Introduction
Ketamine is a commonly used sedating and anesthetic agent in the hospital settingReference Olives, Nystrom, Cole, Dodd and Ho 1 with a relatively rapid onset of effect (three to eight minutes) after intramuscular (IM) administration. It is used in emergency departments (EDs) to facilitate painful and fear-provoking procedures necessitating moderate sedation, particularly in pediatric patients.Reference Ahern, Herring, Stone and Frazee 2 - Reference McCarty, Mencio, Walker and Green 6 Previous works demonstrate its efficacy as a prehospital analgesic agent in the setting of severe traumaReference Roback, Wathen, Bajaj and Bothner 7 - Reference Tran, Nguyen and Truong 10 and as a well-tolerated surgical anesthetic in austere and resource-poor settings.Reference Wiel, Zitouni and Assez 11 , Reference Paix, Capps, Neumeister and Semple 12 Despite its frequent use in these settings, the use of ketamine as a first-line agent to control prehospital agitation is not accepted widely.
Profound agitation represents a significant risk to patients and providers alike, and the use of prehospital physical and chemical restraint during transport often is required to maintain the safety of the patient, first responders, and medical staff.Reference Mellor 13 - Reference Southall, Grant, Fowler and Scott 15 Case reportsReference Bunai, Akaza, Jiang and Nagai 16 , Reference Hick, Smith and Lynch 17 and laboratory dataReference O’Halloran and Lewman 18 - Reference Chan, Vilke, Neuman and Clausen 22 suggest that physical restraint of profoundly agitated individuals may decrease venous return, impair physiologic recovery, and decrease chest wall excursion and minute ventilation. Taken together, these changes suggest impairment in physiologic compensation for the metabolic acidosis incurred by persistent agitation. In the setting of psychomotor stimulation and substance abuse, profoundly agitated patients who are restrained forcefully may thus be at high-risk for cardiovascular collapse.Reference Reay, Howard, Fligner and Ward 23 Sedation with classically employed, slower-onset chemical restraints, such as haloperidol and the benzodiazepine sedative-hypnotic class, carries the risk of a delay to adequate sedation that is clinically significant in the setting of often brief ambulance transport.Reference Chan, Vilke and Neuman 24
Ketamine has emerged as a potentially useful agent for the control of subjects with undifferentiated prehospital agitation, but dosing guidelines, safety profile, and efficacy have been described in only a limited fashion. Published case series of ketamine therapy for agitation in the prehospital setting are few,Reference Isenberg and Jacobs 25 , Reference Burnett, Salzman, Griffith, Kroeger and Frascone 26 although several small case series and individual cases have been reported.Reference Burnett, Peterson and Stellpflug 27 - Reference Pritchard and LeCong 30 Preserved respiratory drive classically is described once a ketamine-induced dissociative state is achieved, but little data are available regarding the rate of intubation in this setting. The few large series reported suggest that the rate of intubation among agitated patients treated with prehospital ketamine is higher than that of patients treated with more traditionally accepted sedatives, although time to adequate sedation is more favorable.Reference Svenson and Abernathy 31 , Reference Iwanicki, Barrett and Saghafi 32 The authors thus sought to define the rate of intubation in profoundly agitated patients receiving prehospital ketamine at high (>5mg/kg) and low (≤5mg/kg) doses, and to describe clinically important outcomes associated with this therapy.
Methods
Study Design
This was a retrospective cohort study of all patients who received prehospital ketamine for control of profound agitation per a pre-defined Emergency Medical Services (EMS) protocol (Figure 1) and who were transported to an urban county hospital. Exposure to prehospital ketamine from May 1, 2010 through August 31, 2013 was identified by a directed computerized search of the prehospital service database (“SafetyPAD” EMS Information Management System, Open Inc.; Bloomington, Minnesota USA) for all references to “ketamine” during the period reviewed. These episodes of care were matched to hospital records from the date of contact. The governing Office for Human Subjects Research at Hennepin County Medical Center (Minneapolis, Minnesota USA; where the EMS system is based) approved this study.
