Introduction
Radiotherapy is central to the management of breast cancer with the aim of delivering a radiation dose to the target volume, while sparing the surrounding healthy tissues. Traditionally, breast cancer patients have been treated supine with one or both arms abducted above the head, lifting the breast tissue in the cranial and anterior direction. Reference Chen, Cheng, Kuo, Chan, Huang and Chen1–Reference Mulliez, Gulyban and Vercauteren5 This position is generally considered to be appropriate, comfortable and reproducible and allows for a range of gantry angles and clear visualisation of the treatment beams. Reference Chen, Cheng, Kuo, Chan, Huang and Chen1,Reference Bartlett, Colgan and Donovan6 Challenges, however, can be encountered when patients have large and/or pendulous breasts, as deep infra-mammary folds and/or lateral wrap skin folds around the chest wall, beyond the mid-axillary line, can occur. Without effective immobilisation, it can be difficult to meet set dose constraints, radiation-related toxicity can be increased and worse cosmetic outcomes have been reported. Reference Ferrari, Ivaldi, Leonard, Rondi and Orecchia2–Reference Morrow, Stepaniak, White, Wilson and Li4,Reference Jain, Marchant and Green7 Given the increasing incidence of breast cancer, the high number of patients referred for breast conserving surgery, the associated decrease in skin elasticity in our aging population and the higher average body mass index (BMI) of patients generally, refinements in breast immobilisation techniques are warranted. Enhancements to breast immobilisation techniques would not only help optimise the therapeutic benefit for post-lumpectomy radiotherapy but might also greatly enhance efficiency and improve the overall patient experience in busy, modern day, radiotherapy departments.
Immobilisation of the large and/or pendulous breast for external beam radiotherapy
To categorise the breast as ‘large’ in the context of external beam radiotherapy is to merely witness the creation of an infra-mammary skin fold when the patient is lying supine on a horizontal table with both arms abducted above their head. A pendulous breast will also create skin folds inferiorly and/or laterally when the patient is similarly positioned. From experimental observation in women with a BMI, in the normal range, a large breast might be defined as a volume of greater than 1100 cc or requiring a G-cup (UK sizing) bra or larger and where the infra-mammary skin fold does not disappear when the patient lies flat and raises both arms above their head.
Supine positioning is often achieved with the addition of an angled breast board (Figure 1), the angle of which is designed to assist radiotherapy field matching. The raising of the head and shoulders in this regard also tends to encourage the creation of the infra-mammary skin fold. An immobilisation technique that could eliminate the fold would be advantageous, and one seemingly logical means of achieving this is to position the patient prone on a specially constructed prone board (Figure 2).
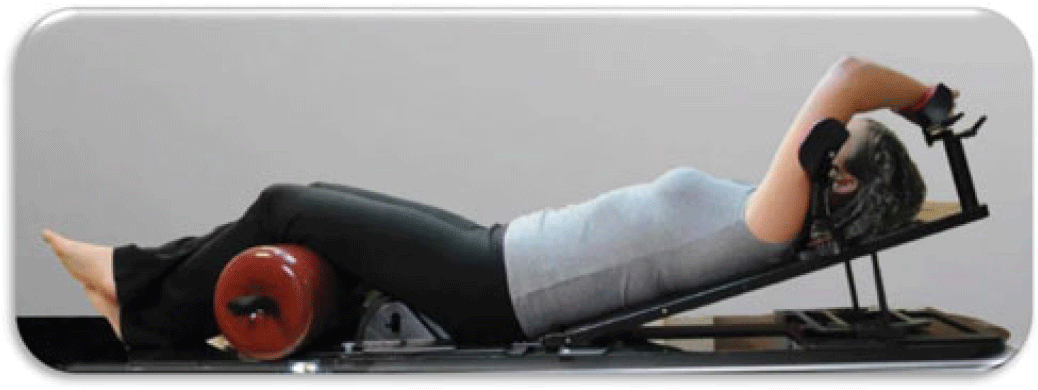
Figure 1. Supine positioning on Quest breast board (permission granted by Oncology Imaging systems for use of the photograph).

Figure 2. An example of prone positioning (permission granted by Orbital Therapy for use of the photograph).
