Introduction
Binocular vision utilising a microscope for improved visualisation while performing otological surgery, first developed in 1952, offers a plethora of advantages, such as ambidextrous hand mobility and a clear view of the middle-ear anatomy except for the retrotympanic space.Reference Nylean1 Since its initial employment, the microscope has been established as a powerful instrument for treating the majority of middle-ear lesions. Alternatively, endoscopic ear surgery, first described by Ohnsorge in 1977, offers a more transparent view of the middle-ear cavity, while bearing the disadvantages of single-hand surgical manoeuvres and a two-dimensional view.Reference Ohnsorge2 During the last half-century, endoscopic approaches for middle-ear pathologies have shifted from diagnostic-only to operative procedures, including tympanoplasties, cholesteatoma removal and stapes surgery.Reference Tarabichi3–Reference Kozin, Gulati, Lehman, Remenschneider, Kaplan and Landegger5
A plethora of studies has been conducted regarding the comparability of the microscopic versus the endoscopic technique, the learning curve, otological outcomes and complication rates. In addition to quality, ample evidence is needed, which cannot be drawn from individual studies and trials. Thus, we feel that a systematic review and meta-analysis of the aforementioned parameters of each approach is of great importance, allowing sturdy conclusions apropos the best technique for the patients’ benefit.
Materials and methods
We prospectively designed search methods, eligibility criteria and a data extraction process. No patient informed consent or institutional review board or ethics committee approval were required because of the nature of the study, which was based on published records. This meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (‘PRISMA’) statement.Reference Moher, Liberati, Tetzlaff and Altman6
Search strategy
Two review authors performed an electronic literature search to identify published studies comparing microscopic with endoscopic stapedectomy (EG and KTD). The electronic search involved three medical databases: PubMed, Cochrane Library and Scopus. We used the following medical subject heading (MeSH) terms and Boolean operators in the search: ‘otosclerosis’, AND ‘endoscopic stapedectomy’ OR ‘endoscopic stapedotomy’ OR ‘endoscopic stapes surgery’, AND ‘microscopic stapedectomy’ OR ‘microscopic stapedotomy’ OR ‘microscopic stapes surgery’, AND ‘success rate’ OR ‘complication’ OR ‘length of hospitalization’ OR ‘cost’. The search process was limited to English-language literature, and the search period extended from 1964 until July 2020 (Table 1). The literature was last accessed in January 2021. Additional records were traced in the reference lists of the gathered studies.
Table 1. Current meta-analysis search strategy according to the PICOT format
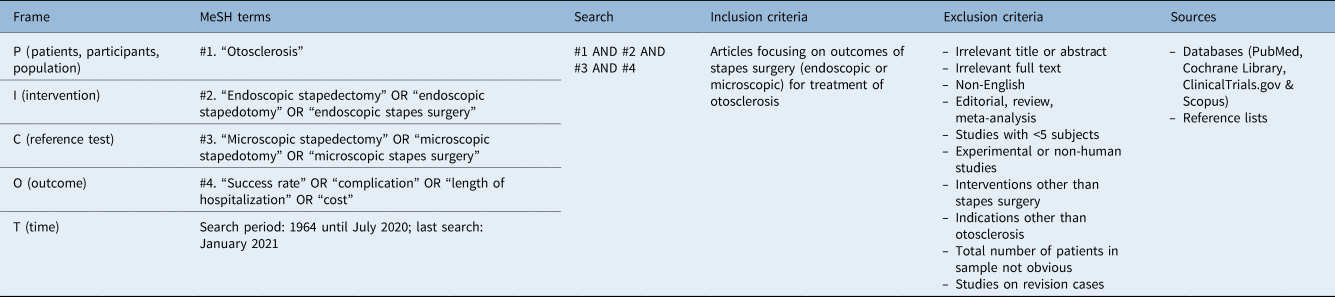
PICOT = patient, intervention, comparator, outcome and timing; MeSH = medical subject heading
Eligibility criteria
We focused primarily on randomised, controlled studies and secondarily on observational studies comparing endoscopic with microscopic stapes surgery in terms of success rate, complications, hospitalisation duration and cost-effectiveness. We discarded case series, case reports, editorials, reviews and systematic reviews, and studies without data suitable for quantitative analysis. We also excluded studies reporting on surgical interventions other than stapes surgery.
