When Hurricane Harvey made landfall along the Texas coast on August 25, 2017, as a Category 4 storm, it was predicted to be one of the worst natural disasters in American history. 1 An estimated 1 trillion gallons of water poured onto Harris County over a 4-day period, resulting in massive flooding that affected at least 120,000 structures. 2 Thirty-six lives were lost and tens of thousands of residents were displaced. On August 29, Harris County and community partners set up a 10,000-bed megashelter at NRG Center. Harris County Public Health (HCPH) was responsible for monitoring the health status of residents and preventing communicable disease outbreaks within the megashelter. Despite the prolonged 20-day active response, an early seasonal influenza outbreak was identified and quickly contained. This analysis aims to describe the multifaceted approach utilized to identify this outbreak and implement control measures, discuss challenges encountered and successes achieved in the surveillance and response, and make recommendations for future emergency response.
METHODS
Surveillance efforts at NRG shelter included data abstraction from patient visits to on-site clinics and pharmacies as well as nightly cot-to-cot resident health surveys that assessed symptoms including fever, cough, sore throat, vomiting, and diarrhea. On a daily basis, HCPH epidemiologists reviewed medical records in on-site clinics and pharmacies to abstract information such as diagnoses, chief complaints, tests and prescriptions ordered, and vaccines administered. The clinics and pharmacies were asked to report communicable diseases promptly for implementation of immediate control measures if necessary.
Cot-to-cot surveys were conducted every evening at 6 pm with an online tool to collect information from residents including symptoms, medical visits and reasons, vaccine history, and demographics. The online tool was a mobile phone–based questionnaire designed by HCPH epidemiologists that utilized the commercially available survey software Qualtrics® and was downloaded onto surveyors’ mobile phones for data entry during interviews. Survey teams comprised staff from HCPH and student volunteers from local universities and were led by epidemiologists. To ensure data quality and communicate daily dynamics, a nightly just-in-time training was required for these teams prior to surveys, and a debriefing session was conducted afterwards. No statistical sampling was performed during surveys; each team aimed to reach all households in their designated shelter area to collect data. The head of household was interviewed for the entire family to answer survey questions. If symptoms of a communicable disease were identified, an epidemiological consultation followed in which more specific questions regarding the illness were asked; in addition, the epidemiologist determined whether further action was needed such as clinic referral and/or isolation. The family of the ill person was also assessed to determine whether others were ill. All individuals exhibiting communicable symptoms were placed in isolation rooms away from other evacuees. One of the 3 isolation rooms in clinic areas was designated for respiratory illnesses.
In addition to isolation, multipronged control measures were carried out to confine and prevent disease spread, including enhanced environmental inspections and cleaning, frequent hygiene education, readily available hand sanitizers, 24-hour on-site vaccination, and prompt treatment as warranted.
Cases were diagnosed using either (1) a Clinical Laboratory Improvement Amendments (CLIA)-waived, commercial rapid antigen detection test or (2) reverse transcription–polymerase chain reaction (RT-PCR) influenza subtype testing performed at a public health laboratory using standardized US Centers for Disease Control and Prevention polymerase chain reaction reagents.
Confirmed cases were defined as influenza-like illness (ILI) (fever ≥100°F, cough and/or sore throat without another known cause) plus positive influenza test by rapid assay, polymerase chain reaction, or culture. Probable cases were defined as ILI with an epidemiological link to a probable or confirmed case but without test confirmation. 3
Collected data were stored on a secure network server and frequencies and percentages were analyzed daily to monitor disease trends and symptoms throughout the operation time period.
RESULTS
The NRG megashelter housed 3365 evacuees at its peak and 7409 persons cumulatively during the 3 weeks of operation. During the 20 days of active surveillance, a total of 3606 household health surveys and 395 epidemiological consultations were completed.
On September 6, an on-site clinic notified HCPH of a shelter resident with ILI who tested positive for influenza A by rapid assay. Treatment of Tamiflu was initiated, and the individual was placed in isolation immediately. In the following 2 days, 6 additional ILI cases were identified with onset dates ranging from September 3 to 6. As presented in Figure 1, these cases were dispersed throughout Single Men’s Unit (1 case), Single Women’s Unit (2 cases), and Family Unit (4 cases). An influenza outbreak surfaced. As a result, HCPH intensified surveillance and control measures. Epidemiologists visited on-site clinic areas at each shift to seek out residents experiencing ILI symptoms and monitored the respiratory isolation room in coordination with clinic staff to ensure that patients were in compliance with isolation protocols until at least 48 hours after the initiation of antiviral treatment. During the outbreak, 15 individuals were isolated for a duration ranging from 1 to 4 days.
