There is growing evidence indicating that the morphogenesis of the so-called sinus venosus defects derives from the persistence of foetal systemic to pulmonary veno-venous bridges, rather than as an absence of the supposed “party wall” between the right atrium and the right upper pulmonary vein. Reference Butts, Crean and Hlavacek1 We present an unusual left-sided interatrial communication, with associated left-sided partially anomalous pulmonary venous return. To the best of our knowledge, this combination has not previously been reported. It lends further credence to the notion of veno-venous bridges.
Case
A 55-year-old man with a history of atrial fibrillation, embolic stroke, hypertension, hyperlipidaemia and an aneurysmal atrial septum with a possible patent oval foramen, presented with worsening fatigue and dyspnoea at rest. His transthoracic echocardiogram showed mild global hypokinesis of the left ventricle with an ejection fraction of 46%, severe dilation of the right atrium and right ventricle and moderate tricuspid regurgitation. A transoesophageal echocardiogram revealed a severely dilated coronary sinus and a persistent left-sided superior caval vein. A regadenoson stress test revealed normal perfusion of the myocardium.
Gated cardiac computed tomography confirmed the presence of the left-sided superior caval vein, which drained to the right atrium via the coronary sinus. There was no right-sided superior caval vein. The left upper pulmonary vein drained into the left superior caval vein, and thence into the right atrium. The left lower pulmonary vein had a window-like communication with the left superior caval vein prior to connecting normally to the left atrium. Leakage of some contrast into the left atrium across this defect indicated bidirectional shunting. Haemodynamic evaluation by cardiac catheterisation revealed a normal cardiac index of 3.6 L/minute/m2, and a pulmonary-to-systemic flow ratio of 1.8:1. His right ventricular end-diastolic pressure was 12 mmHg. His mean pulmonary arterial pressure was 20 mmHg, pulmonary capillary wedge pressure was 9 mmHg and pulmonary vascular resistance was calculated as 1.3 Woods units.
Given his findings of pulmonary over-circulation and embolic stroke from multiple levels of bidirectional interatrial shunting, surgical repair was undertaken. The preoperative diagnostic findings were confirmed at surgery. There was a concern for baffle obstruction to systemic and pulmonary venous return with attempted redirection of the left pulmonary veins into left atrium across the interatrial communication. Hence, the surgeon decided to anastomose both the left upper and lower pulmonary veins to the left atrial appendage. The resultant large defect in the left superior caval vein was closed with a patch. The patient exhibited symptomatic improvement following surgery.
Discussion
While this case fits the conventional definition of a so-called sinus venosus defect, Reference Oliver, Gallego and Gonzalez2,Reference Al Zaghal, Li and Anderson3 it is unique because the abnormalities were all left-sided. The right-sided superior caval vein was absent, and there were connections between the left lower pulmonary vein and both the left atrium and the left superior caval vein, which continued to drain into the right atrium via the coronary sinus. These findings are all remote from the interatrial septum. These features unequivocally support the concept that veno-venous bridges are the developmental substrate for the so-called “sinus venosus defects”, rather than the absence of a presumed party wall leading to “unroofing” of pulmonary veins. Reference Van Praagh, Carrera, Sanders, Mayer and Van Praagh4 Prior case reports that point to persistent or abnormal veno-venous bridges as the developmental substrate for such defects have been limited by their right-sided location, which places them in proximity to the interatrial septum. Reference Butts, Crean and Hlavacek1,Reference Tretter, Chikkabyrappa and Spicer5
We speculate that such a veno-venous bridge existed initially in our patient between the anterior cardinal vein and the left pulmonary veins. Such connections that are remote from the interatrial septum were previously described as cavopulmonary windows Reference Aramendi, Cubero, Hamzeh and Rey6,Reference Haaf, Kadner, Tabbara and Kessel-Schaefer7 . We favour the term veno-venous bridges, which highlights the essence of these interatrial communications as extracardiac conduits with potential for bidirectional shunting. Reference Anderson8
A high degree of suspicion is required to appreciate the morphological and physiological implications of veno-venous bridges. Our patient presented with dyspnoea and embolic stroke due to interatrial communications that were not apparent on an echocardiogram. To enhance the diagnostic accuracy of transthoracic echocardiography in such unusual anomalies that lead to right heart dilation, one must keep in mind the potential for pre-tricuspid shunts distant from the interatrial septum. We suggest a lower threshold to employ multiplanar imaging with either resonance imaging or computed tomography, and use of three-dimensional rendering in order to optimise diagnosis and management. Reference Hansen, Duong and Jivanji9

Figure 1. Three-dimensional volume-rendered image by CT angiography: ( a ) Coronal section from the anterior showing left upper pulmonary vein (LUPV) draining into left superior caval vein (LSCV). ( b ) Left lower pulmonary vein (LLPV) communicated with the left superior caval vein just above its junction with the coronary sinus (CS) and continues to connect with the left atrium (LA).
