Introduction
The clinical use of the flattening filter-free (FFF) beam in linear accelerators is a subject of great interest in recent times.Reference Kry, Howell, Titt, Salehpour, Mohan and Vassiliev 1 – Reference Kry, Howell, Polf, Mohan and Vassiliev 3 Considering the physical characteristics of the FFF beam, it can be expected that the dose fall-off beyond the field sizes will be sharper than that of the flattened beam (FB). This could be attributed to the reduction in (residual) electron contamination and decline in the head scatter factor.
From the clinical perspective, FFF beam could lead to a reduction in the beyond field border dose for modern therapy delivery techniques. Sharper dose fall may yield a higher dose gradient, leading to a sparing of organs at risk (OAR), enhancing the dose to the tumor.
Another advantage of the FFF beam is its increased dose rate, which will in turn reduce the treatment time substantially. However, it is essential to validate the FFF beam for the dosimetric outcome of the beam, to reduce the healthy tissue dose, with better or equal tumor dose coverage. Several investigators have investigated different physical characteristics of the FFF beam, such as the beam profile, etc.
Therefore, the dosimetric characteristic of the FFF beam will have to be evaluated in actual clinical situations, specifically with the planning target volume (PTV) coverage and OAR sparing for different available linear accelerators.Reference Kragl, Baier and Lutz 4 A substantial amount of work has been published on Varian (Varian Medical System, Polo Alto, CA, USA) FFF; but the literature available regarding the Elekta (Elekta AB, Stockholm, Sweden) unflattened beam is very limited.Reference Mancosu, Castiglioni and Reggiori 5 – Reference Sarkar, Pradhan, Munshi, Roy, Ganesh and Mohanti 10
Stereotactic body irradiation (SBRT) is an emerging field and is used for different body sites, like lung, liver and spinal metastasis. SBRT has proved its efficacy in several cases, both for primary as well as metastatic sites. Stereotactic irradiation involves the delivery of a very high dose over a number of fractions. Body stereotactic radiotherapy demands a very good motion management technique.Reference Timmerman, Kavanagh, Cho, Papiez and Xing 11 – Reference Lee, Kim and Dinniwell 13 In particular, SBRT may be appropriate for selected patients with organ-confined, limited-volume primary tumours or oligo-metastatic disease.Reference Macdermed, Weichselbaum and Salama 14 Traditionally, SBRT was delivered using multiple three-dimensioanl conformal radiation therapy (3DCRT) beams or intensity-modulated radiation therapy (IMRT) beams.Reference Cai, Malhotra and Orton 15 , Reference de Pooter, Romero, Wunderink, Storchi and Heijmen 16 The disadvantage with 3DCRT is insufficient fluence modulation, yielding insufficient OAR sparing. However, IMRT gives a good fluence modulation, and hence better OAR sparing. The treatment time is considerably longer, which can lead to patient discomfort and an increase in the probability of inter fraction motion. Volumetric-modulated arc therapy (VMAT) may be a better option as it can deliver the radiation dose within a shorter time and achieve effective OAR sparing. The potential of VMAT used for SBRT to treat liver tumours has been evaluated by a few researchers; nevertheless, these evaluations have limitations.Reference Mancosu, Castiglioni and Reggiori 5 , Reference Reggiori, Mancosu and Castiglioni 6 For example, SBRT was not evaluated using FFF, during deep inspiration breath hold (DIBH) and free breathing conditions. The aim of this study, therefore, was to evaluate the characteristics of the flattened and unflattened beams of the Elekta agility linear accelerator, using VMAT-based liver SBRT technique, in free breathing and DIBH conditions.
Materials and Methods
For a set of eight liver-metastasis patients, computed tomography (CT) scans were taken using DIBH as well as free breathing conditions. Before CT simulation, all patients underwent two practice sessions of breath hold technique for procedure familiarisation. Patients were immobilised using a vacuum bag (vack-lock; Orfit Industries, Belgium).
The vacuum bag takes on the shape of the patient when deflated. An axial section of 1·5 mm axial CT slices was obtained in both DIBH and free breathing conditions. CT datasets were transferred to the Monaco Sim (CMS Elekta, Sunnyvale, CA, USA) workstation for contouring, using DICOM-enabled protocol.