The use of prone patient positioning for breast radiotherapy to reduce radiation-induced toxicity in women with large and/or pendulous breasts has gained momentum internationally in recent years. This is largely due to a favourable toxicity profile in terms of lung, skin and heart doses compared to the supine positioning techniques Reference Chen, Cheng, Kuo, Chan, Huang and Chen1,Reference Buijsen, Jager and Bovendeerd8–Reference DeWyngaert, Jozsef and Mitchell11 together with improved dose homogeneity within the breast volume. Reference Merchant and McCormick12
In 2012, Bergom et al. Reference Bergom, Kelly and Morrow9 conducted a study of 109 patients who were treated prone with whole breast irradiation (WBI) using 3D-conformal radiotherapy, the majority of whom had large and/or pendulous breasts, with 80% of patients having breast volumes of ≥1000 cc. Based on the Harvard Scale for cosmetic outcomes, the majority of patients (89%) had good or excellent cosmetic outcomes with favourable overall toxicity profiles.
In the same year, Lymberis et al. Reference Lymberis, Dewyngaert and Parhar10 conducted a dosimetric analysis of the first 100 patients accrued to their trial where each patient was planned in both a supine and prone position. A supine position was used with no additional immobilisation, and the prone position was on a specially designed prone board with 60% of all patients having a breast size of >750 cc. For all patients, the prone position reduced the amount of lung irradiated and reduced the heart volume irradiated in 87% of left breast cancer patients.
Verhoeven et al. Reference Verhoeven, Sweldens and Petillion13 also conducted a comparative trial of 34 patients in three positions: supine free breathing, supine with gating in deep inspiratory breath hold (DIBH) and prone positioning. They also concluded that the lowest doses to the lungs were achieved in the prone position but found the heart and contralateral breast were best spared in the supine position with gating in DIBH.
While there is evidence that there can be potential dosimetric and cosmetic benefits with the prone position, the stability of the prone position is vital to ensure both inter-fractional and intra-fractional reproducibility. One of the larger comparative studies of supine versus prone positioning was conducted by Mulliez et al. Reference Mulliez, Gulyban and Vercauteren5 who retrospectively analysed cone beam computed tomography (CBCT) set-up data of 242 patients receiving supine and prone WBI. Results indicated that set-up accuracy was generally poorer in the prone position and the treatment sessions were longer as daily CBCT was deemed necessary to guarantee the correct roll of the patient and to avoid unintended irradiation of the contralateral breast.
Conversely, Stegman et al. Reference Stegman, Beal, Hunt, Fornier and McCormick14 carried out a retrospective analysis of 245 patients and reported that the prone technique was reproducible and well tolerated although 2 patients did experience rib fractures as a result of being positioned on the prone board.
A randomised trial conducted by Kirby et al. Reference Kirby, Evans, Helyer, Donovan, Convery and Yarnold15 compared the feasibility, set-up errors and respiratory motion for a supine breast radiotherapy technique compared with prone positioning in patients who had a cup size ≥C (UK sizing). In the study, it was reported that although the prone technique reduced anterior chest-wall motion, it was associated with larger set-up errors. The reasons postulated for the increased set-up errors included patient factors, such as body habitus and seroma shrinkage and staff unfamiliarity with the prone breast radiotherapy technique.
One of the few randomised trials to include additional immobilisation in the supine position was a study by Varga et al., Reference Varga, Hideghéty, Mező, Nikolényi, Thurzó and Kahán16 which compared repositioning accuracy of prone positioning against their supine technique that included a five-point shell fixation moulded around the chin, the neck, the thorax and the abdomen for breast cancer patients. Good positioning accuracy was reported for both positioning techniques, but an overall trend for superior positioning accuracy in the supine position was noted. Positioning accuracy in the prone position improved over time, which the authors stated indicated the need for more experience and expertise with prone positioning techniques.
Evidence to support the adoption of a prone technique in order to eliminate the skin fold remains less convincing than first predicted. Although benefit has been reported with regards to reduced heart and lung dose, the argument to adopt a prone positioning technique is less attractive when you consider the reports of increased treatment slot times, the difficulties encountered by less agile patients mounting prone positioning systems and the report, albeit infrequent, of rib fractures. When using a prone positioning system on top of the treatment couch, the patient’s centre of gravity is raised higher than the isocentre height of the treatment room, which can create moving and handling challenges for therapeutic radiographers. That daily imaging is reportedly necessary in order to guarantee that treatment set-up accuracy is a further consideration although many studies also indicate that the unfamiliarity with the prone positioning technique may be the contributing factor for the reliance on imaging assurance during set-up. This concern would surely lessen if a prone positioning technique was adopted and in regular use in a radiotherapy department. It appears that a lack of experience with the positioning of patients in the prone position could be an obstacle to fully assessing the reproducibility of the technique.