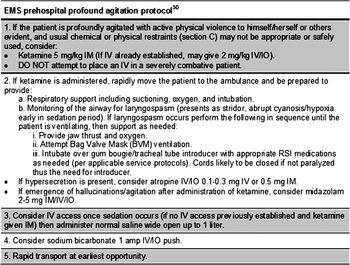
Figure 1 EMS Prehospital Profound Agitation Protocol. Abbreviations: EMS, Emergency Medical Services; IM, intramuscular; IO, intraosseous; IV, intravenous.
Study Setting & Population
The study was conducted at a Level 1 urban trauma center with more than 100,000 annual ED visits from a culturally and linguistically diverse patient population representing over 50 language groups. Prehospital data were provided by a third-service, hospital-operated EMS system which answers over 68,000 calls annually, serves an urban and suburban population of over 1,000,000 residents, and covers more than 200 square miles. On an annual basis, the service responds to over 400 calls coded specifically as “agitation.” Some of these episodes of care meet protocol-defined criteria for “profound” agitation. All ambulances are Advanced Life Support certified and staffed with two paramedics.
Study Protocol
In May 2010, the EMS service instituted standing orders facilitating ketamine administration by paramedics for control of profound agitation, defined as the patient who displays “active physical violence to himself/herself or others…and usual chemical or physical restraints…may not be appropriate or safely used.”Reference Cole, Nystrom and Orozco 33 In the case of this EMS system, “usual chemical restraint” is attained via IM, intravenous, or intraosseous administration of midazolam (5mg) and/or haloperidol (5-10mg). Ketamine is available to prehospital providers for the management of profoundly agitated patients, as described in Figure 1. It is administered intramuscularly in a dose of 5mg/kg based on estimated body weight. Although rarely applicable, up to 2mg/kg also may be administered intravenously if peripheral vascular access has been obtained.
All individuals ≥18 years of age treated with ketamine for profound agitation in the prehospital setting were eligible for inclusion in the study. Patients known to be pregnant or who were transported to other facilities were excluded from the study. Those who received ketamine purely for analgesic purposes per a parallel EMS protocol for acute pain management were excluded. Therefore, only non-pregnant patients, ≥18 years of age, who received prehospital ketamine for control of profound agitation were included.
Prehospital and electronic hospital medical records were reviewed for each potential study subject identified as having received prehospital ketamine. Indication for prehospital ketamine was noted specifically in a unique data entry field in all EMS run sheets. Cases meeting inclusion criteria were enrolled in the study and evaluated as described in the Measurements and Data Analysis sections. Two authors (PN, EMS fellow and TO, emergency medicine resident physician) jointly abstracted all data from the electronic medical record. Oversight was provided by the EMS medical director (JH). Consensus between the two chart abstractors was achieved in all cases for which interpretation of hospital or prehospital data differed. Vital and laboratory data were abstracted from vital sign flow sheets and laboratory results sections of the electronic medical record; in cases of vital or laboratory derangements reported in provider notes, but not verified in vital sign or laboratory flow sheets, flow sheet data are reported. Physiologically implausible vital signs (eg, diastolic blood pressure greater than systolic blood pressure or temperature of 9.8 degrees Fahrenheit) were excluded following consensus. Data collected during the hospitalization but following ED management was not included in the analysis. Missing data (eg, no temperature recorded) was coded as such. Abstractors reviewed coding and verified consistency of practice on multiple occasions throughout the study.
All prehospital data points (case impression, ketamine dosing and complications, response to ketamine, and additional sedation) were entered electronically into a data collection sheet (Microsoft Excel 2011, Microsoft Corp.; Redmond, Washington USA) and matched by name, date and time of EMS run, and clinical context to the corresponding hospital encounter on the same date and time. In a large majority of cases, prehospital EMS run sheets were available as scanned documents in hospital charts, further verifying appropriate matching.
