Anorexia nervosa is a psychiatric disorder characterised by prolonged restriction of food intake and severe weight loss (American Psychiatric Association, 2013). This illness is one of the most difficult to treat because starvation impairs a number of areas of functioning, including physical health and psychological wellbeing. Over time, these health consequences create a ‘snowball effect’ that depletes individuals' resources and chances to recover (Treasure et al., Reference Treasure, Stein and Maguire2015). Data from naturalistic, long-term follow-up studies suggest that only 40–62% of individuals recover from anorexia nervosa over a period of 20 years (Zipfel et al., Reference Zipfel, Löwe, Reas, Deter and Herzog2000; Eddy et al., Reference Eddy, Tabri, Thomas, Murray, Keshaviah, Hastings, Edkins, Krishna, Herzog, Keel and Franko2017; Fichter et al., Reference Fichter, Quadflieg, Crosby and Koch2017).
One way of optimising treatment efficacy is to augment current interventions in the early phases of treatment. This is based on evidence that rapid symptomatic improvement during the first few weeks of treatment is associated with favourable clinical outcomes at the end of treatment and/or follow-up in adolescents and adult patients (Linardon et al., Reference Linardon, Brennan and de la Piedad Garcia2016; Wales et al., Reference Wales, Brewin, Cashmore, Haycraft, Baggott, Cooper and Arcelus2016; Nazar et al., Reference Nazar, Gregor, Albano, Marchica, LoCoco, Cardi and Treasure2017). To date, there are no published reports on the efficacy of different treatment augmentation strategies in the early phase of adult anorexia nervosa treatment. However, two studies examining the efficacy of short treatment modules to improve patient engagement with standard treatment found that brief interventions focused on psychoeducation and/or motivational enhancement increased the likelihood of treatment engagement compared to a control condition (Brewin et al., Reference Brewin, Wales, Cashmore, Plateau, Dean, Cousins and Arcelus2016; Denison-Day et al., Reference Denison-Day, Muir, Newell and Appleton2019).
We developed an online, 6-week guided self-help intervention, RecoveryMANTRA, to augment treatment as usual (TAU) for adult outpatients with anorexia nervosa by targeting motivation to change (Cardi et al., Reference Cardi, Ambwani, Crosby, Macdonald, Todd, Park, Moss, Schmidt and Treasure2015). The intervention is built upon the cognitive interpersonal model and Maudsley Model of Anorexia Nervosa Treatment for Adults (MANTRA; Schmidt and Treasure, Reference Schmidt and Treasure2006; Treasure and Schmidt, Reference Treasure and Schmidt2013) and conceptualised within a recovery framework. This framework highlights the centrality of peer support, optimism about the future, confidence in one's ability to change, development of identity and meaning, and empowerment (Leamy et al., Reference Leamy, Bird, Le Boutillier, Williams and Slade2011) and uses connections with others and skills-sharing as key aspects of recovery (Smith-Merry et al., Reference Smith-Merry, Freeman and Sturdy2011). Indeed, a recent systematic review and meta-synthesis on the process of recovery from anorexia nervosa highlighted the importance of addressing a disrupted sense of self and rebuilding identity, a commitment to change and establishing meaningful relationships with others as a path to self-acceptance (Stockford et al., Reference Stockford, Stenfert Kroese, Beesley and Leung2018). The emphasis of RecoveryMANTRA is on empowering individuals by increasing their motivation and confidence to change. This is consistent with the assumptions of self-determination theory that underpins the intervention and also with the evidence that a patient's motivation to change predicts clinical outcomes and treatment adherence (Clausen et al., Reference Clausen, Lübeck and Jones2013; Vall and Wade, Reference Vall and Wade2015; Thaler et al., Reference Thaler, Israel, Antunes, Sarin, Zuroff and Steiger2016; Denison-Day et al., Reference Denison-Day, Appleton, Newell and Muir2018). Furthermore, the goal to strengthen an individual's confidence to change is consistent with the importance of developing a recovery identity that might improve treatment engagement and outcomes (Dingle et al., Reference Dingle, Stark, Cruwys and Best2015).