An experience radiation oncologist contoured the gross target volume and clinical target volume, in the DIBH as well as free breathing study sets. In free breathing study set, the gross tumor volume was delineated using the minimum intensity projection that was obtained from the 20-slice Siemens positron emission tomography (PET)-CT (Biagraph MCT-20, Germany) console. DIBH and free breathing study sets were co-registered with each other, while they were obtained in the PET-CT. Therefore, they did not require any mutual information co-registration. OAR were contoured by the resident radiation oncologists. CT study sets, along with the contours, were transferred to the Monaco (CMS Elekta) treatment planning system, for radiotherapy planning. Elekta versa HD (Elekta AB) is a linear accelerator with 80 pairs of multi-leaf collimators (MLC) of 5 mm uniform width. It is capable of delivering both flattened and unflattened beams.
Planning was done using both FFF and flat 6 MV photon beams. All patients were treated with a dose of 50 Gy in 10 fractions (this is a standard regime followed in SBRT liver).Reference Milano, Katz and Muhs 17 All patients with one to three liver lesions were combined to form a lone PTV.Reference Rusthoven, Kavanagh and Cardenes 12 , Reference Lee, Kim and Dinniwell 13
A comparison of single patient plan is presented in Figure 1. Panels A, B, C and D represent FFF beam in free breathing CT dataset, FB in free breathing CT dataset, FB in DIBH CT dataset and FFF beam in DIBH CT dataset, respectively.

Figure 1 Treatment plans using moderate hypo-fractionated (50 Gy in 10 fractions) for liver SBRT. Panel A: FFF beam in free breathing CT dataset. Panel B: Flatten beam in free breathing CT dataset. Panel C: Flatten beam in DIBH CT dataset. Panel D: FFF beam in DIBH CT dataset. Abbreviations: SBRT, stereotactic body radiation therapy; FFF, flattened filter-free.
Patients were planned using a partial arc of 230° coplanar arc at table position of 0° (Gantry starts at 180° CW 200° + Gantry starts at 150° CW 30°). Two non-coplanar beams, 30° anterior and 30° posterior, were added at 270° table position. The gantry traverse for all arcs was twice the same locus. Table position–patient–gantry collision possibilities were evaluated before the actual delivery.
All plans were carried out using Elekta versa HD FFF 6 MV photon beam, for the purpose of treatment, in DIBH study set. Subsequently, the same plan was copied onto the free breathing study set and optimisation and dose calculation were carried out, without changing the optimisation parameters. Two more treatment plans were created in DIBH and free breathing study sets, using an Elekta versa HD linear accelerator with FB.
Results were evaluated for doses received by 98% PTV volume (D 98%), maximum dose, Paddick conformity index (CI), heterogeneity index (HI) and PTV volume receiving 105% (V105%) of the prescription dose. Paddick CI and HI were defined as follows:Reference Paddick 18
where TV = target volume, V RX = target volume covered by 100% isodose line, V RI = volume of 100% isodose line, and D 5% and D 95% were the doses received by 5 and 95% of the target volume.
OAR doses were evaluated for mean dose, for bowel bag, heart, bilateral kidney, bilateral lung, chest wall, diaphragm and liver. Spinal cord was evaluated for the maximum dose. Spillage dose to unspecified tissues, corresponding to different beam models in DIBH and free breathing study sets, were evaluated for 5% (I-5%), 10% (I-10%), 20% (I-20%), 30% (I-30%), 40% (I-40%), 50% (I-50%), 60% (I-60%), 70% (I-70%) and 80% (I-80%) isodose volumes.
Results
The mean PTV volume of the liver lesions was 23·7 ± 12·9 cm3, with no patient exhibiting more than three lesions. The graphical comparison of the dose–volume histogram for flattened and unflattened beams, on DIBH, is presented in Figure 2.

Figure 2 Dose–volume histogram comparison in DIBH and free breathing study sets, using flattened and unflattened beams. Abbreviation: DIBH, deep inspiration breath hold.
Averaged overall patient results for dose received by 98% volume (D 98%), maximum dose, Paddick CI, HI and PTV volume receiving 105% (V105%) of the prescription dose are presented, respectively, in the left and right panels of Figure 3.