Measurements
The paramedic case impression, ketamine dose and route, time of presentation, and additional prehospital sedation (ie, haloperidol and midazolam) were abstracted from the prehospital database. Because the protocol followed by the prehospital providers mandates an IM dose of ketamine approximating 5mg/kg, this was chosen as a cutoff to assess for exposure to a high (>5mg/kg) or low (≤5mg/kg) ketamine dose for the purpose of analysis. Case impression is assigned by the EMS provider at the point-of-care based on observations made at the scene, often with baseline vital sign measurements, but typically absent advanced diagnostics. Case impressions are the basis on which treatment is initiated prior to arrival at the ED.
Prehospital data points were combined with data abstracted from the subject’s medical record, including age, gender, presenting vital signs in the ED, and laboratory data including serum or breath ethanol (ETOH) level, serum bicarbonate, lactate, creatine kinase, venous or arterial pH, and urine toxicology testing (immunoassay followed by high-performance liquid chromatography and mass spectrometry). Prehospital and medical records were reviewed for evidence of clinically significant complications of ketamine administration. Hour of presentation was recorded as a proxy for resources available in the ED. Race could not be abstracted verifiably from the chart retrospectively and thus is not reported. Where patient weight from the encounter was not recorded immediately, the most proximal weight documented within one month of presentation was used to estimate weight-based ketamine dosing.
Intubation and indication for intubation, where directly referenced, were abstracted from the electronic medical record. No list of uniformly accepted indications for intubation of the agitated patient is utilized at the receiving institution. While it is not standard practice to intubate agitated patients for safety and expeditious evaluation, it is common practice to aggressively treat agitation with chemical restraint and appropriate environmental cuing. Failing these measures, intubation is undertaken in the most refractory cases, particularly those felt to be at risk of secondary complications (eg, rhabdomyolysis, persistent acidemia, or physical injury).
Data Analysis
Descriptive statistics were employed to characterize the study population. Using the Shapiro-Wilk method at an α of 0.001 and normal quantile plots, data generally were not distributed normally, and thus are presented as medians and interquartile ranges (IQRs). Univariate analyses describe the association between intubation and baseline demographic and collected clinical data using the Mann-Whitney U test, Pearson’s χ2, or Fisher’s exact χ2 statistic, as appropriate to the data. Logistic regression was used to further evaluate variables associated with intubation. Hosmer-Lemeshow goodness-of-fit χ2 statistics were calculated subsequently to evaluate acceptable model fit. All data analyses were completed using Stata 12.1 (StataCorp; College Station, Texas USA).
Results
Prehospital ketamine was administered on 227 occasions during the study period. Of these, 92 were excluded. A single patient with recurrent episodes of encephalopathic behavior was responsible for 38 of 47 exclusions due to EMS transport to a different facility. 34 An additional 33 were excluded due to protocol-driven use of ketamine solely for analgesia, and 12 doses were excluded due to administration to patients less than 18 years of age. A total of 135 episodes of prehospital ketamine administration for profound agitation thus were included for analysis (Figure 2).

Figure 2 Study Flowsheet.
Baseline demographic and vital data are presented in Table 1. Overall, 44% (60) of patients presented with tachycardia at or above 120 beats per minute, and 35% (48) presented with Stage 2 systolic hypertension (systolic blood pressure of >160mmHg) or above. Patients were predominantly male (108/135; 80%). In general, patients who were intubated presented with baseline vital signs similar to those who were not intubated. Several records contained incomplete vital data, including systolic blood pressure (1) and weight (15). Of the 15 records without a documented weight, 13 were non-intubated subjects.
Table 1 Baseline Characteristics (all data presented as median and interquartile range, unless otherwise noted)

a Data missing for 13/50 un-intubated and 2/85 intubated subjects.
b Data massing for 1/85 intubated patients (presented to emergency department in arrest).