The aim of the current study was to examine the acceptability and efficacy of RecoveryMANTRA following assessment for anorexia nervosa at an outpatient service. It was hypothesised that RecoveryMANTRA, used to augment TAU, would increase body mass index (BMI) at 6 weeks (primary outcome) and reduce eating disorder symptoms, psychological distress (depression, anxiety, stress) and work and social impairment over time (6 weeks and 6- and 12-month follow-up). It was also hypothesised that the intervention would increase scores on process measures, such as cognitive and behavioural flexibility, motivation to change and therapeutic alliance. Frequencies of service use (including outpatient treatment, intensive treatment, appointments with general practitioner, family therapy and group therapy) were compared between groups at 6 and 12 months.
Method
The protocol of this study was published in 2015 (Cardi et al., Reference Cardi, Ambwani, Crosby, Macdonald, Todd, Park, Moss, Schmidt and Treasure2015).
Setting and recruitment
Participants were recruited from 22 adult eating disorder outpatient services across the UK (see Acknowledgements for details) between April 2015 and December 2016. Informed written consent was sought from participants after a complete description of the study. The study received ethical approval from a National Research Ethics Service Committee (London Brent, approval number 14/LO/1347) and from the local research and development offices at the participating centres.
Participants
Patients consecutively assessed at one of the participating centres were recruited if (1) they were aged 16 or over, (2) had a diagnosis of anorexia nervosa according to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5; American Psychiatric Association, 2013) or atypical anorexia nervosa [i.e. people who fulfilled all the diagnostic criteria, except the weight criterion; those who fulfilled all criteria but still had menses; those without fat phobia; and those with partial anorexia nervosa, defined as having features of the illness, but missing at least two of the four diagnostic criteria (Thomas et al., Reference Thomas, Vartanian and Brownell2009)], (3) had a BMI of 18.5 kg/m2 or below and (4) had access to the Internet. Participants were considered ineligible if they had (1) insufficient knowledge of English and/or (2) severe mental or physical illness needing treatment (i.e. psychosis or diabetes mellitus). Participant eligibility was assessed using a checklist by the clinicians and clinical study officers recruiting at the centres and clinical diagnoses were confirmed by the clinicians at the participating sites.