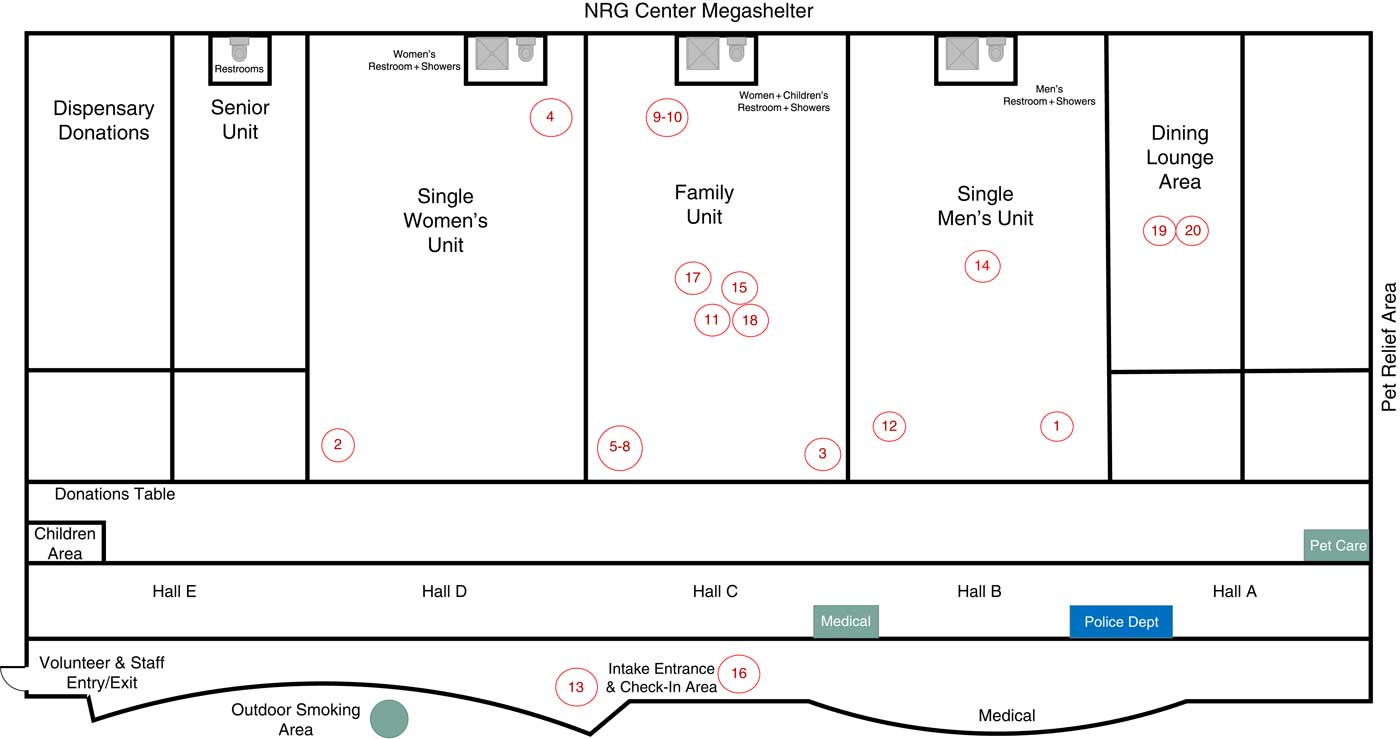
Figure 1 Locations of Identified Flu Cases at NRG Megashelter, September 2017
Hand sanitizers were widely distributed throughout the shelter areas, and environmental cleaning and disinfections were conducted several times a day. Robust communication efforts including large and ubiquitous signage and messaging for flu prevention were placed throughout NRG. Multilingual public address announcements regarding the outbreak were made twice per day, emphasizing hand hygiene and cough etiquette and encouraging on-site influenza vaccination and early treatment if ill. Antiviral medications including oseltamivir were supplied in on-site pharmacies and tracked by the HCPH surveillance team to ensure sufficient quantity for on-site dispensing. A total of 771 free vaccinations were administered on site for residents and shelter staff.
Fifteen throat swab specimens were collected and sent to a public health laboratory for RT-PCR confirmatory testing and to assess epidemiological linkage, which resulted in the identification of influenza A (H3) in 14 of the swabs.
Ultimately, 20 individuals were identified with confirmed influenza: 19 with influenza A and 1 with influenza A/B (Figure 2). Of these, 14 cases were confirmed by RT-PCR tests and 6 were confirmed by rapid tests. Cases were located in all units except the Senior Unit, which was not occupied. Twelve of the 20 individuals with confirmed influenza were male; 3 were younger than 5 years, 1 was younger than 2 years, 1 was older than 65 years, and 4 were shelter staff. It is notable that 5 of these individuals had recently received an influenza vaccine. Symptoms included fever (100%), cough (80%), sore throat (45%), running nose (50%), diarrhea (15%), and vomiting (25%). Twenty percent of the individuals with confirmed influenza reported having at least 1 chronic medical condition. All patients received Tamiflu except for 1 that was lost to follow-up. One patient was transferred to a hospital because of severe diarrhea and vomiting; fortunately, no deaths occurred. No probable cases were identified, and no new cases were identified after September 16 until the last day of shelter operation on September 22.