The median dose of ketamine was 5.20mg/kg (IQR=4.59-6.07mg/kg) with weights available in 120 patients. Ketamine doses in excess of 5mg/kg were administered to 70 subjects; a maximum dose of 11.5mg/kg was administered to a patient who did not require intubation. Ketamine dosing did not differ significantly between intubated and non-intubated patients (median 5.25mg/kg and 5.14mg/kg, respectively; Mann-Whitney U-test P=.68). Emergency Medical Service providers reported initial improvement in agitation following ketamine administration in 124/135 (91.8%), no change in 9/135 (6.7%), and worsened agitation in 2/135 (1.5%) of cases.
Endotracheal intubation was undertaken in 85 subjects (63%). Of these, EMS providers attempted intubation in four subjects (2.96%) in the prehospital setting. No cases of pulmonary edema or laryngospasm were verified in the ED charts. Increased oropharyngeal secretions, a known effect of ketamine administration, were not considered clinically important complications for the purpose of this study. The circumstances surrounding prehospital intubations, as well as noted complications of ketamine administration, are characterized in Table 2. Among the four patients in whom prehospital intubation was undertaken, one experienced post-ketamine vomiting and jaw clenching, followed by two failed intubation attempts and placement of a supraglottic airway prior to ED intubation. Another patient experienced transient severe hypoxemia after intubation attempts were frustrated by a strong gag. An oral airway was placed, after which the patient was intubated in the ED. Two more were intubated prehospital, one due to cardiac arrest and the other due to a clinical impression of “coma with an absent gag reflex.”
Table 2 Prehospital Intubation Cases and Reported Complications of Ketamine Administration in the Prehospital Setting

Note: Prehospital “respiratory depression” is reported in 18 additional patients following ketamine administration. Most EMS run sheets note “suspected hypoxemia” as the basis for intervention. Prehospital treatment commonly included oxygen administration by one or a combination of nasal cannula or facemask (9), bag-valve mask ventilation (8), nasal airway (4), repositioning (2), suctioning (1), and oral airway placement (1). Six of the 21 (29%) respiratory complications had also received IM midazolam alone (n=3; range 2-10mg) or in combination with haloperidol (n=3; range 5-10mg).
Abbreviations: CPR, cardiopulmonary resuscitation; ED, emergency department; EMS, Emergency Medical Services; ETOH, ethanol; IM, intramuscular; ROSC, return of spontaneous circulation.
a No weight on file.
Detailed explanations of the rationale behind the decision to intubate in the ED uniformly were unavailable. Directly referenced indications for the procedure included airway protection (69 references); respiratory failure, depression, distress, or apnea (16 references); ongoing agitation or violence (eight references); cardiac arrest (two references); and altered mental status (one reference). A single indication was referenced in 64/85 intubations (75.3%), more than one indication was referenced in 19/85 intubations (22.4%), and no indication was referenced directly in 2/85 intubations (2.4%).
Adjunctive prehospital sedation was administered to 19 patients (14.1%), including midazolam (8/19), haloperidol (1/19), or both (10/19). Intubation rates were similar across groups receiving any or no adjunctive therapies (68.4% versus 62.1%; Pearson χ2 P=.595).
Fifty-five patients (40.7%) presented to the ED between the late night hours of 11:00 pm and 7:00 am (overnight). Intubation occurred in 74.6% (41/55) of overnight patient encounters, compared to 55% (44/80) of daytime patient encounters (Pearson χ2 P=.021)
Presenting laboratory results are described in Table 3. Intubated patients presented with lower venous pH values (7.25 versus 7.33; Mann-Whitney U-test P=.018), but laboratory data otherwise were distributed similarly. The urine of 107 patients (79.3%) was sent for toxicological screening. Of these, six (4.4%) tested negative for any detectable substances; evidence of sympathomimetic ingestion was found in the urine of 34 subjects (31.8% of those tested). Cocaine was detected in the urine of 20 patients (18.7%), amphetamines in 19 (17.8%), and phencyclidine in one patient (0.93%). Urine toxicology was positive for both amphetamines and cocaine in six patients (5.6% of those tested).
Table 3 Presenting Laboratory Data

a Median concentration including those with detectable levels. Among those with undetectable ethanol concentrations: Intubated (n=72)=0 (0.0-0.18); Not intubated (n=28)=0 (0.0-0.17).
b Significant difference between groups (Mann-Whitney U-test P<.05).