Data extraction
Each study was identified by the name of the first author and the year of publication. The following data were collected: (1) the size of the endoscopic stapes surgery group; (2) the size of the microscopic stapes surgery group; (3) the success rate measured as mean and standard deviation (SD) in each group; (4) the counts of individual complications in the endoscopic and microsurgery groups; (5) the length of hospitalisation in the endoscopic and microsurgery groups; and (6) the costs of the endoscopic and microsurgery groups.
Quality appraisal
Quality appraisal for individual studies, as well as assessment of the overall quality of evidence in the current analysis, was conducted by two independent review authors (KTD and EG). Individual quality appraisal for each included study was conducted using the ROBINS-IReference Sterne, Hernán, Reeves, Savović, Berkman and Viswanathan7 tool for non-randomised studies and the RoB 2Reference Sterne, Savović, Page, Elbers, Blencowe and Boutron8 tool for randomised, controlled trials (RCTs). The ROBINS-I and RoB 2 tools assess studies in seven and four domains, respectively. Both individual RCTs and non-RCTs were considered, bearing a ‘high’, ‘moderate’ or ‘low’ risk of bias, based on the evaluation. The overall quality of the gathered evidence was assessed according to the Grading of Recommendations Assessment, Development and Evaluation (‘GRADE’) Working Group recommendations,9 and categorised as ‘high’ (grade 4), ‘medium’ (grade 3), ‘low’ (grade 2) or ‘very low’ (grade 1) quality of evidence. In cases of disagreement, the two authors reached a consensus after consultation with the senior author (JH).
Data synthesis
The comparison of the two treatment options was conducted through a meta-analysis for every parameter under study. The outcomes of continuous measurements were pooled in terms of mean differences and 95 per cent confidence intervals (CI), whereas the outcomes of count measures were summarised in terms of odds ratios along with 95 per cent CIs through a paired meta-analysis. In addition, a proportion meta-analysis was performed to estimate the incidence of the complication in each arm independently. Inter-study heterogeneity was evaluated using the significance of the Cochran's Q-metric (pQ) and quantified by the Higgins I 2 statistics. Significance was set at p < 0.05, and we used continuity correction equal to 0.5 for metrics associated with zero events. The pooled estimate was assessed using the random effects model in the presence of inter-study heterogeneity (I 2 > 50 per cent) or with the fixed effects model. A sensitivity analysis would be considered only in the case of co-existence of significant statistical heterogeneity and more than three studies per stratum. Publication bias was eyeballed by funnel plots and assessed using the fail-safe N analysis, also known as ‘file-drawer analysis’. All statistical analyses were executed using the Jamovi project for the R-statistical environment.10,11
Results
Study selection and characteristics
In total, 159 articles were identified through database searching, of which 25 were excluded because of duplication. After the title and abstract evaluation, a further 117 articles were removed. Subsequently, the full text of the remaining 17 articles was reviewed and 4 more articles were excluded. Finally, 13 articles were considered eligible and were included in the quality assessment, while only 9 of them were included in the quantitative synthesis because of the paucity of statistics (Figure 1). Quantitative characteristics for these nine studies are presented in Table 2.Reference Kojima, Komori, Chikazawa, Yaguchi, Yamamoto and Chujo12–Reference Das, Mitra, Ghosh and Sengupta20

Fig. 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (‘PRISMA’) flowchart.
Table 2. Summary of eligible studies

Data for quantitative statistical analysis were drawn from 9 of the 13 eligible studies. ABG = air–bone gap; mth = month(s); wk = week(s); SNHL = sensorineural hearing loss; RCT = randomised, controlled trial
The selected articles included a total of 705 patients (711 ears) who underwent endoscopic or microscopic stapes surgery. All articles were written in English language, and were published between 2014 and 2021. One was a randomised, controlled study, while the remaining were observational non-randomised cohort studies. The evidence regarding stapes surgery complications and success is summarised in Tables 3 and 4.