The consort diagram in Fig. 1 shows the number of participants assessed and randomised to the study groups and also the number of participants who completed the assessment measures at baseline, 6 weeks, 6 and 12 months. Of those assessed for study eligibility (n = 202), 187 participants were found to be eligible and were randomised to the RecoveryMANTRA + TAU group (n = 99) or to the TAU only group (n = 88). The 6-week questionnaires were completed by 79.8% and 80.68% of participants in each group, respectively. The 6-month questionnaires were completed by 78.79% in the experimental group and 71.59% of participants in the control group. The 12-month BMI data were obtained from 70.05% of the entire sample (see Fig. 1).
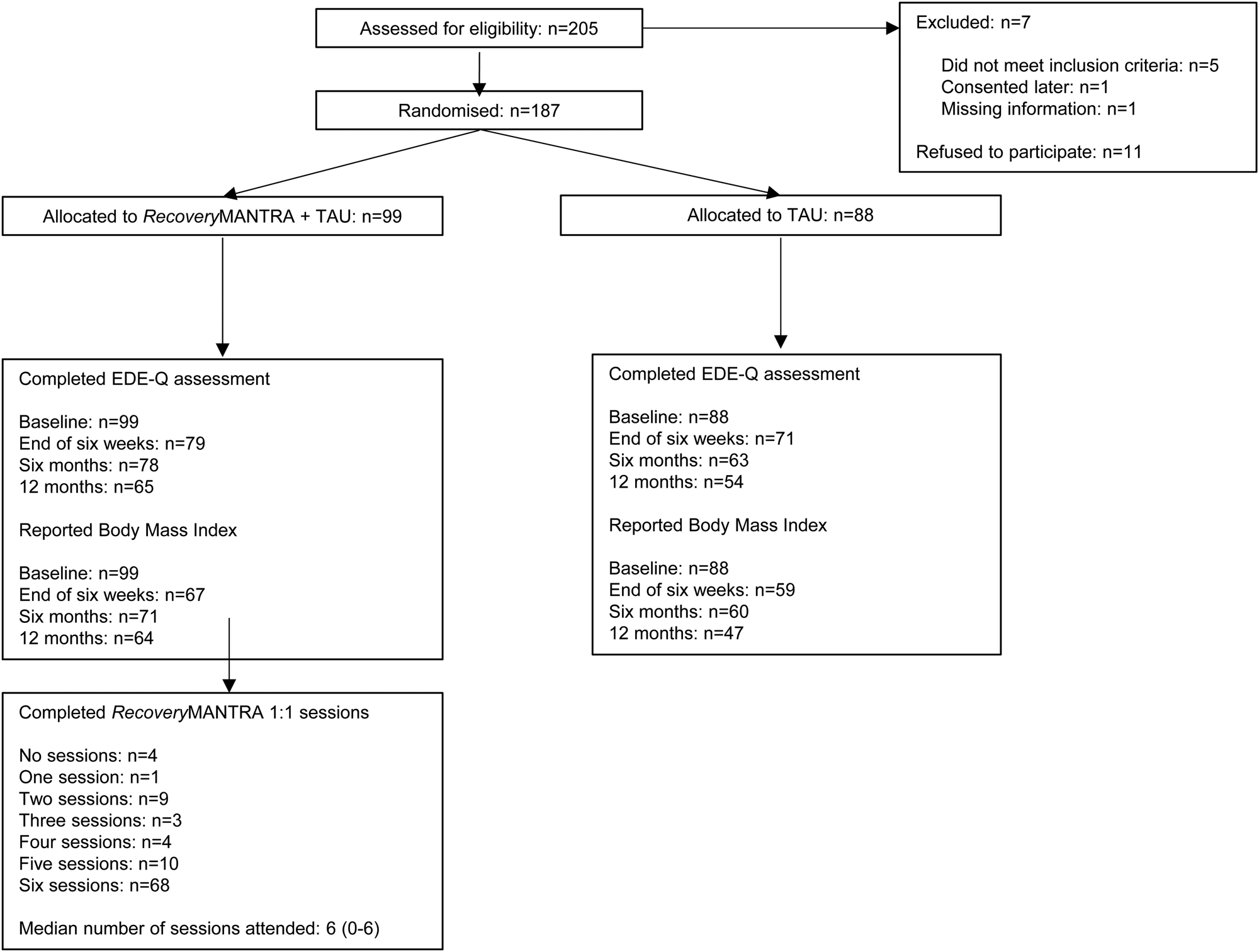
Fig. 1. Flow diagram of participation through the different phases of the trial, including eligibility, randomisation, allocation to study groups, completion of assessments and completion of intervention sessions.
Randomisation
Participants were randomly allocated to one of the two groups: (1) RecoveryMANTRA plus TAU or (2) TAU only. TAU in the participating centres was based on the guidelines of the National Institute for Health and Care Excellence (NICE, 2017), which recommended outpatient care (including psychoeducation, symptom monitoring, psychotherapy) as the first stage of treatment for adults with anorexia nervosa without high medical risk. Randomisation was conducted in Excel by an independent researcher using randomisation stratified by participating centre and illness severity (with severe illness defined as BMI <16 kg/m2). Once the database had returned a participant's group allocation, no changes were made.
Intervention
The group allocated to receiving Recovery MANTRA in addition to TAU had the opportunity to access a workbook, a library of short video clips (‘vodcasts’) and six, 1-h, text-chat sessions with a recovery mentor (either a postgraduate student in psychology, a carer or an individual recovered from an ED for at least 1 year). The intervention materials were developed in collaboration with recovered individuals to challenge the ED identity and develop a more positive social, recovery-oriented identity, a feature associated with improved treatment outcomes for other forms of psychopathology, such as depression (Cruwys et al., Reference Cruwys, Alexander Haslam, Dingle, Jetten, Hornsey, Desdemona Chong and Oei2014), substance abuse and dependence (Dingle et al., Reference Dingle, Stark, Cruwys and Best2015; Frings and Albery, Reference Frings and Albery2015), as well as anorexia nervosa (Stockford et al., Reference Stockford, Stenfert Kroese, Beesley and Leung2018). Motivational interviewing was adopted as the communication strategy throughout the intervention materials to increase confidence and motivation to change. After 6 months, patients in the control group (i.e. TAU only) were granted access to the intervention materials. For further details on RecoveryMANTRA and its theoretical background, please refer to the study protocol paper (Cardi et al., Reference Cardi, Ambwani, Crosby, Macdonald, Todd, Park, Moss, Schmidt and Treasure2015).
