Introduction
Hospitals and the public are increasingly interested in the results of medical and surgical treatments provided. Otolaryngology departments in every hospital in Sweden report their retrospective surgical outcomes to a central institution which then publicises them. Our otolaryngology department intends to initiate continuous monitoring of nasal surgery results. This can be done prospectively or retrospectively, subjectively and/or objectively. Prospective scoring is less dependent on memory. Subjective questionnaires tend to be more user-friendly, and objective methods, while less prone to bias, typically require more resources.
Obstruction is a common symptom after nasal trauma. Comparison of subjective and objective measurements of nasal obstruction has yielded conflicting results.Reference Holmstrøm1–Reference Tompos, Garai and Zemplén4 However, subjective methods have increasingly been used in recent years.Reference Morrissey, Alun-Jones and Hill5–Reference Kjærgaard, Cvancarova and Steinsvåg10 A large study comparing subjective ratings of nasal obstruction with objective measures showed strong correlations between the two methods.Reference Kjærgaard, Cvancarova and Steinsvåg10 Other studies have validated the usefulness of subjective methods.Reference Akduman, Yanilmaz, Haksever, Döner and Sayar11, Reference van Spronsen, Ingels, Jansen, Graamans and Fokkens12
Prospective studies of surgical results often have a dual purpose: to monitor the results of current surgical techniques and procedures, and to compare the results of different surgical techniques. An easy-to-use questionnaire that is suitable for both purposes would be ideal. Furthermore, different surgical techniques can influence nasal obstruction differently during the day, at night and during exercise, particularly if supplementary surgery to the conchae is undertaken. Thus, our intention was to evaluate a questionnaire designed to assess nasal obstruction. The questionnaire comprises separate visual analogue scales (VASs) for assessing obstruction during the day, at night and during exercise, with separate Likert scales for assessing other nasal symptoms that may be influenced by surgery.
Materials and methods
This study was approved by the ethical committee of Lovisenberg Diakonale Hospital. Healthy volunteers with a good command of Norwegian language were recruited from different departments at our hospital. Persons with an infection or those seeking medical advice for nasal obstruction at the time of participation were excluded.
The same questionnaire (Figure 1) was presented twice to participants, with a minimum interval of five weeks (in August and October 2013). Participants were unaware that they would be asked to complete the questionnaire a second time. The answers were given anonymously on forms labelled with a study identification number. One person kept a list linking the names and the study identification numbers for the duration of the investigation to ensure that the questionnaires for each respondent could be compared across the two assessments. The list was subsequently destroyed.
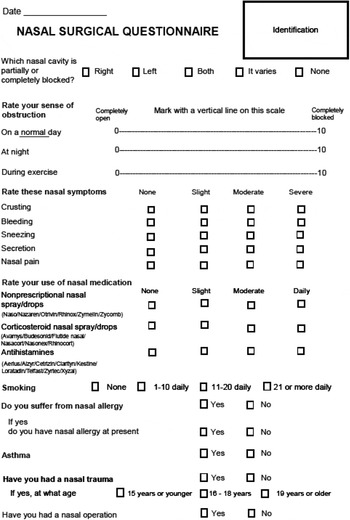
Fig. 1 English version of the nasal surgical questionnaire.
All questions were limited to one page. Respondents rated their subjective sense of nasal obstruction by marking a vertical line on a 10 cm horizontal line. The location of the mark was measured in millimetres, with obstruction scores ranging from 0 (corresponding with ‘completely open’) to 100 (corresponding with ‘completely obstructed’). Separate VAS items were used to assess nasal obstruction during the day, at night and during exercise. Scores were categorised into four groups (as per Lim et al.Reference Lim, Lew-Gor, Darby, Brookes, Scadding and Lund13): none, mild, moderate and severe obstruction. Respondents were also asked if the obstruction occurred on one or both sides, or if it alternated. A four-point Likert scale (with the responses of none, mild, moderate and severe) was used to assess other nasal symptoms (i.e. crusting, bleeding, sneezing, secretion and pain). In addition, we sought information on allergies, smoking habits and nasal medication. Both negative and positive differences in scores between the first and second assessments were given an absolute numerical value.
Statistical analysis
Continuous data are presented as means and standard deviations (SDs), and categorical variables are shown as frequencies and percentages. Group comparisons of VAS scores were performed using the Mann–Whitney U test. The Wilcoxon signed rank test was utilised to estimate the difference in responses between the first and second assessment for the VAS items on nasal obstruction experienced during the day, at night and during exercise. Marginal homogeneity tests were performed to estimate the difference in responses between the first and second assessment for the other nasal symptoms, which were measured on four-point scales. Pearson correlation coefficients were used to estimate associations between VAS scores, and Cronbach's alpha coefficient was used to estimate the internal consistency of the three VAS items. Data were analysed with SPSS software (version 22.0 for Windows; IBM, Armonk, New York, USA). All tests were two-sided, and p values less than 0.05 were considered statistically significant.