Figure 2 Epi Curve of Identified Flu Cases at NRG Megashelter, September 2017
DISCUSSION
Disasters cause dense crowding of evacuees in shelters, which creates environments conducive to transmission of infectious diseases. Diseases, including those caused by respiratory pathogens, are not uncommon in evacuee sheltersReference Figueroa, Gulati and Rainey 4 - Reference Watson, Gayer and Connolly 8 and could lead to secondary public health emergencies and even loss of life. Therefore, public health surveillance and response are critical to protect displaced individuals from additional suffering. The risk factors contributing to respiratory outbreaks in shelters include crowding, poor sanitation and ventilation, lack of access to health care, low vaccination rates, and mixed baseline health status of the displaced population.Reference Watson, Gayer and Connolly 8 , 9 Although the NRG dormitory was spacious and well air-conditioned and access to medical services was readily available, the large number of evacuees, lengthy operation, high mobility, and mixed baseline health status of the population posed challenges for public health surveillance. The survey data showed that 80% of evacuees had not been vaccinated for seasonal flu before arriving the shelter, and 45% were on prescription medications. Approximately 3% of the evacuees were homeless prior to the hurricane.
Disease surveillance in large evacuation shelters can be challenging,Reference Waring and Brown 7 – Reference Lee, Palacio and Shah 11 and the NRG megashelter was no exception. Challenges generally related to the scope and magnitude of the response, coordination with multiple agencies at different levels simultaneously, lack of predesigned survey tools, relatively new staff without previous disaster response experience, quick turnover in surveillance teams and on-site medical staff, and simultaneous management of multiple surveillance activities outside of the NRG shelter. Personal hurricane-induced losses experienced by HCPH staff also impacted response efforts. Additionally, ILI and other communicable symptoms were not screened at intake at the beginning of the response, which might have aided early detection of source infections. Furthermore, surveys were initially conducted using paper questionnaires, which required substantial data entry and personnel time and thus hindered the surveillance process. Lastly, the possibility of adjusting air exchange in the dormitory to increase ventilation was not explored during the outbreak response, which could be an area of improvement for future emergencies.
To overcome these obstacles, HCPH streamlined coordination with partners in the shelter to improve the surveillance and response. Screening of ILI and gastrointestinal symptoms was incorporated into the intake process and ill evacuees received epidemiological consultations and after-action interventions immediately. An online survey tool was quickly developed to replace paper forms, which expedited daily assessments and allowed for flexibility to modify survey questions as the situation evolved. Just-in-time training was adjusted to reflect changes in the surveillance process.
HCPH also coordinated with the Incident Command System in place to ensure adequate staffing for surveillance and response teams. Communications and environmental health strategies were also emphasized to ensure appropriate prevention and response coordination. Although there was no indication that surveillance activities could have contributed to the outbreak, shelter staff were required to enhance hand hygiene and take other measures to prevent potential transmission among evacuees. With this multifaceted, rigorous approach, despite substantial challenges faced and longer-than-expected operations in the densely populated megashelter, rapid detection of the outbreak and interventions aided in limiting transmission of influenza in the shelter and further spread to the community.
CONCLUSION
Future emergency response preparation should include preparing for influenza outbreaks in large evacuation shelters in large-scale disaster settings. A holistic approach consisting of coordinated partnerships with onsite agencies, robust communications and health awareness strategies, predesigned survey tools, trained staff, enhanced isolation and hygiene practices, and sufficient vaccine supply is essential for successful disease identification and control.
Acknowledgements
We would like to acknowledge the following people and entities for their contributions to the NRG surveillance: HCPH staff: Sherrill Pirsamadi, LVN; April Beeks, MPH; Sarah Milligan, MPH; Erika Olsen, MPH; Elya Franciscus, MPH; Natasha Wahab, MPH; Delisabel Lopez, PhD, MPH; Lyndsey Hassmann, MPH; Deborah Bujnowski, PhD, MPH, RD; Martina Salgado; Norma Arcos; Amanda Nguyen; Vishaldeep Sekhon, MPH; Rebecca Rubinstein, MPH; Richard A. Williams; Valeria Brannon, RN, MSN; Ashley Minkeu, MPH; Masihullah Noori. Samantha Solomon, Public Health Associate, US Centers for Disease Control and Prevention; The University of Texas Health Science Center at Houston School of Public Health, Student Epidemic Intelligence Society; Ann Malecha, PhD, RN, Texas Woman’s University; student nurses, Texas Women’s University College of Nursing; Susan Tortolero Emery, PhD, The University of Texas Health Science Center at Houston School of Public Health. Houston Health Department Laboratory Services; Harris County Medical Society Urgent Care Clinic and Pediatric Urgent Care; Baylor College of Medicine, Harris Health Same Day Clinic and Mental Health Clinic; Baptist Child and Family Services; Walgreens and CVS on-site clinics.




