Introduction
The lateral wall of the nose is a complex structure, both in terms of anatomy and physiology. The nasolacrimal duct is a continuation of the lacrimal sac downwards to the inferior meatus. It has an intraosseous portion (12 mm approximately) and an intrameatal portion (5 mm approximately).Reference Whitnall1, Reference Burkat, Lucarelli, Cohen and Brazzo2 The bony nasolacrimal canal is inclined posteriorly and laterally towards the first molar tooth. The course of the nasolacrimal duct is hence directed downwards, posteriorly and laterally, and this is a very important landmark on the lateral wall topography.Reference Whitnall1, Reference Burkat, Lucarelli, Cohen and Brazzo2
Nasolacrimal duct injury has been reported as a consequence of numerous surgical procedures, including uncinectomy, frontal sinusotomy, maxillary osteotomy, external or endoscopic medial maxillectomy, rhinoplasty, inferior turbinectomy, and maxillofacial trauma repair.Reference Shoshani, Samet, Ardekian and Taicher3–Reference Lauritzen and Lilja6 Very few studies have specifically investigated nasolacrimal duct injury following functional endoscopic sinus surgery (FESS).Reference Serdahl, Berries and Chole7–Reference Sadeghi and Joshi12 This paper evaluates the features of the bony nasolacrimal duct pre- and post-uncinectomy, and documents the radiological incidence of nasolacrimal duct injury in a moderately large cohort of patients who underwent FESS.
Materials and methods
Approval was obtained from the institutional research board of the Queen Elizabeth Hospital, Woodville, Adelaide, South Australia, prior to conducting this study. A retrospective, consecutive case series analysis was conducted. It included all patients for whom there were pre- and post-operative radiological images, who had undergone FESS between August 2013 and January 2014.
Fine-cut, axial computed tomography (CT) sinus scans, with three-dimensional reconstructions, were obtained for all patients. Patient demographics, indications for surgery and FESS type were noted. Information collected from the CT scans included: radiological details of nasolacrimal duct anatomy; evidence of nasolacrimal duct dehiscence or damage; presence or absence of residual uncinate process post-surgery; and extent of maxillary sinus disease. Clinical profiles of patients with surgical nasolacrimal duct dehiscence were recorded, and correlations between nasolacrimal duct dehiscence and diagnosis, extent of surgery and surgeon's level of experience were determined.
Results
Sixty-three patients who underwent 118 uncinectomies were included in this study. The male to female ratio was 1:1.6 (24:39). The mean age of patients at the time of surgery was 45 years (range, 18–80 years). Indications for surgery included: chronic rhinosinusitis with nasal polyposis, in 41 per cent of patients (26 out of 63); chronic rhinosinusitis without nasal polyposis, in 54 per cent (34 out of 63); and maxillary sinus inverted papilloma, in 5 per cent (3 out of 63).
Uncinectomies were performed in conjunction with maxillary antrostomy and anterior ethmoidectomy in 41 per cent of patients (48 out of 118), and together with frontal sinusotomy, maxillary antrostomy and total sphenoethmoidectomy in 59 per cent (70 out of 118). All cases except two were primary procedures. Forty-one per cent of patients (26 out of 63) were operated on by trainees; the remaining patients were operated on by consultants.
Pre-operatively, there was complete opacification of the maxillary sinus in 41.2 per cent of patients and partial opacification in 38 per cent. The mean Lund–Mackay score for the maxillary sinus was 1.16 out of 2, with mean scores of 1.25 on the right and 1.07 on the left side. Post-operatively, the overall mean Lund–Mackay score was 0.48, with mean scores of 0.49 and 0.47 on the right and left sides respectively.
There was evidence of residual uncinate process following surgery in 8.4 per cent of patients (10 out of 118), suggesting an incomplete uncinectomy (Figure 1a). Four bony nasolacrimal ducts showed thin but intact walls pre- and post-operatively (Figures 1b and 1c). The incidence of pre-operative nasolacrimal duct dehiscence was 6.8 per cent (8 out of 118 cases) (Figures 1d and 2a). There was reactive osteitis of the nasolacrimal duct post-operatively in 5 out of 118 patients (4.2 per cent), although no dehiscence was noted (Figures 2b–d).

