Introduction
Lung cancer is the most common malignancy in the world and also the leading cause of cancer-related death, being responsible for 29 per cent of all deaths due to cancer.Reference Parkin, Bray, Ferlay and Pisani1 Survival depends on the size and stage of the tumour at diagnosis, with five-year survival rates of 49 and 2 per cent for early stage and disseminated primary tumours, respectively.Reference Bechtel, Petty and Saccomanno2 Published five-year survival rates for patients diagnosed with carcinoma in situ range from 75 to 91 per cent.Reference Edell, Lam, Pass, Miller, Sutedja and Kennedy3
Patients with squamous carcinoma of the head and neck constitute a high risk group for synchronous and metachronous tumours. In such patients, studies have reported a prevalence of second primary tumours of 7 to 21 per cent, with lung cancer being the most common type.Reference Stoeckli, Zimmermann and Schmid4 Smoking is known to be the most important aetiological factor in malignancies of the respiratory system, head and neck.Reference Moro-Sibilot, Jeanmart, Lantuejoul, Arbib, Laverrière and Brambilla5
Patients diagnosed with head and neck cancer require a thorough physical examination, especially of the upper aerodigestive system. X-ray, chest computed tomography (CT), positron emission tomography (PET) CT and upper aerodigestive tract endoscopy (commonly termed panendoscopy) are helpful in the pre-operative investigation of these patients. The diagnosis of central pre-neoplastic and early neoplastic lesions requires bronchoscopy, which also permits biopsy for histopathological examination.Reference Hujala, Sipila and Grenman6
In a previous study, conventional white light bronchoscopy was found to have a failure rate of 60 per cent in the diagnosis of high grade lesions of the central airways.Reference Lam, MacAulay, leRiche and Palcic7 The inadequacy of this method of detecting early lesions has led to investigation of new methods, and autofluorescence bronchoscopy has emerged as a more sensitive method of detecting pre-neoplastic and neoplastic lesions of the central airways.Reference Palcic, Lam, Hung and MacAulay8 Numerous clinical studies have found autofluorescence bronchoscopy to be superior to white light bronchoscopy in the detection of early lesions.Reference Goujon, Zellweger, Radu, Grosjean, Weber and van den Bergh9, Reference Lam, Kennedy and Unger10
Materials and methods
Autofluorescence bronchoscopy
When light of a certain wavelength is applied to tissue, fluorescence occurs.Reference Andersson-Engels, Klinteberg, Svanberg and Svanberg11 Upon excitation with blue light (wavelength 380–460 nm), abnormal tissue shows reduced fluorescence compared with normal tissue. The difference in the fluorescence of normal versus tumour tissue is explained by greater absorption of light by the thickened epithelium of the abnormal tumour tissue, or by decreased fluorescence stimulation in the submucosa. As a result, malignant tissue appears a dark blue-red under fluorescence, while normal mucosa appears green.Reference Qu, MacAulay, Lam and Palcic12 Digital technology enables the integration of millions of emitted fluorescent light signals, making possible real-time video imaging of the bronchial mucosa during autofluorescence bronchoscopy.Reference Hung, Lam, Le Riche and Palcic13
In the current study, we used the Onco-Life autofluorescence bronchoscopy device (Xillix Technologies, Richmond, British Columbia, Canada), comprising a video camera and an endoscopic light source compatible with conventional endoscopes (Figure 1). This device provides real-time images which can be displayed on a monitor. The Onco-Life device has two modes: conventional white light (the colour imaging mode) and fluorescence (blue light is used for this mode). The latter mode enables assessment of tissue fluorescence, facilitating the diagnosis of potentially pre-cancerous or cancerous tissue. Blue light is used to illuminate the tissue, stimulating the fluorophores already present in the tissue. During video imaging, normal areas and areas suspected to be pre-malignant or malignant appear green and brown-red, respectively (Figure 2).

Fig. 1 The Onco-Life autofluorescence bronchoscopy device.

Fig. 2 Bronchoscopic views showing enlargement and hyperaemia of the right lower lobe superior segment: (a) AFB view; normal (b) AFB view; biopsies were obtained from areas suspected of being premalignant or malignant and found severe dysplasia.