In order to inform the debate, a survey of current practice in radiotherapy centres in the United Kingdom and Republic of Ireland (RoI) was undertaken. The aim was to evaluate the immobilisation techniques used during external beam breast irradiation for patients with large and/or pendulous breasts in order to inform best practice.
Methods
A survey was distributed to 74 radiotherapy centres in the United Kingdom and RoI during December 2018 in order to determine the immobilisation techniques being adopted. A regional radiotherapy department manager distributed the request and survey to radiotherapy service managers within the United Kingdom via a Google group e-mail and followed up with a reminder e-mail to those who did not response 2 weeks after the initial contact. A sample of the survey content is shown in Table 1. The survey was also e-mailed directly to Radiotherapy Managers in the RoI and again a follow-up email used as a reminder 2 weeks later. Twenty-six completed surveys were received and reviewed for the purpose of the study—a 35% response rate.
Table 1. Survey questions
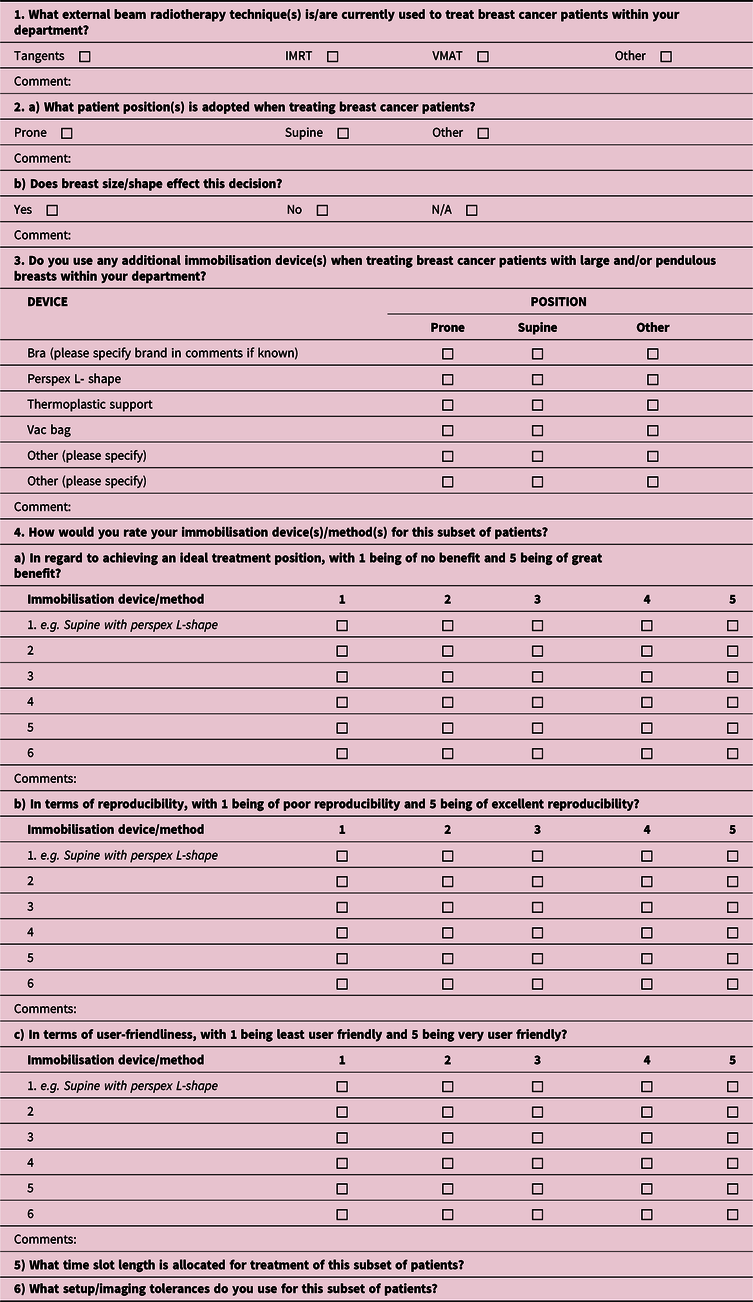
VMAT, volumetric-modulated arc therapy.
