothermia in the aftermath of the GEJE indicated that 66 of the 91 patients (72.5%) were discharged without sequelae. Of the remaining patients, 8 (8.8%) were able to live as before in spite of mild sequelae, 7 (7.7%) required physical assistance due to sequelae, and 4 patients (4.4%) died. A significantly higher percentage of patients who sought treatment within 24 hours of the earthquake were discharged without sequelae compared to those who sought treatment in the 24 to 72 hours after the earthquake (83.3% vs 44%, P<.001, Figure 4A, 4B). This observation was true for the whole cohort and for patients admitted with a temperature of less than 35°C (83% vs 50%, P=.01, Figure 4C, 4D).

Figure 4 Treatment Outcomes for Hypothermia in Patients Seeking Treatment Within 72 Hours of the Earthquake. A, Patients seeking treatment within 24 h of the earthquake (N=66). B. Patients seeking treatment 24 to 72 h after the earthquake (N=25). The percentage of patients who were discharged without sequelae was significantly higher in those arriving within 24 hours of the earthquake compared to those arriving 24 to 72 h after the earthquake (P<.001). C. For patients with a temperature <35ºC seeking treatment within 24 h of the earthquake (N=47). D, Treatment outcome for patients with a temperature <35ºC seeking treatment 24 to 72 h after the earthquake (N=12). The percentage of patients who were discharged without sequelae was significantly higher than those seeking treatment within 24 h of the earthquake than those arriving 24 to 72 h after the earthquake (P=.01).“Live independently” defined patients who could live as before in spite of mild sequelae. “Need assistance” defined patients who needed physical assistance in daily life.
In contrast, the percentage of patients without sequelae did not significantly differ among the 4 groups based on the severity of hypothermia at admission (P=.26, Table). We also compared patient outcome based on whether the hospitals’ heating system was functional. No significant difference was found in the percentage of patients who were discharged without sequelae regardless of whether the heating system was functional or not (72.6% vs 72.4%, P=1.00). The reported complications in all 91 patients included infections (N=9), which were subdivided into pneumonia (N=5) and sepsis (N=1); cerebral infarction (N=3); convulsions (N=1); heart failure (N=5); angina pectoris (N=1); and pulmonary embolism (N=2).
Discussion
The majority of patients with hypothermia (72.5%) admitted to the emergency hospitals in Miyagi Prefecture within 72 hours of the GEJE had hypothermia caused by being struck by the tsunami. Many of the patients sought treatment within 24 hours of the earthquake. Most patients had a temperature of 32ºC or higher on arrival at the hospital and were classified as potential or mild hypothermia cases in our survey. The patients were rewarmed primarily by passive external rewarming using blankets. In general, their outcomes were favorable: 68.8% had no sequelae and 10.4% were able to live independently.
This survey included patients with temperatures between 35ºC and less than 36ºC, which is not generally considered a state of accidental hypothermia. In fact, 32 of 91 (35%) patients were classified as potentially hypothermic. Shivering can occur even when the core temperature is above 35°C.Reference Sessler 22 Thus, health care providers might consider this a symptom of hypothermia and it may be one of the reasons why so many patients who had temperature between 35 and less than 36°C were hospitalized.
In the 24 to 72 hours after the earthquake, 25 of 91 patients (27.5%) sought treatment (Figure 1). One of the probable causes for the delay of the hospital visit was the difficulty in gaining access to the hospital. The serious shortage of medical resources that existed before the earthquake in the coastal area of Miyagi Prefecture was exacerbated by the devastating damage.Reference Ishii and Nagata 25 In fact, 3 secondary emergency hospitals were destroyed almost completely by the tsunami. A geographically complex coastline also created access difficulties.Reference Ishii and Nagata 25 Therefore, the patients had problems in seeking hospitals.
Heating Systems at the Hospitals
No working heating system was available after the earthquake at 7 of 13 hospitals. The heaters became available within 72 hours of the earthquake at 4 of the 7 hospitals. Overall, 10 of the 13 hospitals had working heating systems by 72 hours after the earthquake. In addition to rewarming, treatment for accidental hypothermia includes methods to reduce heat dissipation. These methods may include removing wet clothes and keeping the room warm.Reference Howard and Bessen 11 Although many of the hypothermic patients sought treatment within 24 hours of the earthquake, many hospitals had to treat them without working heating systems.