Treatment fidelity
Recovery mentors (postgraduate psychology students, n = 13; carers, n = 2; or people recovered from an ED who had been weight-recovered and ED symptom-free for at least 24 months, n = 9) completed two mandatory 3-day trainings in motivational interviewing and implementation of RecoveryMANTRA. Two-day ‘booster’ training sessions were also offered twice a year. Recovery mentors also received a weekly email or telephone supervision based on session transcripts by one of two clinical supervisors with extensive experience in the treatment of EDs.
Assessments
Eligible participants accessed assessments and RecoveryMANTRA materials online through IESO Digital Health (http://www.iesohealth.com). Participants completed self-report questionnaires on the online platform at baseline, 6 weeks, 6 and 12 months. Assessments were prompted by a research assistant sending an email reminder through the online platform the day before the assessments were due. After completion of the baseline assessment, participants were randomised to one of the two study groups and their clinicians at the participating site were kept blind to this allocation. Although all study measures were collected online and completed as self-reports, the clinical teams (blind to treatment allocation) were contacted to report on BMI at 6 weeks, 6 and 12 months to recover missing data. The research team did not measure participants' weight and height at assessment or follow-up because patients were recruited from all over the UK and face-to-face research assessments were not feasible.
Self-reported clinical measures
Eating disorder symptoms were assessed using the Eating Disorder Examination Questionnaire (EDE-Q; Fairburn and Beglin, Reference Fairburn and Beglin1994); mood was measured using the Depression, Anxiety and Stress Scales (DASS-21; Lovibond and Lovibond, Reference Lovibond and Lovibond1995) and quality of life was assessed using the Work and Social Adjustment Scale (WSAS; Mundt et al., Reference Mundt, Marks, Shear and Greist2002). These measures were assessed at baseline, 6 weeks, 6 and 12 months.
Self-reported process measures
Motivation for treatment was assessed at baseline and 6 weeks using The Autonomous and Controlled Motivations for Treatment Questionnaire (Zuroff et al., Reference Zuroff, Koestner, Moskowitz, McBride, Marshall and Bagby2007; adapted from Williams et al., Reference Williams, Rodin, Ryan, Grolnick and Deci1998). This measure assesses people's intrinsic, internally generated motivation to change (i.e. autonomous motivation), as well as motivation to change due to external demands and pressures (i.e. controlled motivation). Motivation to change was assessed at baseline, 6 weeks, 6 and 12 months, using two visual analogue scales (scales ranging from 0 to 10 and measuring confidence in one's own ability to change and importance to change). Alliance with the therapist at the outpatient service was measured at baseline and 6 weeks, using five, seven-point visual analogue scales developed by the study team (i.e. the scales measured levels of: therapist's understanding, confidence in therapist's ability to point towards the right direction of change, mutual agreement on therapeutic goals, trust and ability of therapist to offer new ways of looking at the problem; an average total score was used for the analyses). Cognitive and behavioural flexibility was measured at baseline and 6 weeks, using two, seven-point visual analogue scales developed by the study team (i.e. the scales measured the extent to which participants pay attention to small details at the detriment of seeing the bigger picture and the extent to which they need to adhere to rules and rituals in their behaviour; average total score was used for the analyses).
Participants service use
This was assessed asking participants to report on the usage of clinical services (including outpatient treatment, inpatient or daycare services, group therapy, family therapy and appointments with the general practitioner) over the previous 6 and 12 months.
Assessment of RecoveryMANTRA intervention usage
The number of 1-h, chat-based sessions attended was recorded for each participant in the RecoveryMANTRA arm. Based on average completion rates reported in systematic reviews of individual psychotherapy (20–40%; Dejong et al., Reference Dejong, Broadbent and Schmidt2012) and technology-based interventions (57.6%; Schlegl et al., Reference Schlegl, Bürger, Schmidt, Herbst and Voderholzer2015) for eating disorders, we set an a priori definition of ‘completion’ as attendance at a minimum of four of the six offered sessions. Participants also completed daily ratings of usage of workbook and video clips over the 6 weeks (42 days).