Univariate analyses revealed statistically significant associations between intubation and both male gender (Pearson’s χ2=12.02; P=.001) and ED arrival during the overnight shift between 11:00 pm and 7:00 am (Pearson’s χ2=5.34; P=.021). Rates of intubation were similar between subjects receiving low-dose (≤5mg/kg) and high-dose (>5mg/kg) ketamine (72.0% versus 67.1%; Pearson’s χ2=0.323; P=.57; Figure 3). Paramedic case impression (Table 4), age >40 years, objective evidence of ETOH or sympathomimetic ingestion on presentation, and prehospital co-administration of midazolam or haloperidol were not associated with intubation.

Figure 3 Ketamine Dosage by Intubation Status.
Table 4 Paramedic Case Impressions

Logistic regression modeling included binary variables for age (age ≤40 versus >40 years), ketamine dose (≤5mg/kg versus >5mg/kg), gender, co-administration of any prehospital midazolam or haloperidol, and ED arrival time (Table 5). Emergency Medical Service case impression was not included in the adjusted analysis due to inconsistencies in coding of similar presentations and a high likelihood of misclassification bias. Urine toxicology assessments were undertaken on fewer than 80% of subjects, and thus these results were not included in the adjusted analysis. Ethanol concentration similarly was omitted. A total of 120 subjects therefore were included in regression analysis when accounting for those without weights recorded within a month of their presentation. The association between male gender and intubation persisted in adjusted analysis (odds ratio=1.91; 95% confidence interval, 1.14-3.21), as did late night arrival (odds ratio=2.57; 95% confidence interval, 1.05-6.27). Neither age >40 years, ketamine dosing (>5mg/kg), nor co-administration of haloperidol or midazolam was associated with intubation in this model. Binary cut-points of 30 years and 40 years were both modeled due to a bimodal age distribution in the study sample. Neither cut-point suggested an association between age and intubation (data not shown).
Table 5 Multivariate Analysis of Intubation Rates after Prehospital Ketamine
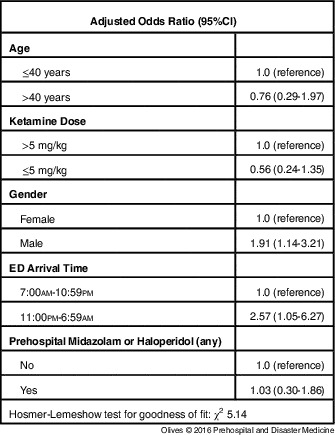
Abbreviation: ED, emergency department.
Two subjects sustained cardiac arrests shortly after ketamine administration. Both were treated initially with IM ketamine in doses at or near the median study dose. The first, a 36-year-old male, was found breathing sonorously after a reported mixed overdose of citalopram and clonidine. As EMS initiated cares and intravenous access, he became profoundly agitated requiring both physical restraint and chemical sedation. Following 500mg (6.25mg/kg) of ketamine, he was cooperative initially, but subsequently became obtunded. Three minutes after ketamine administration, a cardiac rhythm strip revealed a sinus rhythm with reported T-wave inversions. At nine minutes post-ketamine, the patient developed bradycardia and ultimately sustained a pulseless electrical activity arrest; a right bundle branch block with a prominent (4mm) r-wave in lead aVR was described. Resuscitative efforts were unsuccessful and the patient was pronounced dead 70 minutes after ketamine administration; basic labs were not collected during resuscitation. Emergency physicians cited pronounced clonidine toxicity as the likely cause of death, but post-mortem clonidine levels were not drawn. Autopsy results revealed quantitative citalopram and amphetamine blood levels of 6,100 nanograms per milliliter (reference level 9-200ng/mL at a daily dose of 30-60mg) and 340ng/mL (reference level 35-110ng/mL at a daily dose of 10-30mg), respectively.Reference Olives, Nystrom, Ho and Cole 35 The county medical examiner and the medical director of the regional Poison Center independently determined the cause of death to be citalopram and amphetamine toxicity in the setting of chronic substance abuse.