Survey findings
Figure 3 summarises the methods/devices used for immobilisation and quantifies their popularity. The outcome measures of Effectiveness, Reproducibility and User-friendliness [E, R, U] ratings are wholly subjective, and only in instances where a single department utilises more than one technique might, any sense of comparison, be made. Effectiveness, reproducibility and user-friendliness rating scores, when comparisons are possible, are demonstrated in square brackets. The best possible rating being [5, 5, 5] and the weakest being [1, 1, 1] for the outcome measures in respective order, namely, [Effectiveness, Reproducibility, User-friendliness]. The results of the survey demonstrate that supine positioning is the most commonly employed patient position for this subgroup of patients in the United Kingdom and Ireland with only two respondents reporting the use of a prone positioning technique.
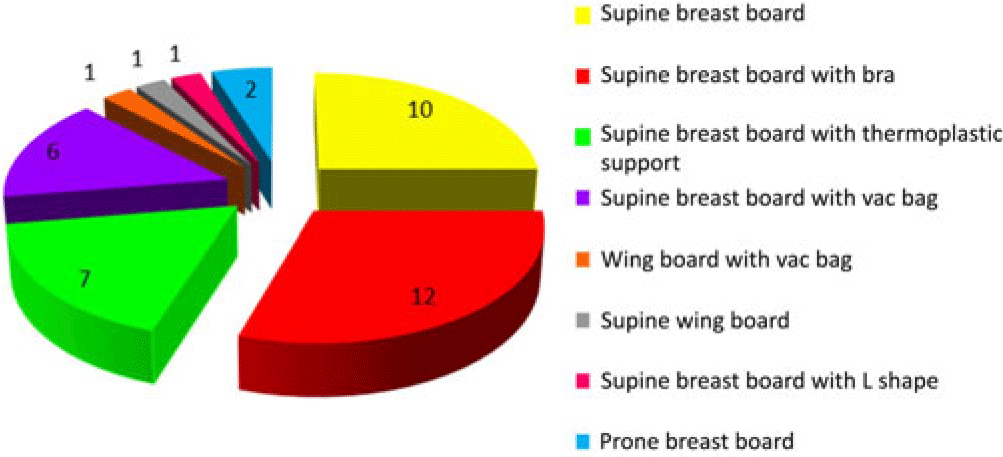
Figure 3. The immobilisation methods/devices used during external beam radiotherapy for breast cancer patients with large and/or pendulous breasts. The 26 radiotherapy centres that responded to the survey utilise a total of forty immobilisation methods/devices between them.
Supine breast board
Ten centres reported the use of a supine breast board without a bra. For six, this was the only method used. For the remaining four, the respondents all rated the supine breast board without a bra as better than alternatives.
Supine breast board with bra
In the centres that reported the adoption of a bra in the supine position on a breast board, most described the use of the patient’s own, non-underwired, bra. One centre commented that the reproducibility of the set-up with the patient’s own bra very much depended on the quality of the bra in terms of its fit and support. Two centres recommend to the patients’ what bra type they might purchase for use during radiotherapy. The popularity of bras for immobilisation is clear from the survey responses with one centre recommending the use of a commercially available bespoke radiotherapy bra.
Supine breast board with thermoplastic support
Utilisation of a thermoplastic support device was reported by seven centres with three of the seven also employing the use of additional immobilisation methods. One of the three rated the thermoplastic support better in all three outcome measures than the use of a bra, while the other two rated it poorer in comparison to the use of a vac bag.
Supine breast board with vac bag
One centre reported the use of vac bags alone for immobilisation and rated it [3, 3, 3] for the outcome measures. The three remaining centres that reported the use of vac bags all indicated that they were used infrequently for specific cases. Three centres use both vac bags and bras: first, Vac Bag [3, 4, 4] and Bra [4, 4, 3], second, Vac Bag [3, 4, 3] and Bra [4, 4, 5], and the third did not rate the device due to its very sporadic use. One centre noted that the vac bag increases the risk of gantry collision during treatment set-up.