Statistical analyses
All analyses were conducted in SPSS version 24.0 (SPSS, Inc., USA, IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp.). Univariate analyses of variance were used to compare the intervention (RecoveryMANTRA + TAU) and control (TAU alone) groups on the sociodemographic, clinical and process continuous variables separately at 6 weeks, 6 and 12 months. Logistic regression was used for dichotomous measures. Covariates for all models included baseline observations. All analyses were based on an intention-to-treat (ITT) approach, except for the frequency of using clinical services. Missing data for outcomes at 6 weeks, 6 and 12 months were imputed using multiple imputation based upon the Markov chain Monte Carlo method (Schafer, Reference Schafer1997) and maximum likelihood imputation based upon the Expectation-Maximization (EM) algorithm. Results were compared across the two methods. Effect sizes for the outcomes were established using Cohen's d and interpreted as small (0.2), medium (0.5) and large (0.8) (Cohen, Reference Cohen1988).
The primary outcome was BMI at 6 weeks. Secondary outcomes were BMI at 6 and 12 months, eating disorder symptoms (EDE-Q total score), depression, anxiety and stress scores (DASS-21) and work and social adjustment (WSAS) at 6 weeks, 6 and 12 months. Process measures were autonomous and controlled motivation for treatment, confidence in own ability to change and importance to change, and cognitive and behavioural flexibility. Frequencies of clinical service use were compared between groups using Pearson's χ2 tests.
Results
Participants' characteristics
One-hundred and eighty-seven participants (including n = 181 females) completed the baseline assessment (see Table 1 for demographic and descriptive information). This is within the target sample size (n = 180) resulting from the power calculation reported in our protocol paper (Cardi et al., Reference Cardi, Ambwani, Crosby, Macdonald, Todd, Park, Moss, Schmidt and Treasure2015). There were no significant differences in demographic or clinical variables between the control and intervention groups at baseline, except for a trend-level difference in BMI (p = 0.06; higher BMI in the TAU only group). Participants had suffered from an eating disorder for 7.76 years on average (s.d. = 8.91), and 22% (n = 42) had had previous hospital admissions. At the time of recruitment, 123 participants (70.3%) had started outpatient treatment following assessment. As noted in Table 1, assessment of functioning indicated clinically significant elevations on eating disorder symptoms (EDE-Q) and moderate to severe levels of depression, anxiety and stress (DASS-21). Mean scores on the WSAS indicated significant functional impairments.
Table 1. Baseline demographic and clinical data for the entire sample, RecoveryMANTRA + treatment as usual (TAU) group and TAU-only group

Completion of guidance sessions and the use of self-help materials
Eighty-two individuals completed four or more of the six guidance sessions (82.83%; Fig. 1). The self-help materials (workbook and/or video clips) were accessed by 76.77% of the participants (76/99) in total. Frequency of usage for the self-help materials was variable, with some accessing the resources once (n = 6), between six and 10 times (n = 21) and up to 21–26 times (n = 9) over the course of the 6-week intervention period.
Primary and secondary outcomes
Differences between groups are described in Table 2. No significant group differences in BMI were found at 6 weeks (primary outcome). No significant differences between groups were found on BMI at 6 and 12 months and no significant differences were found on eating disorder symptoms, depression, stress and work and social adjustment at any time points. There was a trend-level difference in anxiety scores between groups at 6 weeks (p = 0.06), with a reduction in anxiety in the intervention group and an increase in the control group.
Table 2. Baseline, 6-week, 6- and 12-month clinical outcome data and process measures for the trial's participants

Primary outcome highlighted in bold.
Data imputed using multiple imputation based upon Markov chain Monte Carlo method (n = 187 participants). Primary outcome = body mass index at 6 weeks.
Analyses were repeated after data were imputed with maximum likelihood imputation based upon the EM algorithm. The same patterns of findings were found, overall (online Supplementary Table S1).