Results
Eighty-four volunteers, 41 male and 43 female, were recruited and completed the questionnaire at both the first and second assessments. One male individual responded inconsistently stating that his symptoms were the same on both occasions although he rated them very differently. This was likely to be because of inadequate language skills; this participant was therefore excluded. The age and gender distributions of the remaining 83 volunteers are shown in Table I. A few of the respondents left some of the questions blank. Ten of the respondents were smokers, 12 had a known nasal allergy and 3 reported prior nasal trauma.
Table I Age and gender distributions

Data represent numbers of respondents
Mean VAS scores for nasal obstruction experienced during the day, at night and during exercise at initial assessment are presented in Table II. Mean scores for night-time obstruction were significantly higher than daytime obstruction scores (p < 0.001), but neither were significantly different from exercise obstruction scores. The VAS scores for nasal obstruction during the day, at night and during exercise were highly correlated with one another (r = 0.85–0.93; all p < 0.001), with a Cronbach's alpha coefficient of 0.96. At the initial assessment, 38 per cent of the scores indicated no obstruction (scores of 0), 47 per cent indicated mild obstruction (scores 1–30), 13 per cent indicated moderate obstruction (scores 31–70) and 2 per cent indicated severe obstruction (71–100). The number of respondents in each of the four severity groups and the mean score for each group are also presented in Table II.
Table II Frequency of responses according to nasal obstruction severity

Data represent score frequencies, with mean scores in parentheses
Comparison by gender, analysed using the Mann–Whitney U test, showed that the scores for all three VAS items were statistically higher in males than in females (mean VAS score of 17.47 vs 6.12; p < 0.001). Comparison by allergy status indicated that nasal obstruction scores were higher in those with allergies than in those without allergies (mean VAS score of 28.42 vs 8.55; p = 0.001). Scores were higher, but not significantly, in smokers compared with non-smokers (mean VAS score of 19.10 vs 10.47; p = 0.593). Similar patterns of group differences were observed for VAS scores at the second assessment.
Scores for each VAS item at the initial assessment were highly correlated with the same item at the second assessment (r = 0.84–0.86; all p < 0.001). The mean absolute difference in the VAS scores between the first and second assessment was 5.09 (SD = 7.73) for daytime obstruction, 6.22 (SD = 7.88) for night-time obstruction and 6.38 (SD 8.17) for obstruction experienced during exercise. Wilcoxon signed rank tests indicated that scores for the first and second assessments were not significantly different for any of the three VAS obstruction items (daytime, night-time and exercise).
Stratified analyses were used to examine the mean difference in VAS scores between the first and second assessments within specific subgroups: men and women, allergic and non-allergic persons, and smokers and non-smokers. The analyses did not show any significant differences between the first and second responses to the three VAS items for nasal obstruction in any of the subgroups except for the VAS score at night in allergic persons (35.91 vs 28.45; p = 0.013; Wilcoxon signed rank test). This difference of 7.46, although statistically significant, was clinically small.
Ratings of the other nasal symptoms indicated some small differences between the first and second assessment for sneezing and secretion (Table III), but these were not statistically significant.
Table III Score difference between first and second assessment for secondary outcomes

Data represent numbers of respondents
One person used vasoactive nasal sprays and another used topical steroids on a regular basis. Because of the infrequent use of such medication in this sample, analysis of their effect on ratings of nasal obstruction could not be concluded.
Discussion
We intended the questionnaire to be self-explanatory, and to a large extent it was. However, as seen in this study, it may sometimes be necessary at the pre-surgical consultation to instruct some patients on how to complete the questionnaire. The post-surgical questionnaire will be mailed to the patient, and it would be less practical to provide instructions at that point. In addition, it may be useful to include cross-checking questions to help identify inconsistent responses.
Prior studies evaluating an instrument's test–retest reliability have used intervals of one to two weeks.Reference Stewart, Witsell, Smith, Weaver, Yueh and Hannley14, Reference Bezerra, Padua, Pilan, Stewart and Voegels15 We increased the interval to more than five weeks to overcome the possibility of a recollection of the first response. Even with this longer interval, the questionnaire was shown to have strong test–retest reliability.
The high Cronbach alpha coefficient for the three VAS nasal obstruction items suggests that the instrument has high internal consistency, but indicates that the inclusion of all three items may not be necessary. Given that scores for nasal obstruction experienced during exercise did not differ from the scores for either daytime or night-time obstruction, the exercise VAS item may not be needed. Additional evaluation is needed to determine whether the exercise item is useful among certain subgroups of patients.