Spectrofluorometric studies have provided objective evidence that the autofluorescence of normal tissue, dysplastic tissue and carcinoma in situ differs.Reference Kurie, Lee, Morice, Walsh, Khuri and Broxson14–Reference Kusunoki, Imamura, Uda, Mano and Horai19 The sensitivity and specificity of autofluorescence bronchoscopy in detecting abnormal lesions are 73–89 per cent and 46–91 per cent, respectively.Reference Kurie, Lee, Morice, Walsh, Khuri and Broxson14–Reference Kennedy, Lam and Hirsch20 A significant number of abnormal lesions can be detected during conventional bronchoscopy; however, sampling all these lesions prolongs procedural time and increases the workload of the pathologist.Reference Beamis, Ernst, Simoff, Yung and Mathur21–Reference Venmans, van Boxem, Smit, Postmus and Sutedja24
Patients with laryngeal cancer have an increased risk of lung cancer. The aim of this study was to detect pre-invasive tracheobronchial lesions before they progressed to invasive cancer, and also to test the efficacy of bronchoscopy as a screening tool, bearing in mind that bronchoscopy is relatively straightforward where such patients have a permanent tracheostomy. This study also aimed to test the sensitivity and specificity of autofluorescence bronchoscopy and white light bronchoscopy in detecting abnormal lesions, by comparing their independent and combined use.
Between November 2007 and December 2008, 30 patients in the department of ear, nose, throat and head and neck surgery of Haseki Education and Research Hospital were included in this prospective study. These patients had undergone total laryngectomy for squamous cell carcinoma of the larynx, and had normal chest X-ray and chest CT results. The patients were referred to the Yedikule Chest Disease and Thoracic Surgery Hospital, where bronchoscopies were performed after the first post-operative month.
Patients with cardiovascular disease, bleeding diatheses and unstable asthma were not included in the study. We also excluded patients with nonlaryngeal head and neck cancer and those with subtotal laryngectomy (because of the safer and easier application of bronchoscopy after total laryngectomy).
Diagnostic bronchoscopy procedure
Informed consent was obtained from all patients before the procedure, and the study protocol was approved by the local ethics committee and institutional review board.
The Onco-Life (Xillix) autofluorescence and white light bronchoscopy device was used, always by the same physician (EC), who was experienced in the procedure. Pre-medication with 0.07 mg/kg midazolam was given before bronchoscopy, and supplemental lidocaine was applied through the working channel of the bronchoscope when necessary. Bronchoscopy was performed through the tracheostomy site in all patients (Figure 3). During bronchoscopy, oxygen was given at 2 l/min through the tracheostomy site via a cannula, and oxygen saturation and heart rate were monitored transdermally. Bronchoscopy commenced at the tracheostomy site and progressed toward the trachea, carina, main bronchi, lobes, segments and visible segmental bronchi, using first white light and then autofluorescence. In both modes, areas suspected to be pre-malignant or malignant were recorded. Finally, white light bronchoscopy and autofluorescence bronchoscopy were used in combination, and biopsies were obtained from all areas suspected to be pre-malignant or malignant. Samples were fixed in formalin, numbered and sent for histopathological examination. During white light bronchoscopy, severe erythema, mucosal thickening or irregularity, and nodular or polypoid changes were considered abnormal. During autofluorescence examination, all areas appearing brown or purple (rather than the normal green) were considered abnormal. To avoid error, friable and/or haemorrhagic fields and areas with dense mucous secretions were re-evaluated after lavage. In order to determine true and false negatives, for the calculation of diagnostic accuracy, patients with reactive changes were accepted as false positives. Biopsy samples deemed inadequate or inappropriate by the pathologist were not included in the evaluation.
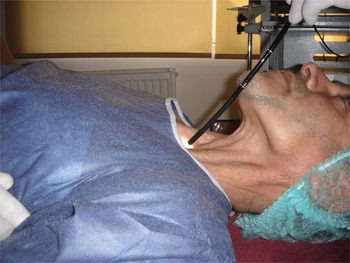
Fig. 3 Bronchoscopy was carried out through the tracheostomy site.
Histopathological analysis
Pathology results were divided into the following six stages, according to the World Health Organization classification of lung tumours: one = normal tissue; two = reactive changes, chronic inflammation, basal cell hyperplasia and squamous metaplasia; three = mild dysplasia; four = moderate dysplasia; five = severe dysplasia or carcinoma in situ; and six = invasive squamous cell carcinoma.Reference Brambilla, Travis, Colby, Corrin and Shimosato25 Stages one and two were evaluated as reactive changes, while stages three to six were evaluated as pre-neoplastic and neoplastic. Of those patients who had undergone biopsy for positive findings during bronchoscopy, those with pre-neoplasia and neoplasia were accepted as true positives, while those with stage one and two lesions were accepted as false positives.