Table 3. Summary of evidence regarding complications of stapes surgery
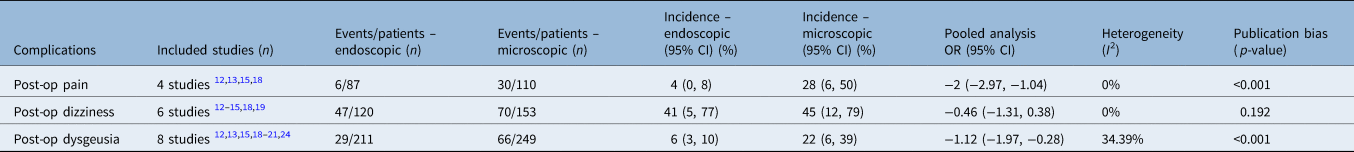
Results from the proportion and the paired meta-analyses with regard to post-operative complications of the two modalities. CI = confidence interval; OR = odds ratio; post-op = post-operative
Table 4. Summary of evidence regarding stapes surgery success

‘Success’ reflects post-operative air–bone gap of less than 20 dB. Results from the pooled meta-analysis with regard to post-operative air–bone gap considered successful. ABG = air–bone gap; CI = confidence interval
Quality assessment
Regarding the observational studies, all 12 (100 per cent) were considered to have a ‘moderate’ risk of bias. With regard to the randomised, controlled study, a ‘low’ risk of bias was ascertained in all domains. Evaluation findings for the observational studiesReference Kojima, Komori, Chikazawa, Yaguchi, Yamamoto and Chujo12–Reference Moneir, Abd El-Fattah, Mahmoud and Elshaer19,Reference Sproat, Yiannakis and Iyer21–Reference Kuo and Wu24 are presented in Table 5, and those for the randomised, controlled trialReference Das, Mitra, Ghosh and Sengupta20 are shown in Table 6. The overall quality of evidence was found to be ‘very low’ for three outcomes evaluated (pain, dysgeusia and dizziness) and ‘low’ for one outcome (success rate). Quality of evidence was downgraded largely because of the presence of risk of bias, indirectness and inconsistency issues (Table 7).
Table 5. ROBINS-I tool findings: individual observational study risk of bias evaluation

Domain 1 – bias because of confounding; domain 2 – bias because of participant selection; domain 3 – bias in classification of intervention; domain 4 – bias because of deviations from intended interventions; domain 5 – bias because of missing data; domain 6 – bias in measurement of outcomes; and domain 7 – bias in selection of the reported result. ‘−’ = moderate risk of bias; ‘+’ = low risk of bias
Table 6. RoB 2 tool findings: individual RCT study risk of bias evaluation

Domain 1 – bias arising from the randomisation process; domain 2 – bias because of deviation from intended intervention; domain 3 – bias because of missing outcome data; domain 4 – bias in measurement of the outcome; and domain 5 – bias in selection of the reported result. ‘+’ = low risk of bias. RCT = randomised, controlled trial
Table 7. Quality assessment of overall evidence according to GRADE recommendations9

Data represent grades unless indicated otherwise. Starting grade was 4 in outcomes where a randomised, controlled trial was included in the studies. Starting grade was 2 for outcomes where only observational studies where included. GRADE = Grading of Recommendations Assessment, Development and Evaluation working group
Success rate
Based on five studies,Reference Gulsen and Karatas13,Reference Surmelioglu, Ozdemir, Tarkan, Tuncer, Dagkiran and Cetik16–Reference Bhardwaj, Anant, Bharadwaj, Gupta and Gupta18,Reference Das, Mitra, Ghosh and Sengupta20 the pooled air–bone gap after endoscopic and microscopic stapes surgery was 9.08 dB (95 per cent CI = 7.06, 11.10) and 10.79 dB (95 per cent CI = 7.82, 13.75), respectively. In the absence of statistical heterogeneity (I 2 = 51.57 per cent, pQ = 0.08), there was no difference in terms of success rate between the two treatments (pooled mean difference = −0.20; 95 per cent CI = −0.53, 0.14) (Figure 2). In addition, the regression test for funnel plot asymmetry failed to detect publication bias (p = 9.79).