Process measures
Differences between groups were explored with regard to process measures (i.e. cognitive and behavioural flexibility, autonomous and controlled motivation for treatment, importance and confidence in own ability to change and alliance with therapist at the outpatient service) (Table 2). Significant differences between groups were found on confidence in own ability to change and alliance with therapist at 6 weeks (p = 0.02 and p = 0.005, respectively), both of which were higher in the intervention group. Group differences in confidence in own ability to change reduced over time and were no longer significant at 6 or 12 months. Group differences in the other process measures were not statistically significant. The type of mentor allocated to participants (either a postgraduate student in psychology or a carer, or an individual recovered from an ED) did not affect the pattern of findings.
Similar findings were obtained when data were imputed using maximum likelihood imputation based upon the EM algorithm (online Supplementary Table S1), with the exception of importance to change, which also increased significantly more in the intervention group, compared to the control group, at 6 weeks (p = 0.03).
Service use
At 6 months, a greater proportion of participants in the RecoveryMANTRA group (88.31%) than the control group (71.42%) were still attending outpatient treatment, χ2(1) = 6.34; p = 0.01. This difference was not significant at 12 months, χ2(1) = 0.85; p = 0.35. There were no other significant differences between groups in terms of frequency of service use over the previous 6 or 12 months, including use of intensive treatment (inpatient or day-care), visits to general practitioner, group therapy or family therapy.
Discussion
The aim of this study was to test the acceptability and efficacy of adding an online self-help intervention, RecoveryMANTRA, to augment outpatient treatment for anorexia nervosa. There was a reasonably high level of adherence (with 83% completing four or more sessions) to the online guidance which adopted a motivational interviewing framework. Additionally, over three-quarters of our participants accessed the self-help videos and workbook at some point during the 6-week intervention. However, the usage of the self-help videos and workbook materials was variable across respondents, with some demonstrating high levels of use and others accessing the resources infrequently. The intervention did not produce between-group differences in BMI, but there was a greater trend-level reduction of anxiety symptoms in the RecoveryMANTRA group at 6 weeks, compared to an increase in anxiety in the control group. This effect was no longer significant at 6- and 12-month follow-up. Group differences on eating disorder symptoms or other indicators of well-being such as depression, stress and work and social adjustment were negligible. These findings align with those described in a recent meta-analysis of specialised treatments in anorexia nervosa, which found a lack of superiority effects over standard treatment on improving weight and psychological outcomes at follow-up (Murray et al., Reference Murray, Quintana, Loeb, Griffiths and Le Grange2019). Similarly to other treatment trials (e.g. Zipfel et al., Reference Zipfel, Wild, Groß, Friederich, Teufel, Schellberg, Giel, de Zwaan, Dinkel, Herpertz, Burgmer, Löwe, Tagay, von Wietersheim, Zeeck, Schade-Brittinger, Schauenburg and Herzog2014; Schmidt et al., Reference Schmidt, Ryan, Bartholdy, Renwick, Keyes, O'Hara, McClelland, Lose, Kenyon, Dejong, Broadbent, Loomes, Serpell, Richards, Johnson-Sabine, Boughton, Whitehead, Bonin, Beecham, Landau and Treasure2016; Byrne et al., Reference Byrne, Wade, Hay, Touyz, Fairburn, Treasure, Schmidt, McIntosh, Allen, Fursland and Crosby2017), participants in this study had clinical features associated with a worse prognosis, including long duration of illness and low weight. Furthermore, they were receiving outpatient treatment at their clinical sites and RecoveryMANTRA was compared against this. Both severity of symptoms and concurrent outpatient treatment might limit the impact of RecoveryMANTRA and explain the lack of augmentation effects on BMI and core eating disorder symptoms.
The target outcomes of the motivational interviewing strategies employed by recovery mentors (i.e. confidence in own ability to change and alliance with TAU therapists) increased at 6 weeks in the intervention group. This indicates good fidelity and adherence to the model. These results are consistent with recent findings from a multisite outpatient trial of cognitive-behavioural therapy for anorexia nervosa, which reported that the motivational enhancement module was the most commonly used, thereby attesting to the value of motivational strategies to tackle the core feature of ambivalence in anorexia nervosa (Resmark et al., Reference Resmark, Kennedy, Mayer, Giel, Junne, Teufel, de Zwaan and Zipfel2018).