Fig. 1 Axial computed tomography scans, showing: (a) bilateral intact bony nasolacrimal ducts but with residual uncinate process on the left side, (b) and (c) thin-walled but bilaterally intact nasolacrimal ducts, and (d) pre-operative large bilateral bony nasolacrimal duct dehiscence.
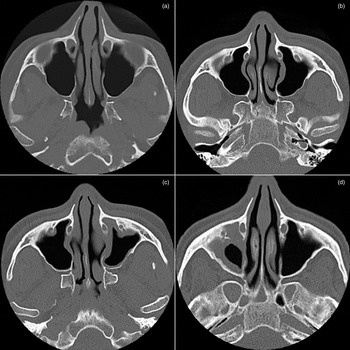
Fig. 2 Axial computed tomography post-operative scans showing: (a) no increase in dehiscence (dehiscence is stable) (shows the same patient as in Figure 1d), (b) bilaterally intact but thin-walled nasolacrimal ducts, (c) intact nasolacrimal duct, but there is reactive osteitis of the posteromedial and posterolateral walls (shows the same patient as in part b), and (d) an example of bilateral reactive osteitis affecting the posterior wall of the nasolacrimal duct (left side more than the right) following functional endoscopic sinus surgery.
In 3.3 per cent of patients (4 out of 118), there was new evidence of dehiscence post-operatively (Figures 3a–d). Of these four patients with nasolacrimal duct injury as a consequence of surgery, two had a diagnosis of chronic rhinosinusitis with nasal polyposis, one had a diagnosis of chronic rhinosinusitis without nasal polyposis and one had an inverted papilloma involving the maxillary sinus. None of these four patients had dehiscence pre-operatively. Two patients reported epiphora in the post-operative period; one of these opted for and underwent endoscopic dacryocystorhinostomy. All nasolacrimal duct injuries occurred in patients operated on by a trainee. No injuries were caused by a consultant. The radiologist did not comment on the status of the nasolacrimal duct in relation to any of the pre- or post-operative scans.

Fig. 3 Axial computed tomography scans showing: (a) thinned but intact bony nasolacrimal duct, (b) post-operative radiograph of the same patient as in part a – note the gross posterior wall dehiscence bilaterally, (c) pre-operative radiograph showing bilaterally intact nasolacrimal duct with thin rims posteromedially, and (d) post-operative radiograph of the same patient as in part c, demonstrating left postero-medial wall dehiscence with minimal prolapsed soft tissue.
Discussion
Although it is a well-recognised complication, nasolacrimal duct injury following FESS is poorly documented in the literature. In the current study, the radiological incidence of iatrogenic nasolacrimal duct injury for patients undergoing uncinectomy was 3.3 per cent. The nasolacrimal duct passes anterior to hiatus semilunaris in the wall of the middle meatus, and here the distance between nasolacrimal duct and maxillary ostium ranges from 3 to 6 mm. This close anatomical relationship predisposes the nasolacrimal duct to iatrogenic injury during uncinectomy and middle meatal antrostomy.
Serdahl et al.Reference Serdahl, Berries and Chole7 were the first to report cases of nasolacrimal duct injury following FESS; all eight patients affected required dacryocystorhinostomy for post-operative epiphora. In their study, the mean time interval between injury and dacryocystorhinostomy was nine months. Those authors proposed that when enlarging the maxillary ostium anteriorly with backbiting forceps, the thicker bone surrounding the nasolacrimal duct could be inadvertently removed if caution was not taken, with subsequent damage to the duct itself. While vigorous anterior enlargement of middle meatus ostium is to be discouraged, the authors believe that use of the backbiting forceps is safe as long as anatomical boundaries are respected.