Causes of Hypothermia
Hypothermia was caused by being struck by the tsunami in 72.5% of patients who sought treatment within 72 hours of the earthquake. In the first 24 hours after the earthquake, more than 80% of the patients with hypothermia (55/66) who sought treatment were affected by hypothermia associated with the tsunami. Consistent with this finding, in the 66 patients admitted for care in the first 24 hours after the earthquake, 37 patients (56%) had developed hypothermia outdoors. The number of patients admitted the hospital decreased between 24 and 72 hours after the earthquake to 25 patients. Of the patients admitted later, 19 of 25 patients (76%) had developed hypothermia indoors.
The majority of admitted patients (83/91) were affected by potential to mild hypothermia. Previously published workReference Molnar 16 has demonstrated that about 50% of people exposed to water between 5ºC and 10ºC for 1 to 2 hours die. It is reasonable to conclude that people struck by a tsunami in a cold climate, like the victims of the GEJE, are likely to die unless they escape from the cold seawater quickly. We would suggest that escape leading to a relatively short exposure to the cold seawater was likely the reason most patients were only affected by potential to mild hypothermia. Many of the patients who were hypothermic without being exposed to the tsunami had underlying disorders. The most common were cerebrovascular disorders, which were found in 8 patients. These patients had primary hypothermia due to heat loss inside buildings where no heating was available. In particular, those with underlying cerebrovascular disorders may have developed hypothermia that could have resulted from a compromised thermoregulatory capacity of the body.Reference Brown, Brugger, Boyd and Paal 10 In addition, if these patients had altered mental status, motor or sensory dysfunction, or gait disturbance attributable to their underlying cerebrovascular conditions, it may have been physically difficult for them to relocate to warm locations or seek medical care.
Rewarming Methods
Most patients with potential to mild hypothermia (temperature of 32ºC or higher) were treated with passive external rewarming methods that required no electricity. Active external rewarming methods using electric warming devices were used more frequently in patients with moderate to severe hypothermia (temperature of less than 32ºC).
Typically, the method of rewarming patients with accidental hypothermia varies depending on the treatment policy of the medical institution and the warming devices available. In general, passive external rewarming is used to treat mild hypothermia, and moderate to severe hypothermia is treated using active external and internal rewarming methods. Although the surveyed hospitals generally use these standard treatments, very few patients were treated with warm fluid infusion, which is a minimally invasive method for active internal rewarming.Reference Brown, Brugger, Boyd and Paal 10 , Reference Howard and Bessen 11 , Reference Kempainen and Brunette 13 Administering warm fluids is recommended to treat hypothermic patients because it is a simple technique without complications.Reference Howard and Bessen 11 However, in this survey, it remains unknown why so few patients were treated using warmed fluid infusion. In addition, none of the patients were treated with more invasive active internal rewarming techniques, such as intrathoracic or intraperitoneal lavage and extracorporeal circulation, probably because available medical resources were limited. While severe hypothermia with circulatory collapse can be successfully treated with extracorporeal circulation,Reference Walpoth, Walpoth-Aslan and Mattle 26 it takes a long time to start this complicated technique.Reference Kempainen and Brunette 13
Interestingly, van der Ploeg and colleagues reported no significant difference in the survival rate in a retrospective survey of 84 hypothermic patients treated with single or multiple rewarming methods.Reference van der Ploeg, Goslings, Walpoth and Bierens 27 In this survey, the rate of rewarming for each type of rewarming technique (passive external rewarming vs active external rewarming) was not specified. Active external rewarming has been associated with a faster rate of rewarming but with no outcome improvement.Reference Steele, Nelson and Sessler 28 In this survey, the time it took to rewarm the patient was available for only a few patients. Therefore, we could not compare the rate of rewarming. Currently, no studies have shown that a difference in the rewarming methods applied affects the outcome of hypothermic patients. Patients with mild hypothermia and no complications can be successfully treated with passive external rewarming alone.Reference Kempainen and Brunette 13
In this survey, we were not able to describe how differences in the rewarming method affected outcome. However, the results suggest that the standard rewarming methods used to treat accidental hypothermia in ordinary clinical practice can result in a favorable outcome even during a disaster. In fact, because only 14 patients had moderate to severe hypothermia after the earthquake, almost all of them could have been rewarmed with active external rewarming techniques, even given the restricted lifeline. However, if a larger number of patients with moderate to severe hypothermia had required treatment, passive external rewarming may have been the only choice because of blackouts and damage to the heating systems. In this situation, limited treatment options may have had an impact on treatment outcome.