Statistical evaluation
Sensitivity, specificity, positive predictive value and negative predictive value were calculated separately for white light bronchoscopy and autofluorescence bronchoscopy, and also for the combined use of both modalities. Statistical analyses were performed using MedCalc® version 10.4.0 software.
Results
All patients had a history of smoking and had undergone total laryngectomy for squamous cell carcinoma of the larynx, subsequently requiring a permanent tracheostomy. Their mean age was 55.7 years (range 43–74). All patients were male. After the laryngeal operation time to bronchoscopy time was 4.1 months in patients with neoplasia and 4.5 months in all patients. The minimum and maximum intervals between surgery and bronchoscopy were one month and one year, respectively. One patient developed pneumonia two days after bronchoscopy and healed completely with medical treatment. In 11 of the 30 patients, the tracheobronchial system appeared normal on both white light bronchoscopy and autofluorescence bronchoscopy, and no biopsies were taken. In the remaining 19 patients, a total of 27 biopsies was obtained; these revealed invasive squamous cell carcinoma in one patient and pre-neoplastic changes in six.
Eleven patients had pathological bronchoscopic findings on white light bronchoscopy examination, two of whom had positive histological findings (Figure 4). Evaluation of white light bronchoscopy examination alone revealed the following diagnostic parameters: sensitivity 28.57 per cent, specificity 60.87 per cent, positive predictive value 18.18 per cent, negative predictive value 73.68 per cent, positive likelihood ratio 0.73 and negative likelihood ratio 1.17 (Table I).

Fig. 4 Results of white light (WL) bronchoscopy evaluation.
Table I Diagnostic utility of bronchoscopy modes

WL = white light bronchoscopy; AFB = autofluorescence bronchoscopy; sens = sensitivity; spec = specificity; PPV = positive predictive value; NPV = negative predictive value; PLR = positive likelihood ratio; NLR = negative likelihood ratio
Upon autofluorescence bronchoscopic examination, 16 patients had pathological findings and 14 appeared normal. Seven of the biopsies showed positive histological findings (Figure 5). Evaluation of autofluorescence bronchoscopy alone revealed the following diagnostic parameters: sensitivity 100.00 per cent, specificity 60.87 per cent, positive predictive value 43.75 per cent, negative predictive value 100.00 per cent, positive likelihood ratio 2.56 and negative likelihood ratio 0.00 (Table I).

Fig. 5 Results of autofluorescence (AF) bronchoscopy evaluation.
When white light bronchoscopy and autofluorescence bronchoscopy were performed together, 11 of the 30 patients appeared normal and 19 had pathological findings. Biopsy samples obtained from the latter group revealed positive pathological results in seven patients.
Discussion
This study was designed to assess patients who had undergone a total laryngectomy, in order to detect pre-neoplastic lesions at an early stage, and also to assess the role of bronchoscopy as a practical investigative technique in such patients. The study aimed to investigate whether increased diagnostic sensitivity could be achieved by combining white light bronchoscopy, a commonly used diagnostic method, with autofluorescence bronchoscopy, a technique which is gaining popularity due to its greater sensitivity to pre-neoplastic lesions.Reference Lee, Brokx, Postmus and Sutedja26
Patients with squamous cell carcinoma of the head and neck are at high risk of developing squamous cell carcinoma of the lung.Reference Zargi, Fajdiga and Smid27 Chest X-rays and CTs do not have adequate sensitivity to detect early stage neoplasia in such high risk patients.Reference Flehinger, Melamed, Zaman, Heelan, Perchick and Martini28 Furthermore, PET CT is expensive and requires biopsy, and sputum cytology cannot diagnose intraepithelial lesions (studies in high risk patients have shown that sputum cytology is inadequate for detecting pre-neoplastic changes, does not help reduce cancer-specific mortality, and requires further bronchoscopic evaluation and histological examination in patients with atypical findings).Reference Kennedy, Franklin, Prindiville, Cook, Dempsey and Keith29 Therefore, bronchoscopy is the most valuable screening and diagnostic tool for such high risk patients.Reference Vermylen, Pierard, Roufosse, Bosschaerts, Verhest and Sculier30 In addition, bronchoscopic access in such patients may be facilitated by the presence of a permanent tracheostomy.