Kennedy et al.Reference Kennedy, Zinreich, Shaalan, Kuhn, Naclerio and Loch8 reviewed 117 middle meatal antrostomies and found 2 cases of nasolacrimal duct injury and epiphora. They suggested that one case was secondary to silver nitrate cautery used in the region for adhesions and the second was thought to be a direct consequence of intra-operative trauma to the nasolacrimal duct. Bolger et al.Reference Bolger, Parsons, Mair and Kuhn9 reported a much higher rate of intra-operative injury, with evidence of occult nasolacrimal duct trauma in 15 per cent of the 46 endoscopic procedures included in their study. None of their patients subsequently developed epiphora; this led Bolger et al. to conclude that occult nasolacrimal duct trauma is more common in FESS than first appreciated. However, in the current study, two of the four patients with nasolacrimal duct injury reported epiphora.
Unlu et al.Reference Unlu, Goktan, Aslan and Tarhan10 evaluated 31 patients following FESS with active transport dacryocystography. This evaluation was performed at a mean period of 59.7 days after the surgery (range, 12–247 days). The non-operated sides of unilateral cases (n = 15) were taken as controls. Bony dehiscence of the nasolacrimal duct was noted in 53.2 per cent of operated cases and in 20 per cent of non-operated cases. Epiphora was not reported by any of the patients; 14.9 per cent of the operated patients demonstrated no passage of dye into the inferior meatus, possibly reflecting a nasolacrimal duct obstruction. The authors of that study concluded that nasolacrimal duct injury need not always result in epiphora, and performing middle meatal antrostomy in the posteroinferior direction may minimise the chance of nasolacrimal duct injury.
Our study, the largest to date, provides further information on the incidence of nasolacrimal duct injury following surgery. Unlike the above-mentioned studies, the availability of both pre- and post-operative imaging allowed documentation of pre-existent and surgically related dehiscence, which may explain the lower rate of nasolacrimal duct injury reported. The low incidence of iatrogenic injury made it difficult to draw conclusions regarding the influence of the type and extent of disease on the likelihood of injury. Nevertheless, it was interesting to note that all injuries occurred when the procedure was performed by a trainee, suggesting that surgical experience and anatomical knowledge may be an important factor.
To our knowledge, this study is the first to also report on the prevalence of reactive osteitis following uncinectomy. The findings suggest that patients with thick bone surrounding the nasolacrimal duct may be somewhat protected from injury, and that the prevalence of injury may be higher in patients with thin bone.
• Functional endoscopic sinus surgery can result in nasolacrimal duct injury, with reported incidences of injury ranging from 15 to 53 per cent
• A close anatomical relationship between the maxillary ostium and nasolacrimal duct predisposes the latter to injury
• This study elucidates the concepts of pre-operative dehiscence, reactive osteitis and thinning of the bony nasolacrimal duct
• Active participation by otolaryngologists in pre-operative lacrimal system assessment and active supervision of trainees during middle meatal antrostomy is essential
• Post-operative follow up of patients with dehiscence is required to determine the need for further lacrimal surgery
Another interesting finding of this study not documented in the literature is the failure of radiologists to record pre-existing nasolacrimal duct dehiscence when reporting on sinus CT scans. This does suggest that otolaryngologists themselves should become familiar with the radiological course of the nasolacrimal duct and with variants in the bony anatomy, in the hope of identifying patients at risk of iatrogenic injury. Other factors that may reduce the incidence of injury during FESS include clear visualisation of the surgical field, appreciation of regional anatomy, controlled enlargement of the maxillary ostium, a posteroinferior direction of the backbiter punch and avoidance of bone engagement anterior to the uncinate process.
Conclusion
Nasolacrimal duct injury following FESS is uncommon, but it does occur. Hence, all patients should be consented appropriately pre-operatively. Surgeons should familiarise themselves with the radiological and surgical anatomy of the nasolacrimal duct to reduce the possibility of injury during surgery.
Acknowledgements
The authors wish to acknowledge Ms Lyn Martin and Ms Sabera Banu for their help with the literature search and provision of the relevant articles.