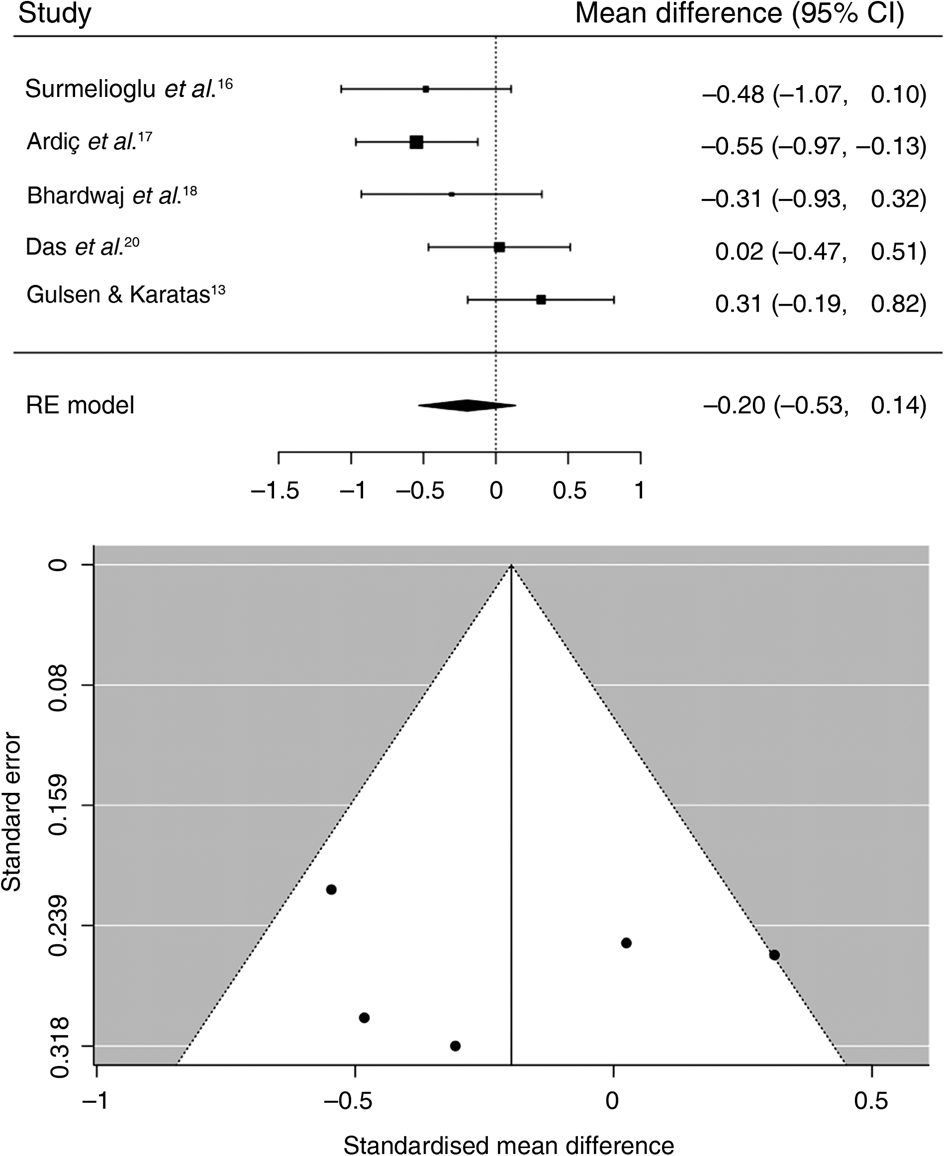
Fig. 2. Forest plot for success of stapes surgery. CI = confidence interval; RE = random effects
Complications
The available data permitted the pooling of evidence regarding the three post-operative complications associated with stapes surgery: pain, dizziness and dysgeusia (Figures 3–5). Dizziness was the most frequent post-operative complication, with estimated pooled incidence rates as high as 41 per cent (95 per cent CI = 5–77 per cent) for endoscopic procedures and 45 per cent (95 per cent CI = 12–79 per cent) for microscopic procedures. There was no statistically significant difference between the two modalities (odds ratio = −0.46 (95 per cent CI = −1.31, 0.38)). Conversely, the difference between the two modalities regarding dysgeusia was in favour of the endoscopic surgery (odds ratio = −1.12; 95 per cent CI = −1.97, −0.28). In fact, dysgeusia occurred with an estimated pooled incidence rate as high as 6 per cent (95 per cent CI = 3–10 per cent) after endoscopic surgery and 22 per cent (95 per cent CI = 6–39 per cent) after microscopic stapes surgery. Likewise, post-procedural pain was more frequent (odds ratio = −2.00; 95 per cent CI = −2.97, −1.04) after microscopic (28 per cent; 95 per cent CI = 6, 50) than endoscopic (4 per cent; 95 per cent CI = 0, 8) stapes surgery.