Strengths and limitations
The current study has several strengths, some of which have been considered critical for improving the quality and clinical usefulness of randomised controlled trials in eating disorders (Lock et al., Reference Lock, Kraemer, Jo and Couturier2018; Wade et al., Reference Wade, Johnson and Byrne2018). A protocol paper was published when the trial started (Cardi et al., Reference Cardi, Ambwani, Crosby, Macdonald, Todd, Park, Moss, Schmidt and Treasure2015) with a full description of rationale, methods and plans for analyses, ensuring that no changes to the original plan were made based on the trial findings. Missing data were addressed by ITT analyses and by using two different ways of imputing missing data; randomisation biases were minimised using block randomisation and adjustment for baseline variables in the analyses. External validity of the study was ensured by the involvement of many different services across the UK (thereby reflecting real-life clinical practice with no control over TAU) and the inclusion of typical, as well as atypical presentations of anorexia nervosa. A range of outcomes were used to capture changes in transdiagnostic psychological variables above and beyond eating disorder-related outcomes (i.e. weight and eating disorder symptoms; Murray et al., Reference Murray, Loeb and Le Grange2018). The sample size was above minimal requirements for capturing clinically significant treatment effects (n = 50; Kraemer and Thienemann, Reference Kraemer and Thiemann1987) and attrition rates were within the lower end of those typically observed in the field (20–40%; DeJong et al., Reference Dejong, Broadbent and Schmidt2012).
A possible limitation of this study is that participants' access to the Internet was not assessed continuously throughout the project. Difficulties accessing the Internet might explain the modest use of online self-help materials. However, patients' ambivalence towards change might also account for the sub-optimal use of self-help materials which did not involve direct supervision from the mentor. A further limitation is that patients' weight and height (main study outcome) were not directly measured by the study team. This is because participants were recruited from all over the UK and face-to-face research assessments were not feasible.
Clinical implications
It is somewhat surprising that improvements in therapist alliance and confidence in own ability to change were not matched by improvements in weight and eating disorder psychopathology as there is evidence that these common factors in psychotherapy are major drivers of clinical symptom change in the treatment of anorexia nervosa (Sly et al., Reference Sly, Morgan, Mountford and Lacey2013; Brauhardt et al., Reference Brauhardt, de Zwaan and Hilbert2014). The lack of effect may be, in part, because of the suboptimal match between the primary and secondary outcomes (i.e. BMI and eating disorder symptoms) with the contents of the self-help materials and guidance (i.e., intra- and inter-personal maintaining factors, recovery identity, motivational enhancement). Upon reflection, the psychological processes targeted (and successfully changed) in the intervention might need more intense and sustained efforts (i.e. longer duration, more guidance) to translate into changes in weight and core eating disorder symptoms in this participant group who, for the most part, have shown themselves to be resistant to treatment. Alternatively, recent findings suggest that exposure to recovery narratives may not directly increase motivation to change, or could evoke positive as well as negative (e.g. social comparative) responses, thus highlighting the need for further assessment of underlying mechanisms for recovery narratives and alternative strategies for presentation of these stories (Dawson et al., Reference Dawson, Mullan, Touyz and Rhodes2018). It is also possible that the format of our intervention failed to optimise reflection and adoption of a recovery identity through increasing social support. For example, clinical observations from a trial in progress testing online guided self-help for patients with anorexia nervosa and their carers to facilitate the transition from intensive hospital treatment into the community (Cardi et al., Reference Cardi, Ambwani, Robinson, Albano, Macdonald, Aya, Rowlands, Todd, Schmidt, Landau, Arcelus, Beecham and Treasure2017) indicate that strengthening social connection by improving patient-to-patient support and support from carers is highly valued by participants.
Conclusions
RecoveryMANTRA increased confidence in the person's own ability to change and therapeutic alliance with TAU clinicians in the short-term. The intervention was also associated with small-sized improvements in anxiety compared to the control group. More extended periods of guidance and/or a greater focus on interpersonal elements might improve clinical outcomes over time. Strategies such as inviting carers to provide support and encourage the use of self-help materials (Hibbs et al., Reference Hibbs, Magill, Goddard, Rhind, Raenker, Macdonald, Todd, Arcelus, Morgan, Beecham, Schmidt, Landau and Treasure2015; Cardi et al., Reference Cardi, Ambwani, Robinson, Albano, Macdonald, Aya, Rowlands, Todd, Schmidt, Landau, Arcelus, Beecham and Treasure2017) and greater utilisation of peer support to strengthen the recovery identity (Leamy et al., Reference Leamy, Bird, Le Boutillier, Williams and Slade2011) might better augment outpatient interventions for anorexia nervosa.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291719002824.