Wing board with vac bag
One centre reported the use of a wing board with vac bag [5, 5, 5] and additionally utilised two alternative methods: thermoplastic support [4, 4, 3·5] and supine board [5, 5, 5].
Supine wing board
The use of a wing board was reported by one centre for patients who have a high BMI exceeding the weight limit of the breast board. They scored the use of the wing board [3, 3, 4].
Supine breast board with L-shape
The use of an L-shape was reported by one centre and rated [3, 3, 4].
Prone breast board
Two out of the twenty-six respondents reported the use of prone positioning with one centre using a prone technique alone, while the other employs a combination of methods for immobilisation, namely, supine with a bra, supine on a QFix board and prone positioning.
The centre that reported the use of prone positioning alone commented that they had previously used a bra technique but found it to be very unreproducible with treatment time slots becoming unmanageable. They rated their prone technique very favourably [5, 5, 5], the maximum for all three outcome measures.
Paradoxically, the centre that adopts a variety of positioning techniques rated the bra [5, 5, 5] but the prone technique [3, 4, 4]. They also commented that while the prone technique is reasonable in terms of reproducibility, it requires additional time for patient set-up and manual handling at a higher table position. Subsequently, they typically allocate 15-minute treatment slots for patients on the supine board with or without the addition of a bra and 25 minutes for the prone breast technique. Additionally, they reported imaging on days 1–3 and then weekly for the supine technique but daily for the duration of the prone technique using kilovoltage (kV) imaging with online correction.
Limitations
The survey set out to determine the kind of immobilisation techniques currently being adopted in radiotherapy centres in the United Kingdom and RoI. Figure 3 summarises the findings. The additional feedback elicited under outcome measures ‘Effectiveness, Reproducibility, User-friendliness’ is entirely subjective and merely a vehicle to encourage discussion and understanding. The survey did not specify who in the department might complete the same, the breast cancer specialist being an obvious choice, but it might have been completed by any staff member or the radiotherapy manager. The cross-section of radiotherapy centres represented is modest yet not unrealistic yielding a 35% response rate. Clearly large gaps exist in the survey results.
Discussion
Despite radiotherapy being central to the management of breast cancer, developments in effective breast immobilisation appear slow. This is perhaps somewhat due to the simplicity of the long-established supine wedged tangential pair treatment method. Application of advancing treatment techniques in breast irradiation, intensity-modulated radiotherapy and arc techniques, combined with the move towards hypofractionated treatment schedules and accelerated partial breast irradiation, has more recently, however, driven the need to explore how set-up accuracy and reproducibility can be improved in order to optimise dose delivery. These advancing treatment methods result in inhomogeneous dose distributions and sharp dose gradients between the target tissue and organs at risk (OARs) Reference Mulliez, Gulyban and Vercauteren5 and, therefore, warrant a high degree of daily positional confidence to avoid a geographical miss. Reference Offerman, Lamba and Lavigne17 In addition, patients are now living longer to experience the long-term side effects caused by radiation doses received by OARs and any potential misadministration of prescribed dose. Reference Bartlett, Colgan and Donovan6 Therefore, it is vital that robust systems are in place to ensure that a high therapeutic ratio is achieved. Despite all this, there appears to be no universal consensus as to how patients should be immobilised for breast irradiation, particularly those with a large and/or pendulous breast volume.
A major advantage of the utilisation of bras for breast irradiation immobilisation is that they can be easily integrated into already established supine treatment techniques with minimal modification to protocols and prove compatible for nodal irradiation. Reference Arenas, Hernández and Farrús18 Additionally, they are reported as being comfortable and well tolerated by patients at the centres in the United Kingdom and Ireland that use this form of immobilisation. In addition to effective immobilisation, the wearing of a bra might also serve to improve patient dignity by creating a less vulnerable arrangement than being naked from the waist up. That said, consideration might also need to be given to the potential reduction in skin sparing created by placing support structures over the surface of the breast. It would defeat the purpose of attempting to reduce radiation-induced skin toxicity in skin folds if the very immobilisation method used shifted the risk to other surfaces of the skin. This might particularly be an issue with the use of the thermoplastic support among others.