Fig. 3. Forest plot for post-operative pain. CI = confidence interval; RE = random effects

Fig. 4. Forest plot for post-operative dizziness. CI = confidence interval; RE = random effects

Fig. 5. Forest plot for post-operative dysgeusia. CI = confidence interval; RE = random effects
Operation time
Operation time ranged from 45 minutes (SD = 8.4 minutes) to 128 minutes (SD = 27 minutes) for endoscopic procedures, and from 36.5 minutes (SD = 8.2 minutes) to 132 minutes (SD = 38.7 minutes) for microscopic procedures. Based on four studies, there was no significant difference between the two techniques regarding operation time (mean difference = −1.92; 95 per cent CI = −5.88, 2.03; I 2 = 99.22 per cent).
Discussion
Otosclerosis is a multifactorial and complex disorder affecting hearing ability, caused by pathological bone resorption and deposition of the otic capsule.Reference Quesnel, Ishai and McKenna25 Stapes surgery is a widely accepted method and the ‘gold standard’ technique for treatment of this disease. While the microscopic approach has traditionally been the preferable modality, remarkable progress has been achieved utilising specially designed endoscopes, providing a powerful asset to otorhinolaryngologists aiming to improve any inadequacy associated with the microscopic approach.Reference Vincent, Sperling, Oates and Jindal26,Reference Marchioni, Rubini, Gazzini, Alicandri-Ciufelli, Molinari and Reale27
Offering excellent visualisation of the middle-ear cavity, the endoscopic technique permits a multi-angle view of every ‘corner’, combined with improved accessibility to fine structures. Furthermore, the endo-aural approach is feasible through endoscopes, even for narrow or curved external auditory canals, allowing minimally invasive operations. Thus, hearing improvement accomplished by endoscopic stapedectomy is considered comparable to its microscopic counterpart. This conclusion is supported by the results of the current study, and those of previous meta-analyses encountered in the literature, particularly research by Hall et al., Nikolaos et al. and Koukkoullis et al.Reference Hall, Mandavia and Selvadurai28–Reference Koukkoullis, Tóth, Gede, Szakács, Hegyi and Varga30 Exceptionally, Fang et al. observed a statistically significant difference in favour of the endoscopic technique, demonstrating its superiority.Reference Fang, Xu, Wang and Huang31
Moreover, the improved visualisation of the surgical field provided by the endoscope enables less bony auditory canal drilling, and, consequently, limited manipulation or injury of the chorda tympani, leading to better rates regarding post-operative dysgeusia.Reference Anschuetz, Siggemann, Dür, Dreifuss, Caversaccio and Huwendiek32 This is in compliance with the outcomes of recent meta-analyses, as their results are relevant to those of the current study.Reference Nikolaos, Aikaterini, Dimitrios, Sarantis, John and Eleana29–Reference Fang, Xu, Wang and Huang31 Furthermore, less or no scutum curetting, alongside minimal incisions, offers the advantage of minimal post-operative pain.Reference Koukkoullis, Tóth, Gede, Szakács, Hegyi and Varga30,Reference Fang, Xu, Wang and Huang31 This accords with the outcomes of the present study, where post-operative pain was less frequent for the endoscopic approach. On the contrary, Koukkoullis et al. reported no statistically significant difference between the two treatment modalities in terms of pain (odds ratio = 0.84; 95 per cent CI = 0.36, 1.96; I 2 = 64.2 per cent, p = 0.039), regardless of the slightest external auditory canal injury.Reference Koukkoullis, Tóth, Gede, Szakács, Hegyi and Varga30 Nonetheless, dizziness was the most frequent complication to be observed in the present study. However, no significant difference was reported between the two approaches (odds ratio = −0.46; 95 per cent CI = −1.31, 0.38; I 2 = 0 per cent, p = 0.192), even if dizziness was also lower with the endoscopic technique.