Acknowledgements
This paper presents independent research funded by the National Institute for Health Research (NIHR) under its Research for Patient Benefit (RfPB) Programme (Grant Reference Number PB-PG-0712-28041). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. This work was also supported by the Psychiatry Research Trust, the NIHR Maudsley Biomedical Research Centre for Mental Health (VC, JT, US) and the South London and Maudsley NHS Foundation Trust (US, JT). The views expressed herein are not necessarily those of the NHS, NIHR or the Department of Health. We are grateful to the recovered individuals who contributed to the video clips used in the RecoveryMANTRA intervention and to Scarlet Park and Elise Pacquette, who contributed illustrations for the workbook. We acknowledge the support of the National Institute for Health Research Clinical Research Network (NIHR CRN) and are very grateful to our participating clinical services and local collaborators for their help with participants' recruitment (participating centres: Avon and Wiltshire Mental Health NHS Trust, Barnet Enfield and Haringey Mental Health NHS Trust, Berkshire Healthcare NHS Foundation Trust, Cambridgeshire and Peterborough NHS Foundation Trust, Central and North West London NHS Foundation Trust, Coventry and Warwickshire Partnership NHS Trust, Cumbria Partnership NHS Foundation Trust, Derbyshire Healthcare Foundation Trust, Dorset Healthcare University NHS Foundation Trust, Kent and Medway NHS, Leicestershire Partnership NHS Trust, Lincolnshire Partnership NHS Foundation Trust, Northamptonshire Healthcare NHS Foundation Trust, North Essex Partnership NHS Foundation Trust, Nottinghamshire Healthcare NHS Foundation Trust, South London and Maudsley NHS Foundation Trust, South Staffordshire and Shropshire healthcare NHS Foundation Trust, South Essex Partnership University NHS Foundation Trust, South West London and St George’ s Mental Health NHS Trust, Surrey and Borders Partnership NHS Foundation Trust, Sussex Partnership NHS Foundation Trust, Worcestershire Health and Care NHS Trust. Local collaborators: Alysum Jones, Heather Tinkler, Lynsel Wilson, Katie Egan, Eric Johnson-Sabine, Karishma Jivraj, Ilyas Mirza, Elma Ramly, Emma Donaldson, Jessica Cox, Alice Wright, Amber Dickinson, Andy Foster, Jane Shapleske, Frances Connan, Matthew Pugh, Hayley Dunn, Naomi Bateman, Kay Wright, Anthony Winston, Aujla Manjit, James Tucker, Emily Benson, Liz Bolt, Miriam Naheed, Yumna Masood, Sarah Thornthwaite, Jose Schutter, P. Kendal, Audrey Williamson, Lisa Thompson, Rubina Reza, Joanna Miatt, Ciaran Newell, Jean Throughton, Hazel Eaton, Ramesh Muthuswamy, Alisha O’ Connor, Hannah Herlihy, Jon Arcelus, Debbie Whight, Rebecca Cashmore, Thomas Hanly, P. Marshall, Rachael Lawrence, Anna Chafer, Helen Birchall, Sally Clarke, Michelle Chalke, Amy McConnell, Mhorag Brown, Lara Horrax, Ian Lea, Steph King, Neisha Rhule, Kim Moore, Andy Taylor, Tim Lewington, Jane Dalgleish, Sarah Thurlow, Jennifer Walker, Marissa Hodson, Vicky Fryer, Maxine Barnard, Sophia Ali, Irene Yi, Jack Holland, Ashley Chapman, Jane Gregg, Dorrie Mystris, Renate Pantke, Philippa Case, Charmaine Kohn, Kay Lobo, Angela Hoadley). We are grateful to all our study participants for their patience and perseverance.