In the second case, EMS was called for a 42-year-old male who had sustained multiple seizures throughout the day following a period of antiepileptic medication refusal. First responders found the patient violent and agitated; EMS noted the same and administered a 500mg dose (approximately 5.15mg/kg based on most recent documented weight of 97kg) of IM ketamine. The patient was transferred to a waiting ambulance where he developed apnea and asystole. Advanced Cardiac Life Support was initiated and resuscitative efforts were continued in the ED where asystole persisted. Initial finger-stick glucose was 222mg/dL, serum sodium 161mEq/L, and serum potassium 6.1mEq/L. Resuscitative efforts failed, and the patient was pronounced dead 57 minutes after ketamine administration. Post-mortem examination revealed tongue hemorrhage consistent with his history of seizure. Further laboratory investigations revealed undetectable serum valproic acid and a urine drug screen with only the nicotine metabolite cotinine; volatile screens were unremarkable. The county medical examiner cited seizure disorder, sub-therapeutic anti-seizure medication levels, and atherosclerotic heart disease in the setting of cardiomegaly, hypertension, and a history of substance abuse as the cause of death.
Discussion
Endotracheal intubation was undertaken for 63% of study subjects, independent of ketamine dose. The case definition of this patient population denotes an immediate danger to themselves and others, and might reasonably impact the decision to undertake aggressive airway management. Thus, profound agitation alone may trigger endotracheal intubation irrespective of choice of sedating medication or response thereto. The degree of agitation identified during the prehospital provider’s initial clinical assessment may be articulated incompletely in the medical record, despite being conveyed verbally to the accepting emergency physician. Variables that impact the decision to intubate thus may be incompletely elucidated by this study.
This particularly is highlighted by the case impression coded by prehospital providers. It is subject to limitations inherent to the data that prehospital providers are able to obtain and is based on historical information obtained at the scene. Thus, two patients experiencing very similar pathophysiology may be coded differently. The absence of statistically significant differences in intubation rates across paramedic case impressions likely represents inexact and inconsistent coding, with probable confounding of the causal pathway between the true exposure and the decision to intubate.
Males in this study were more likely than females to be intubated; however, recorded serum pH, serum bicarbonate, evidence of sympathomimetic exposure, and ketamine dose per kilogram body weight were similar across the genders. It is plausible that providers perceived agitated males as a greater danger to providers once patients were admitted to the hospital, and thus intubated males at a higher rate. Furthermore, communication between prehospital providers and the receiving ED providers may convey a degree of urgency or potential danger unique to a specific patient that is captured inadequately in the medical record.
Patients presenting during the overnight shift were more likely to be intubated than those presenting during the day and evening. Among the 31 staff emergency physicians and fellows who cared for this cohort of patients, two providers accounted for 50.9% (28/55) of overnight encounters, but 65.9% (27/41) of overnight intubations. The same two providers comprised just 7.5% (6/80) of daytime encounters, but 11.4% (5/44) of all daytime intubations. This post-hoc finding suggests a provider-dependent practice with respect to airway management in the profoundly agitated patient after prehospital ketamine, and may signify a preference to intubate early when resources are less available (on overnight shifts). Alternately, different providers may variably perceive ketamine-induced dissociation, with some interpreting this as apnea or inadequate airway protection. Finally, it is also plausible that a high rate of intubation overnight represents a perceived safety measure in the absence of a full palette of resources to care for the acutely agitated patient on the hospital floor.
While two providers intubated a majority of profoundly agitated patients who received prehospital ketamine, their practice patterns were not outliers. Among those providers who cared for five or more subjects (n=10; 32.3%), intubation rates ranged from 0% to 100% (median=60%; IQR=25%-92%). These post-hoc findings imply that intubation following ketamine administration to control agitation in the prehospital setting – while common and provider-dependent – is not a universal practice, suggesting the need for further study.