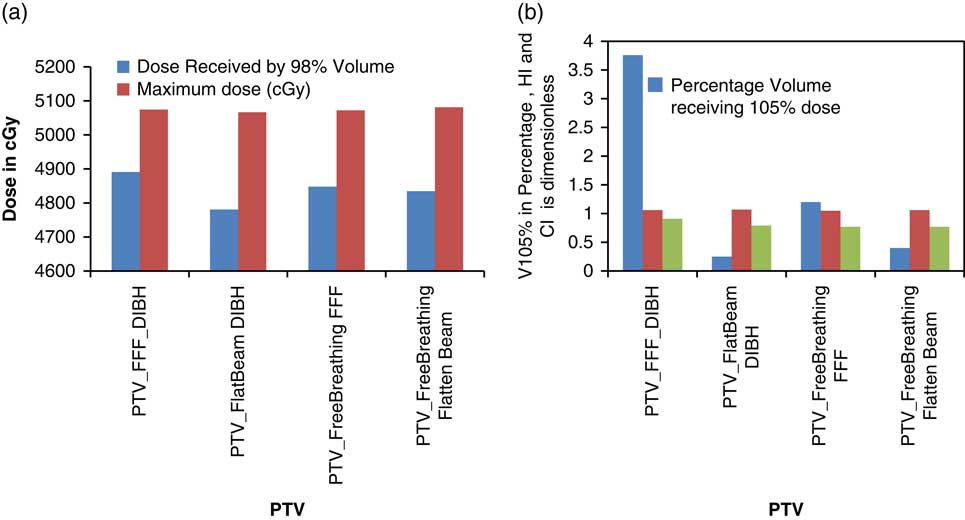
Figure 3 Variation of PTV coverage and hotspot related parameters, as a function of beam model in DIBH and free breathing condition. Abbreviations: DIBH, deep inspiration breath hold; PTV, planning target volume.
Mean D 98% for FFF in DIBH, FB DIBH, FFF in free breathing and FB in free breathing dataset were 48·9, 47·81, 48·5 and 48·3 Gy, respectively. Statistical co-relation (p) at 95% confidence interval (p), between the different beam models, was calculated using a Student’s t-test. DIBH study set p, for FFF-FB, was 0·34. Free breathing study set p, for FFF-FB, was 0·69. Statistical significance p, for FFF-FB, indicates no statistical variation between the DIBH and free breathing study sets. The average PTV maximum dose for FFF and FB for DIBH study sets, were 50·7 and 50·7 Gy, respectively. Maximum doses for free breathing study set, for the same group, were 50·7 and 50·8 Gy, respectively. PTV V 105% for the same set were 3·76, 0·25, 1·2 and 0·4%, respectively. Mean HI for all study sets and beam models varies between 1·05 and 1·07. Paddik CI, using unflattened and FBs, in DIBH at 98% prescription dose were 0·91 and 0·79, respectively. The average CI of both beams, for free breathing CT set, was 0·77. The difference between the FFF and FBs for DIBH study set (statistical significance p) was <0·001.
Average dose for OARs including the bowel bag, heart, bilateral kidneys, bilateral lung, chest wall, diaphragm, liver and maximum dose for spinal cord were presented in Figures 4a, 4b and 4c, respectively.