The sensitivity success of white light bronchoscopy in detecting early neoplastic changes in the central airways is less than 40 per cent.Reference Hirsch, Franklin, Gazdar and Bunn31 However, autofluorescence bronchoscopy is now in widespread use.Reference Palcic, Lam, Hung and MacAulay8, Reference Hung, Lam, Le Riche and Palcic13 Numerous studies have found its sensitivity to be superior to that of white light bronchoscopy.Reference Kennedy, Lam and Hirsch20, Reference Sato, Sakurada, Sagawa, Minowa, Takahashi and Oyaizu32
The sensitivity and specificity of white light bronchoscopy and autofluorescence bronchoscopy change with the number of patients, the number of biopsies and the experience of the bronchoscopist. Fuso et al. assessed the use of bronchoscopy to identify pre-cancerous bronchial lesions, and found sensitivities of 43.8 and 82.8 per cent for white light bronchoscopy and autofluorescence bronchoscopy, respectively, and a positive predictive value of 70.2 per cent for the latter.Reference Fuso, Pagliari, Boniello, Trove′, Varone and Longobardi33 In their multicentre study, Ernst et al. found sensitivities of 28 and 67 per cent for white light bronchoscopy and autofluorescence bronchoscopy, respectively, for the detection of pre-malignant airway change.Reference Ernst, Simoff, Mathur, Yung and Beamis34 Venmans et al. reported a sensitivity of 21 per cent for white light bronchoscopy used to detect bronchial intraepithelial neoplasia, compared with 28.57 per cent in our study.Reference Venmans, van Boxem, Smit, Postmus and Sutedja35 In these latter two studies, the sensitivity figures for autofluorescence bronchoscopy were 57 and 60.87 per cent, respectively. Based on these data, autofluorescence bronchoscopy is a more sensitive technique than white light bronchoscopy in the detection of early neoplasia, and thus should be preferred.
The significance of detecting lesions at an early stage is best illustrated by considering that 10 per cent of moderate dysplasias and 19–46 per cent of severe dysplasias progress to invasive carcinoma within six months, and that 50–60 per cent of squamous cell carcinomas of the lung arise in the central airways and are accessible by bronchoscopy.Reference Hirsch, Franklin, Gazdar and Bunn31 Patients who exhibit long-term survival are those who were diagnosed early and with completely resectable tumours; however, less than 20 per cent of patients have asymptomatic, stage one lesions at the time of diagnosis. Stage zero and one lesions carry the best prognosis; therefore, early diagnosis of lung cancer in high risk patients is critical for patient survival.
• Patients with head and neck squamous cell carcinoma are at high risk of lung cancer
• Such patients require close post-operative follow up even if pre-operative investigations were negative
• In patients with a permanent tracheostomy, bronchoscopy is a simple, comfortable procedure requiring minimum intervention, and is valuable for lung cancer screening
The pre-malignant lesions discussed above are often seen in smokers, and very rarely in nonsmokers.Reference Peters, Morice, Benner, Lippman, Lukeman and Lee36 The risk is 20- to 25-fold higher in individuals with a smoking history of more than one pack per day for more than 20 years.Reference Peto, Darby, Deo, Silcocks, Whitley and Doll37 Thus, it is important to screen heavy smokers (i.e. >20 packs/year), symptomatic smokers and patients with a history of upper respiratory tract cancer. Patients with chronic obstructive pulmonary disease who have smoked more than 40 packs/year have a higher incidence of pre-malignant dysplasia on sputum cytology.Reference Kennedy, Proudfoot, Franklin, Merrick, Saccomanno and Corkill38 Such patients represent an important target population for early diagnosis.
All 30 patients in the present study were heavy smokers, and had undergone total laryngectomy for squamous cell carcinoma of the larynx. Biopsies revealed invasive squamous cell carcinoma of the lung in one patient and pre-neoplasia in six; this total (seven of 30) corresponded to 23 per cent of patients.
Conclusion
Autofluorescence bronchoscopy has greater sensitivity and specificity than white light bronchoscopy in the detection of pre-neoplastic lesions. In patients with a permanent tracheostomy, bronchoscopy is a simple, comfortable procedure which requires minimum intervention, and which is valuable for the screening of patients with cancer of the head and neck and those at high risk of lung cancer. Autofluorescence bronchoscopy shows promise for the detection of pre-malignant changes of the tracheobronchial system in patients previously treated for laryngeal cancer.
These findings need to be supported by larger, multicentre studies.