Outcomes
Of the 91 hypothermic patients, 74 (81.3%) treated after the earthquake had no sequelae or could live independently after discharge and only 4 patients (4.4%) died. In this small sample size, the mortality rate for patients with moderate to severe hypothermia (temperature <32ºC) was 7.1% (1 of 14 patients). Previous studies have reported varying mortality rates for patients with accidental hypothermia, ranging from 17% to 60%.Reference van der Ploeg, Goslings, Walpoth and Bierens 27 , Reference Vassal, Benoit-Gonin, Carrat, Guidet, Maury and Offenstadt 29 - Reference Kornberger and Mair 32 Compared with these studies, the mortality rate shown in this survey was low in spite of the lack of functional heating at many hospitals after the GEJE. Many of the patients with post-earthquake hypothermia were thought to have been otherwise healthy and lived normally. Therefore, one possible explanation for the low mortality rate could be that these patients had no underlying disorders and were simply hypothermic from exposure to the tsunami.
The outcome of patients who sought treatment 24 to 72 hours after the earthquake was worse than patients who sought treatment within 24 hours of the earthquake. More patients admitted between 24 and 72 hours had hypothermia that was not associated with the tsunami, and these patients may have been exposed to the cold weather longer. However, no clear reason for the hypothermia was identified. Even in this population, the 12.0% mortality rate documented among hypothermic patients was lower than the mortality rates reported elsewhere.Reference van der Ploeg, Goslings, Walpoth and Bierens 27 , Reference Vassal, Benoit-Gonin, Carrat, Guidet, Maury and Offenstadt 29 These results suggest that the outcome of patients treated within 24 hours may have been quite favorable. Identifying why patients treated in the 24 to 72 hours after the earthquake had worse outcomes, and developing a strategy to treat these patients, could improve their outcomes.
Hypothermia Treatment at the Time of the Disaster
A large number of people are expected to rush to hospitals immediately after a natural disaster; however, medical institutions tend to malfunction because their lifeline shuts down. The resulting imbalance between medical supply and demand can greatly affect medical activities. Minimizing this imbalance is an important issue that needs to be addressed in the early stage of disaster medical care. In this survey, more than 80% of patients were only potentially hypothermic or had mild hypothermia, which was successfully treated using passive external rewarming techniques similar to normal operations. These results could be valuable for informing the development of strategies for future disaster medical care. For example, patients with temperature between 32ºC and less than 36ºC do not necessarily need to be treated at medical institutions if only passive external rewarming is required. They can be triaged at hospitals first and then receive treatment outside the hospital. In fact, with a large stock of covering materials, such as blankets or aluminum sheets, hypothermic patients can be treated at local shelters. This alternative strategy would help reduce the number of inpatients and the burden on medical institutions in the early post-disaster phase.
Limitations
The high incidence of hypothermia and the large number of drowned patients could be easily inferred from a tsunami disaster. We were not able to include all possible hypothermic patients because there was not adequate information available pertaining to outpatients at many institutions due to the simplified documentation implemented in the aftermath of the earthquake. We included only inpatients with adequate clinical information and assumed that patients with severe symptoms would have been hospitalized. In this survey, the questionnaires asked the minimum number of questions about each hypothermia patient. Thus, we were not able to describe some of the details about the patients (eg, field situation, clinical symptoms/complaints, and diagnosis other than hypothermia) after the GEJE. These details may have some kind of influences to their variables (eg, temperature on arrival) and their outcomes. The questionnaire included the minimum number of questions because (1) an extensive questionnaire form may have increased the strain on respondents leading to many blank replies; (2) given the extent of the damage, it was presumed that most of the included patients, even patients with a temperature of more than 35ºC, would be diagnosed with hypothermia, and that patients with other diagnoses were unlikely to be included; and (3) respondents from the hospitals might not necessarily have medical expertise. However, not all the patients had complete records because questions were left unanswered. This deficit was likely due to incomplete records obtained during the confusion in the early stage of a catastrophic disaster. We had to abandon further investigation into incomplete records.