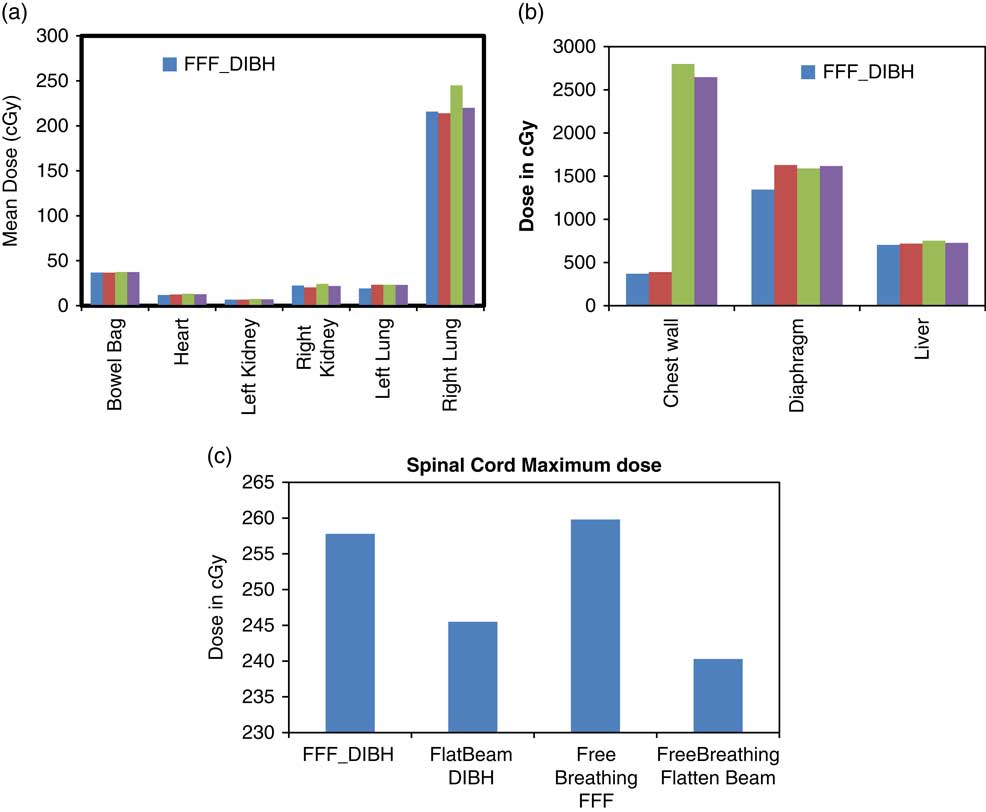
Figure 4 Mean dose to bowel bag, heart, bilateral kidney, bilateral lung (panel A), chest wall, diaphragm and liver (panel B) and maximum dose to the spinal cord (panel C), in DIBH and free breathing datasets using unflattened and flattened beam models. Abbreviation: DIBH, deep inspiration breath hold.
The dose administered to organs presented in panel A of Figure 4 is very low, as the organs are away from the target volume. Mean dose to the right lung varies between 2·2 and 2·5 Gy with regard to different beam models and study sets. Bowel, bilateral kidney and left lung doses were between 0·07 and 0·37 Gy. Average doses to chest wall, for unflattened beam and FB, were 3·7 and 3·9 Gy, respectively; the same for free breathing study set were 28 and 26·5 Gy, respectively. Difference of dose on chest wall, between DIBH and free breathing study sets, was statistically significant (p = 0·03). Mean diaphragm doses for all four tested plans were comparable and varied between 13·4 and 16·3 Gy. Mean liver dose also did not yield any variation, with respect to beam models and study sets.
The spillage doses of different beams and models (I-5% and I-10% to I-80%), are presented in Figure 5.

Figure 5 Isodose volume of 5% and 10%–80% were plotted as a function of beam model in DIBH and free breathing conditions.
Figure 5 shows a negligible variation of the isodose volumes, with respect to flattened and unflattened beams, in DIBH and free breathing conditions. For example, I-5% yields a variation within the range of 2288·8–2427·2 cm3. This was noted to be the highest variation among all the isodose volumes. The variation between the isodose volumes attributed to the flattened and unflattened beams, for DIBH and free breathing conditions, diminishes with the increasing isodose values. The variation in I-80% was between 47·6 and 53·8 cm3, which is only 6·2 cm3.
Monitor unit
Average monitor units of FFF beam in DIBH, FB in DIBH, FFF beam in free breathing CT dataset and FB in free breathing CT dataset were 1318·6 ± 265·1, 1940·3 ± 287·6, 1343·3 ± 238·1 and 2192·5 ± 252·6 MU, respectively. The mean numbers of the breath holds were found to be 3·3 ± 1·9 and 9·7 ± 3·2 for unflattened beam and FB, respectively.