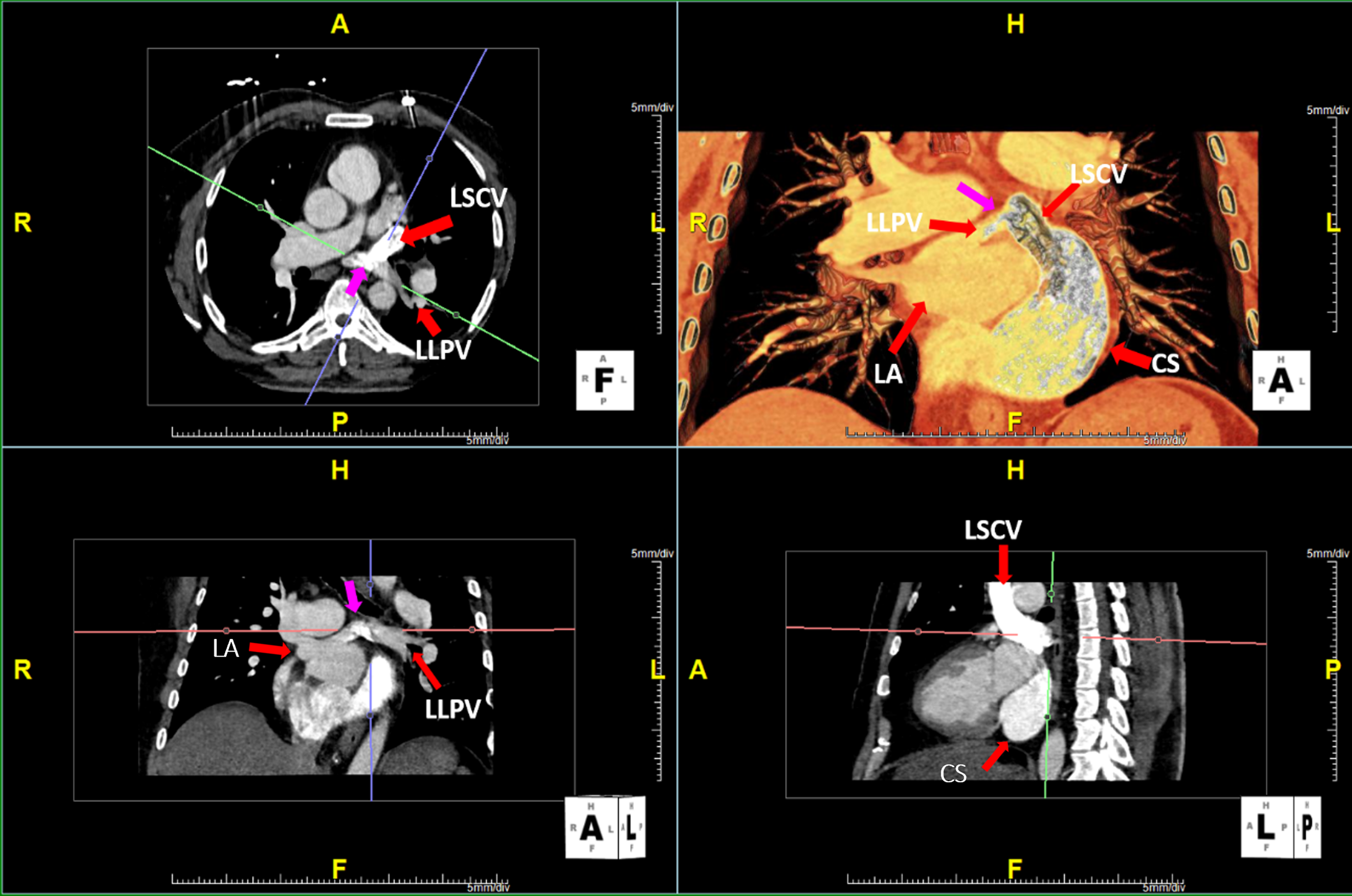
Figure 2. Multiplanar imaging reveals a tunnel-like interatrial communication (denoted by pink arrow) between the left lower pulmonary vein and the left superior caval vein. There is leakage of contrast into the left lower pulmonary vein before it connects to the left atrium (LA), suggesting bidirectional shunting.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
Patient data has been anonymised.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1047951121004315