The hemodynamic and laboratory parameters of this cohort do not display the degree of derangement characterized in some previously reported cases of profound agitation.Reference Bunai, Akaza, Jiang and Nagai 16 However, the improvement of vital sign derangement following prehospital ketamine has also been reported previously. 36 Other reports of severe agitation document substantially more deranged vital parameters, notably in the setting of confirmed sympathomimetic intoxication.Reference Burnett, Peterson and Stellpflug 27 In a larger series of patients who met criteria for excited delirium,Reference Maher, Walsh, Burns and Strote 14 only 37% (16) of patients presented with tachycardia in excess of 120 beats per minute, and only 7% (3) were hypertensive on presentation to the ED; 5% (2) were hypotensive. Few displayed serum bicarbonate levels of <10mEq/L (three patients; 7.5% of those with labs drawn) or a pH below 7.20 (two patients; 33% of those with labs drawn). By comparison, a large proportion of patients in this study presented with systolic blood pressures greater than or equal to 160mmHg (35%) and with tachycardia at or above 120 beats per minute (44%). Serum bicarbonate was below 20mEq/L in 42 patients (33.9%) and below 10mEq/L in four patients (3.2%), suggesting that this profoundly agitated patient population is comparable to previously described study populations.
The extent of vital and laboratory derangement seen in this study population may represent confounding by medical comorbidities and medications, precluding adequate characterization of agitation severity. Patients receiving beta-adrenergic antagonists for hypertension or anxiety, for example, may be incapable of mounting a tachycardic or hypertensive response that accurately reflects their degree of psychomotor agitation. Therapeutic excess of proserotonergic agents may precipitate dysautonomia, introducing variability into measured hemodynamic parameters.Reference Burnett, Watters, Barringer, Griffith and Frascone 37 Obstructive lung disease may chronically elevate serum bicarbonate levels, thus leading to an underestimate of the degree of acidosis revealed by this measure in isolation. Finally, a ketamine-induced dissociative state may contribute to a relatively low prevalence of severe hypertension, tachycardia, acidosis, and hyperpyrexia seen in this study following adequate control of neuromuscular agitation.
Few studies characterize the outcomes of agitated patients administered prehospital ketamine. Two small series in unselected patients suggest its utility for a range of clinical needs across a broad age range. In the largest of the two, Svenson & Abernathy reported the administration of ketamine to 40 trauma or medical patients ranging from two months to 75 years of age.Reference Ho, Smith and Nystrom 29 The most common indications for the employment of ketamine included analgesia in the setting of hypotension, sedation of the agitated patient without a definitive airway, and analgesia for pain refractory to narcotic pain management, with a reported dosing range from 1mg/kg intravenously to 5mg/kg intramuscularly. No adverse events were reported, although intubation rates following ketamine administration are not described. In a smaller series, Burnett et al describe the ED course of 13 patients in whom ketamine was administered in the prehospital setting for chemical restraint.Reference Chan, Vilke and Neuman 24 Of these, one required intubation for recurrent laryngospasm, one was intubated due to intracranial hemorrhage, and five were discharged directly from the ED. Of the 10 non-intubated patients, three were diagnosed by the treating provider as experiencing an emergence reaction. Two more recent series presented in abstract form report high rates of intubation (50% and 38%) and no deaths or laryngospasm in agitated patients administered prehospital ketamine.Reference Svenson and Abernathy 31 , Reference Iwanicki, Barrett and Saghafi 32
These results stand in contradistinction to two recent retrospective chart reviews reporting lower intubation rates. Burnett et al report a sample of 49 patients with a range of prehospital ketamine dosing (2.25-9.42mg/kg; mean 5.26mg/kg) that is similar to the patients in the present study.Reference Isenberg and Jacobs 25 The reported unadjusted rate of intubation of 29% is substantially lower than the rate herein. The mean ketamine dose reported in this study was significantly higher among intubated patients than among patients not requiring intubation; however, the authors note that their univariate model likely does not account for potential confounders. Additionally, although the difference in reported mean ketamine doses to intubated versus non-intubated patients achieved statistical significance, it is unclear that this is a clinically significant finding in a drug classically described in binary terms as “dissociative” or “sub-dissociative.” Keseg et al also recently describe EMS-reported improvement in agitation in a cohort of patients administered prehospital ketamine for agitation.Reference Boyer and Shannon 38 Although dosage per kilogram body weight was not described, mean ketamine dose was lower than the mean dose (324mg IM versus 466mg IM) reported in this study. Emergency Medical Services documentation of initially improved agitation was similar (91% in both studies), and improvement in agitation was noted by EMS providers despite eventual ED intubation in at least four patients. The authors similarly point out likely confounders of the relationship between ketamine administration and subsequent intubation, including suspected suicide attempt with polysubstance toxicity and ETOH intoxication. Taken together, these data add depth to a body of knowledge documenting substantial variability in clinically significant outcomes among patients who have received prehospital ketamine.