Over the past number of years, there has been growing interest in the use of prone positioning for breast irradiation. Some advocate that it could improve some of the technical limitations faced when treating breast cancer patients, in particular those with a large breast volume or who have pendulous breasts. Reference Chen, Cheng, Kuo, Chan, Huang and Chen1,Reference Ferrari, Ivaldi, Leonard, Rondi and Orecchia2,Reference Morrow, Stepaniak, White, Wilson and Li4,Reference Varga, Hideghéty, Mező, Nikolényi, Thurzó and Kahán16,Reference Jozsef, DeWyngaert, Becker, Lymberis and Formenti19 Nevertheless, despite favourable literature on prone positioning and its widespread use for decades in diagnostic radiography, its adoption in radiotherapy appears limited. This is likely largely due to the reproducibility of the technique and its set-up accuracy remaining a subject for debate. Reference Chen, Cheng, Kuo, Chan, Huang and Chen1,Reference Krengli, Masini and Caltavuturo3–Reference Bartlett, Colgan and Donovan6,Reference Varga, Hideghéty, Mező, Nikolényi, Thurzó and Kahán16,Reference Arenas, Hernández and Farrús18,Reference Jozsef, DeWyngaert, Becker, Lymberis and Formenti19 Other reasons possibly contributing to this are that a change from supine to prone positioning would involve equipment procurement, extensive staff training and protocol revision. Reference Krengli, Masini and Caltavuturo3 Furthermore, increased time slot duration would be likely during the induction phase and perhaps thereafter, if daily imaging is deemed to be required to ensure positional accuracy. Reference Krengli, Masini and Caltavuturo3,Reference Mulliez, Gulyban and Vercauteren5–Reference Jain, Marchant and Green7 Additionally, manual handling issues associated with positioning patients at a higher height was identified by one of the responding centres that employs a prone technique.
It has been suggested that regardless of the positioning technique adopted some form of image guided radiotherapy should be employed to optimise set-up precision in both positions Reference Krengli, Masini and Caltavuturo3–Reference Mulliez, Gulyban and Vercauteren5,Reference Bergom, Kelly and Morrow9,Reference Kirby, Evans, Helyer, Donovan, Convery and Yarnold15,Reference Varga, Hideghéty, Mező, Nikolényi, Thurzó and Kahán16,Reference Arenas, Hernández and Farrús18–Reference Fatunase, Wang and Yoo20 as any dosimetric advantages that are obtained through advanced treatment techniques or prone positioning are of no clinical benefit if precise treatment delivery cannot be guaranteed. The optimal method of image-guidance in breast radiotherapy remains unclear. The role of CBCT has been questioned due to its additional associated dose, imaging/gantry clearance limitations and the additional time required for imaging Reference Kirby, Evans, Helyer, Donovan, Convery and Yarnold15,Reference Varga, Hideghéty, Mező, Nikolényi, Thurzó and Kahán16,Reference Arenas, Hernández and Farrús18–Reference Fatunase, Wang and Yoo20 . The use of digital tomosynthesis as an alternative method of obtaining three-dimensional (3D) soft tissue images from the on-board imaging unit (obtained in partial rotations) has been suggested by Fatunase et al. Reference Fatunase, Wang and Yoo20 . Additional alternative technologies advocated include implant-transponder systems or dosimeters and opto-electronic surface imaging. Reference Kirby, Evans, Helyer, Donovan, Convery and Yarnold15,Reference Fatunase, Wang and Yoo20 Further research into the use of these suggested verification technologies would aid decision-making regarding which is most suitable for various clinical situations including the management of large breast volumes.
Conclusion
Several methods and devices are available to aid the immobilisation of patients with large and/or pendulous breasts, and no one technique has gained widespread acceptance over the others for use in external beam radiotherapy. The survey throughout the United Kingdom and Ireland has identified eight different immobilisation methods/devices in current use. The utilisation of prone positioning appears much less common than what might have been expected and seemingly for justifiable reasons. Consideration must be given to the workflow in already overburdened radiotherapy departments with protocols also prioritising optimal patient comfort and dignity.
Further analysis of set-up accuracy and reproducibility of immobilisation methods through large multi-centre randomised control trials comparing prone with supine techniques with additional immobilisation would greatly inform decision-making. In addition to the technical effectiveness of immobilisation techniques, service user evaluation to establish the patient perspective should be integral to future work.
Acknowledgements
The authors thank the staff of the radiotherapy department, Belfast Health and Social Care Trust, for their help and support.
Financial Support
This review received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
None.