Accidental hypothermia is generally diagnosed based on the patient’s core temperature. However, in this cohort the temperature was not measured using a standardized method (measurement site and device). When the core temperature was obtained, it was measured at different sites and many patient records lacked core temperature data. The site of temperature measurement and the devices used also differed among the surveyed hospitals. Temperature measurement from different anatomical sites is quite inconsistent in each person.Reference Brown, Brugger, Boyd and Paal 10 While core temperature is required to accurately diagnosis accidental hypothermia it could not be obtained using a recommended method in all patients at the time of the disaster. This was likely due to the surge in the number of patients in hospital emergency rooms.
This survey might not reflect all the CPA patients associated with hypothermia. There was 1 severe hypothermic patient with CPA in this survey. It was not possible to investigate the hypothermia-related CPA patients who were not taken to hospitals because they had no medical records. Immediately following the earthquake, many CPA patients, who normally would have been taken to hospitals quickly, were likely triaged black (ie, likely to die) and might have been left untreated. This finding may have affected the fatality count and mortality rate.
Another limitation of this survey is that a patient hospitalized at 1institution and then transferred to another could have been counted as 2 patients. We could not know how many patients were double counted in this survey due to transfer because we collected de-identified data. However, we concluded it is likely that only a small number of patients could have fallen into this category and that the results would have been only minimally influenced by these patients. This conclusion was based on the absence of any hypothermic patient being transferred from any other hospital to the Tohoku University Hospital, 1 of the 4 tertiary emergency hospitals in Miyagi Prefecture. Finally, this survey may have included patients whose normal temperature was between 35ºC and less than 36ºC.
Conclusions
A total of 91 patients with a temperature of less than 36ºC in Miyagi Prefecture sought treatment in the first 72 hours following the GEJE. The primary cause of hypothermia was exposure to the tsunami. Most patients received treatment within 24 hours of the earthquake. Although many of the hospitals where the hypothermic patients were hospitalized had no working heating system, favorable treatment outcomes were observed for patients with potential to mild hypothermia arriving within 24 hours after the earthquake. Patients who sought treatment 24 to 72 hours after the earthquake had worse outcomes. However, no clear reason for this was identified. These findings suggest that patients who are potentially hypothermic or who have mild hypothermia can be treated outside medical institutions and may not require inpatient care in the early post-disaster phase.
Funding and Support
This work was supported in part by a Challenging Exploratory Research grant (No. 24659794) from the Japanese Ministry of Education, Culture, Sports, Science, and Technology; Supporting Funds for Emerging Industry from Tohoku Bureau of Economy, Trade and Industry, Daiwa Securities Health Foundation, SENSHIN Medical Research Foundation, Mitsui Life Social Welfare Foundation, Takahashi Industrial and Economic Research Foundation, ZENKYOREN (National Mutual Insurance Federation of Agricultural Cooperatives), The Marumo Fund, Daido Life Welfare Foundation, and Special Research Project of International Research Institute of Disaster Science, Tohoku University.
Acknowledgments
Tomohiro Tanno, Tohoku University Graduate School; Rumiko Okada and Shizuka Osaki, Department of Emergency and Critical Care Medicine, and Yayoi Okano, Department of Neurosurgery, Tohoku University Graduate School of Medicine; Michio Kobayashi, Emergency Center, Japanese Red Cross Ishinomaki Hospital; Sae Ochi, Department of Epidemiology and Biostatistics, Imperial College London School of Public Health; and the directors and emergency center staff at 72 secondary and tertiary emergency medical institutions in Miyagi Prefecture assisted with this survey. Lloyd Kawakami (Manoa DNA) and Mr and Mrs Takaya Yokokawa supported our research activities.