The findings of this study provide some evidence of the questionnaire's validity for assessing nasal obstruction. As would be expected, the VAS obstruction scores were significantly higher for allergic persons than non-allergic persons, suggesting that the questionnaire can effectively distinguish between higher and lower levels of nasal obstruction.
Comprehensive quality of life questionnaires such as the Rhinoconjunctivitis Quality of Life Questionnaire and the 22-item Sino-Nasal Outcome Test were designed for rhinitis patients and include many items in the total score. However, obstruction is the major symptom in patients with nasal septal deviation and inferior concha hypertrophy, and reduction of obstruction is therefore the primary objective of surgery. The effect of surgery on this primary symptom may be masked if other symptoms are included in the same scoring. Other nasal symptoms like crusting, bleeding and nasal pain are known side effects of nasal surgery and should therefore be addressed separately in the questionnaire as secondary objectives. We believe that four-point scales are sufficient for this purpose.
The patient is typically used as his or her own control in prospective studies of surgical results. It is therefore not necessary to take into account confounding factors such as the person's age and gender. This study showed no difference in scoring between the first and second assessment, except in allergic individuals' scores for nasal obstruction at night. We consider the size of this difference to be so small that it is clinically unimportant. We realise, however, that allergen exposure may influence nasal obstruction, and thus the questionnaire should preferably be answered outside of the allergy season. If that is not feasible, allergic symptoms need to be taken into consideration.
Visual analogue scales for nasal obstruction (with scores from 0 to 10) have been validated against mild, moderate and severe category scales.Reference Kjærgaard, Cvancarova and Steinsvåg10, Reference Lim, Lew-Gor, Darby, Brookes, Scadding and Lund13 It was found that scores from 0 to 3 were comparable to mild, 3 to 7 to moderate and 7 to 10 to severe obstruction. The scores in the mild, moderate and severe category scales were found to be comparable to the objective methods of peak nasal inspiratory flow and acoustic rhinometry in a study with a large number of patients.Reference Kjærgaard, Cvancarova and Steinsvåg10 A single VAS scale for combined allergic symptoms has been validated for the grading of rhinitis severity in accordance with the Allergic Rhinitis and its Impact on Asthma guidelines.Reference Bousquet, Combescure, Neukirch, Klossek, Méchin and Daures16 It was reported that scores from 0 to 5 corresponded to mild rhinitis while scores from 6 to 10 corresponded to severe rhinitis, leaving the scale scores 5 to 6 undefined.
We believe that it will be simpler to measure changes in the subjective sense of nasal obstruction before and after surgery if continuous VASs are used. The Nasal Obstruction Symptom Evaluation questionnaire has been validated as an organ-specific questionnaire for nasal surgery.Reference Stewart, Witsell, Smith, Weaver, Yueh and Hannley14 It uses a five-point scale for five different ways of observing obstruction. It has been translated into Portuguese and successfully used in Brazil.Reference Bezerra, Padua, Pilan, Stewart and Voegels15 We wanted to focus on the subjective sense of obstruction in three different settings using uninterrupted scales that would be easier to measure.
Other nasal symptoms such as crusting, bleeding and pain may be important sequelae of surgery, but less so than obstruction. A four-point scale was used to assess each of these symptoms, and only minimal differences were seen in the scores for crusting, bleeding and pain. Sneezing and secretion are symptoms of rhinitis and may fluctuate with time and exposure. There was, however, no statistical difference in the scores in this study.
• Nasal symptoms rated on two separate occasions using the nasal surgical questionnaire were consistent
• Differences in mean scores between the first and second assessment of daytime nasal obstruction were small
• Visual analogue scale scores indicated greater nasal obstruction at night, in males and in smokers
• This questionnaire is suitable for prospective quality control assessment of surgery for nasal septal deviation and inferior concha hypertrophy
Based on the results, we believe that our questionnaire is sufficiently inclusive, with scales appropriate for the purpose of quality control of nasal surgery, provided that information on the patient's allergic history and use of medication is taken into account.
Conclusion
A nasal surgical questionnaire, designed for prospective monitoring of nasal septal surgery results, was presented to 83 healthy volunteers twice, with a minimum interval of 5 weeks. It comprises separate VAS items for nasal obstruction experienced during the day, at night and during exercise, and separate four-point Likert scales for the assessment of other nasal symptoms. There was no statistical difference in the responses between the first and second presentation. We believe this nasal surgical questionnaire will be useful in monitoring the results of current procedures and in comparing different surgical techniques.
Acknowledgement
We thank Dr Caryl Gay for reviewing the statistics and for English language editing.