Discussion
Several studies of the past have investigated the planning aspect of unflattened beam, for liver and lung SBRT, esophagus, craniospinal irradiation and cranial stereotactic radiotherapy.Reference Reggiori, Mancosu and Castiglioni 6 – Reference Sarkar, Pradhan, Munshi, Roy, Ganesh and Mohanti 10 , Reference Dzierma, Bell, Palm, Nuesken, Licht and Rübe 19 – Reference Sarkar, Pradhan and Munshi 21 It is established that unflattened beam is dosimetrically comparable with the FB. Investigators have obtained a mixed result on the efficacy of the unflattened beam over the FB. For liver SBRT, many studies have been designed, comparing flattened and unflattened beams. However, no study group has studied the influence of breath hold technique on this. This study is the first of its kind to evaluate flattened and unflattened beams, with respect to free breathing and breath holding techniques.
Reggiori et al. noted the effect of tumour volume on flattened and unflattened beams, depending on the CI. They favored unflattened beam for intermediate volume tumours (100 cm3 ≤ PTV volume ≤ 300 cm3) and FB for the smaller and larger tumours. The mean target volume of the patient in this study did not exceed 50 cm3. However, we have observed an advantage of the unflattened beam over the FB in the target conformity.Reference Reggiori, Mancosu and Castiglioni 6
Earlier studies have noted a considerable reduction in the delivery time for unflattened beam because of the enhanced dose rate. For Elekta linear accelerator, the dose rates are 600 and 2000–2200 MU/minute, for flattened and unflattened beams, respectively. Breath holding times do not exceed 30 seconds, with the average holding time between 20 and 25 seconds. Therefore, breath holding technique essentially requires an unflattened beam to reduce the delivery time.
The advantage of Elekta versa HD linear accelerator is the speed of the MLC, which is as fast as 6 cm/second, which helps sustain a very high dose rate of 2000–2200 MU/minute. High dose rate delivery requires a higher MLC speed for a compatible delivery. A low MLC speed cannot sustain a high dose rate VMAT delivery.Reference Manikandan, Sarkar, Holla, Vivek and Sujatha 22
In this study, we observed a high CI with respect to the unflattened beam for breath hold technique. OAR doses to chest wall show a high dose difference between the breath hold and the free breathing techniques. Change in the CI of the unflattened beam is characteristic of the unflattened character of the beam. However, the loss of dose to the chest wall can be attributed to the fact that the chest wall in DIBH is fixed in a longer distance, for a longer time from the target. However, decrease in chest wall doses can be explained only with the unflattened characteristic of the beam.
As per the basic theory of Gaussian distribution, an unflattened beam is closer to a Gaussian distribution while a FB is a blur Gaussian. With the same characteristics, an unflattened beam should observe a better dose buildup to tumour, with a sharper fall at the periphery. However, no such phenomenon has been observed in any previous investigations so far.
Several authors have reported phase I/II clinical trials of liver metastasis, using stereotactic body irradiation.Reference Rusthoven, Kavanagh and Cardenes 12 , Reference Lee, Kim and Dinniwell 13 , Reference Fong, Fortner, Sun, Brennan and Blumgart 23 – Reference Aloia, Vauthey and Loyer 25 For the large surgical series, including those primarily in patients with metastatic colorectal cancer, 5-year survival after liver resection ranges between 37 and 71%.Reference Fong, Fortner, Sun, Brennan and Blumgart 23 – Reference Aloia, Vauthey and Loyer 25 Patients who were not suitable for surgery and those with poor risk-prognostic factor were chosen for the radiotherapy clinical trials, yielding a median survival of 20·5 month and a two-year local control of 100%.Reference Rusthoven, Kavanagh and Cardenes 12
Conclusion
VMAT-based stereotactic body irradiation for liver metastesis shows considerable reduction in the delivery time for FFF beam, when compared to the FB. The reduction in delivery time is essential to keep the treatment time suitable for patients using the breath holding technique. Unflattened beam shows no dosimetric advantage for unspecified tissues and OAR. However, a better conformal dose distribution was obtained for the unflattened beam. In conclusion, an unflattened beam is a good choice for liver SBRT, while using the breath hold technique.
Acknowledgements
The patient treatment plans were performed at Aditya Birla Memorial Hospital, Pune. The authors are very much thankful for treatment planning system analysis by Dr Rajeev Srivastav, Dr Birendra kumar Rout and Dr Govindaraj.