Finally, the two patients in whom cardiac arrest occurred are of particular concern. Electrocardiographic findings indicative of severe citalopram toxicity with markedly elevated serum citalopram concentration in the first subject strongly suggest profound serotonin toxicity, a process widely known to produce an agitated state.Reference Burnett, Watters, Barringer, Griffith and Frascone 37 In the second patient, critical electrolyte dysregulation in the setting of multiple seizures suggest the severity of their illnesses prior to ketamine administration. The degree of agitation encountered by prehospital providers likely is explained by both a post-ictal state and critical hypernatremia, both of which are known to induce alterations in behavior. The medical examiner investigation of both cases found no unifying physiologic mechanism related to ketamine, and in both cases, the critical illness associated with profound agitation strengthened the notion that this patient population must be aggressively medically managed to minimize the potential for poor outcomes. Both cases exemplify the variability of pathology underlying the clinical diagnosis of profound agitation and underscore the inexact correlation of initial case impressions with underlying pathology.
Limitations
Several important limitations constrain the interpretation of these data. First, this retrospective, single-center, observational study cannot be seen to suggest causality or to apply beyond this center, given the potential for clinical differences between patients transported to this facility and those transported to other facilities after prehospital ketamine. When excluding a single patient who was transported to another facility on 38 occasions, only nine others were excluded due to transport to an alternate facility. Second, this study is subject to limitations inherent to a retrospective review: collected data points cannot be expected to accurately or completely capture the gravity of prehospital agitation, nor can the authors infer a complete articulation of the rationale behind intubation or nuances to the paramedic report that may have influenced the decision to intubate. The high intubation rate may appropriately reflect overall severity of illness, a decision made based on EMS report, anticipated clinical course, available resources, irrespective of the degree of illness severity. It may also reflect variable provider perceptions of the dissociative state induced by ketamine as respiratory failure or failed airway protection. A prospective, ideally multicenter, interventional study of the chemical control of prehospital agitation is needed to validate these findings. Third, the case burden of agitated or combative patients transported by this EMS system likely is underestimated by paramedic case impression coding, as some cases of profound agitation may be coded based on additional contextual data. Finally, additional clinically important outcomes are not captured by this study, notably short- and long-term mortality and duration of intubation following exposure to prehospital ketamine in the setting of profound agitation.
Conclusions
A large proportion of patients in this series ultimately underwent endotracheal intubation independent of ketamine dosing, although male gender and late night ED arrival were both associated with higher rates of intubation. The basis for observed intubation rates remains unclear, but it appears plausible that indications incompletely articulated in the medical record, including incompletely articulated illness severity, or individual provider practice in the management of post-ketamine patients. Prospective research into both the efficacy and safety of prehospital ketamine and provider interpretation of the ketamine-induced dissociated state is warranted if the rationale for intubating these patients is to be understood completely.
Acknowledgements
The authors acknowledge the generous assistance of Ross Chávez, BA, NRP, CCEMT-P and David Rogers, EMT-P, EMS supervisor with the implementation of this study and the preparation of the resulting manuscript.