As far as the operation time is concerned, no statistical analysis could be executed because of the lack of measurable data. Hence, there was insufficient evidence in the present analysis that the endoscopic was inferior to the microscopic technique in this regard. Nonetheless, Das et al. reported a statistically significant difference in favour of the endoscopic technique; its operation time was 31 minutes shorter compared with the microscopic method (p < 0.05).Reference Das, Mitra, Ghosh and Sengupta20 Additionally, both Gulsen and Karatas, and Plodpai et al., recorded that endoscopic stapedectomy was faster than microscopic stapedectomy, yet no statistical significance was observed (p > 0.05 and p = 0.72, respectively).Reference Gulsen and Karatas13,Reference Plodpai, Atchariyasathian and Khaimook23 Moreover, Iannella and Magliulo mentioned that, in the absence of a statistical difference between the two approaches regarding operation time, during their last study period, the surgical execution time of endoscopic stapedectomy appeared to be significantly improved when comparing the first 10 with the last 10 patients.Reference Iannella and Magliulo15
Apart from its efficacy in ear surgery results, the endoscopic approach appears to be somewhat beneficial concerning middle-ear anatomy teaching and ear surgery skills acquisition. With the endoscopic technique, both the surgeon and their assistants have an unimpeded view of the surgical field and the procedure through the uniformly used monitor, resulting in better education for the observers of the operation.Reference Anschuetz, Siggemann, Dür, Dreifuss, Caversaccio and Huwendiek32,Reference Anschuetz, Stricker, Yacoub, Wimmer, Caversaccio and Huwendiek33 Nevertheless, like any other newly introduced technology, this innovative approach has a learning curve for every surgeon not acquainted with endoscopic otology.Reference Surmelioglu, Ozdemir, Tarkan, Tuncer, Dagkiran and Cetik16,Reference Bhardwaj, Anant, Bharadwaj, Gupta and Gupta18–Reference Das, Mitra, Ghosh and Sengupta20,Reference Plodpai, Atchariyasathian and Khaimook23,Reference Nogueira, Martins, Aguiar and Pinheiro34 In line with this view, Iannella and Magliulo reported that operative duration seemed to decrease with greater experience.Reference Iannella and Magliulo15 However, as the microscopic technique is of great importance and cannot be entirely substituted, ENT trainees should be enrolled in augmented learning curricula, combining microscopic and endoscopic ear surgery teaching, allowing optimal performance in otological surgery.Reference Anschuetz, Siggemann, Dür, Dreifuss, Caversaccio and Huwendiek32
As health professionals aim to achieve the highest possible satisfaction and comfort with their services, endoscopic stapes procedures undoubtedly belong in the everyday clinical practice of otological surgery. Given its proven predominance so far in terms of two-dimensional vision, cosmetic result, post-operative pain and safety, combined with a comparable success rate, endoscopic surgery seems to be the frontrunner, and may replace microscopes in most common otological cases in the near future.Reference Koukkoullis, Tóth, Gede, Szakács, Hegyi and Varga30,Reference Fang, Xu, Wang and Huang31 Furthermore, digitally developed surgical instruments (downsized endoscopes or less heat-emissive cold light sources), as well as the anticipated widespread use of robots in ear surgery, are expected to improve three-dimensional visualisation and overcome the aforementioned drawbacks of the endoscopic technique.Reference Aksoy, Dogan, Ozturan, Eren, Veyseller and Gedik35,Reference Dundar, Bulut, Güler, Yükkaldiran, Demirtaş and Iynen36 Undoubtedly, microscopes will still be available for advanced and more complex cases, such as reoperation or when the surgical view is obstructed by extensive bleeding.
Study limitations
The current study is characterised by some important limitations, affecting its power to arrive at extensively applicable conclusions. Most importantly, only one randomised, controlled trial was included in the current analysis. Moreover, clinical heterogeneity and inconsistency in numerous factors contributed to the downgrade of risk of bias scores, including: revision surgery, the number and experience of the operating surgeon(s), follow-up periods, methods and diagnostic tools of complication evaluation and assessment, sample size, and the retrospective nature of data collection. Furthermore, a lack of systematic complication assessment and evaluation methods limited the number of studies included in the final statistical analysis. Additionally, data regarding length of hospitalisation and cost were insufficient; thus, pertinent results in regard to these parameters could not be achieved. These factors should be addressed appropriately in future studies.
Conclusion
Endoscopic stapes surgery is a promising innovative alternative to the microscopic technique, resulting in commensurate outcomes regarding hearing improvement. In terms of post-operative complications, pain and dysgeusia appear to be less frequent using the endoscopic approach. Further studies need to be conducted, including wider sample sizes, in order to draw widely applicable conclusions concerning operation time, the learning curve and the acquisition of otology surgical skills.
Competing interests
None declared














