Introduction
An itchy ear is one of the most frequently encountered complaints in otolaryngological practice.Reference Djalilian and Memar 1 Several otolaryngological diseases such as bacterial or fungal external otitis, hypocerumenosis, and allergic rhinitis can cause itching of the external ear canal. Itching of the external ear canal may also be a sign of a dermatological disease, or an underlying systemic disease such as diabetes mellitus, hepatic or renal diseases, lymphoma, leukaemia, or other malignancies. However, the cause of the itchy ear cannot be clarified in a significant portion of the patients.Reference Djalilian and Memar 1 , Reference Acar, Simsek, Oguztuzun, Zaim and Karasen 2 Although it is a common symptom, the aetiology and best choice of treatment for an itchy ear remain unclear.
Isolated itching of the external ear canal can be defined as the sensation of pruritus in the external ear canal, with the absence of any localised or systemic disease.Reference Tuzuner, Akdagli, Sen, Demirci, Tarimci and Caylan 3 Various topically applied medications, including ear drops, creams, ointments and magistral solutions, which contain alcohol, boric acid, steroids, antibiotics or immunosuppressive agents as ingredients, are used in an attempt to achieve symptomatic control.Reference Djalilian and Memar 1 , Reference Karakuş, Arda, Ikincioğullari, Gedikli, Coşkun and Balaban 4 – Reference Caffier, Harth, Mayelzadeh, Haupt and Sedlmaier 6 Steroid ear drops are generally effective in the treatment of itchy ears.Reference Djalilian and Memar 1 However, the long-term use of topical steroids is contraindicated as they have negative effects on keratinocytes, microvasculature and epidermal structure. Other available treatment options have their own limitations and alternative treatment approaches are needed in the management of patients with itchy ears.
Castellani's paint is a well-known and frequently used antiseptic agent in dermatology clinics.Reference Shah 7 It is also used in otolaryngological practice, especially in the treatment of external otitis and otomycosis.Reference Gultekin, Yener and Ozdemir 8 This study aimed to investigate the effects of Castellani's paint on the sensation of pruritus and on skin flora in patients with an itchy external ear canal.
Materials and methods
A prospective, randomised, controlled clinical study was designed and conducted at the otolaryngology and medical microbiology departments of Baskent University, Ankara, Turkey. This study was approved by the Baskent University Institutional Review Board and Ethics Committee (project no: KA10/79) and supported by the Baskent University Research Fund. Written informed consent was obtained from all participating patients.
The study included 61 patients who complained of recurrent, bilateral itchy ear canals. ENT examination findings of the patients were normal. Patients who had a history of long-term topical or systemic steroid and/or antibiotic use, and those who had used topical or systemic steroids and/or antibiotics in the previous week, were excluded from the study. Patients who had impacted cerumen, or who showed signs of otological disease such as otomycosis, external otitis or chronic otitis media on otoscopic examination, were also excluded, as were those who had a history of ear surgery, systemic disease such as diabetes mellitus, renal or hepatic disorders, or dermatological disease such as psoriasis or atopic dermatitis.
Subjective pruritus was evaluated by asking the patients to score the degree of itching between 0 (none) and 10 (extreme). In order to determine the effect of pruritus on quality of life, patients were asked to complete two surveys: the Dermatology Life Quality Index and the Short Form (36) Health Survey (‘SF-36’)). During the otoscopic examination, a physician scored the degree of erythema and desquamation in the external ear canal using a seven-point scoring scale (0 = none, 1 = very mild, 2 = mild, 3 = moderate, 4 = moderately strong, 5 = severe and 6 = extreme). Afterwards, bilateral external ear canal skin swabs were taken for bacterial and fungal cultures.
Patients were randomly divided into three groups. In group one, 1 cc Castellani's paint was instilled into the external ear canal of the patients, bilaterally, on days 0, 3, 6, 9 and 12. Castellani's paint contains phenol, basic fuchsine, ethyl alcohol 95 per cent, boric acid, acetone, resorcinol and distilled water. In group two, 3–4 drops of 0.1 per cent dexamethasone ear drops (Onadron; İbrahim Etem Ulagay İlaç Sanayi Türk, Istanbul, Turkey) were instilled into each patient's ear, 3 times a day for 7 days, and once daily for the next 5 days. In group three, the lateral one-third of the external ear canal was gently cleared with curettes, and, if present, non-impacted cerumen was manually removed. The patients in group three received no medication.
The patients were re-assessed one month after the initial visit by the same physician, who did not ask as to the patients' treatment type. The doctor assigned the scores before learning which treatment each patient had received. The degree of erythema and desquamation in the external ear canal, subjective pruritus, and quality of life were re-assessed, and scores were compared with those before treatment.
Microbiological analyses
All microbiological analyses were performed by a microbiologist who was blind to the nature of the samples. All samples were subcultured on 5 per cent sheep agar, MacConkey agar and two Sabouraud dextrose agar plates. The 5 per cent sheep agar, MacConkey agar and one of the Sabouraud dextrose agar plates were incubated at 37 °C for 24–48 hours; the other Sabouraud dextrose agar plate was incubated at 30°C for 1 week. The degree of reproduction density was determined using a score ranging from 1 to 4.
Gram-positive cocci were identified as Staphylococcus aureus and coagulase-negative staphylococcus by catalase and coagulase tests. Corynebacteria were classified to genus level and streptococci were classified according to haemolysis characteristics. Gram-negative bacilli were identified to species level by conventional methods using a fully automated microbiology system (Phoenix; Becton Dickinson Diagnostic Systems, Sparks, Maryland, USA). For yeasts, a germ tube test was conducted. Corn meal agar was used as the medium and the yeasts were identified with a semi-automated system (API 20C Aux; bioMerieux-Vitek, Hazelwood, Missouri, USA). For mould yeasts, Sabouraud dextrose and potato dextrose agars were used, and microscopic characteristics were determined using lactophenol cotton blue stain.
Statistical analyses
Statistical analysis was performed using SPSS software (version 22.0; SSPS, Chicago, Illinois, USA). The values representing scores were expressed as mean scores ± standard deviations. The Kruskal–Wallis test was used to compare the data among groups. Wilcoxon signed rank and Friedman tests were used to evaluate the data obtained before and after treatments. The chi-square test was used to evaluate categorical data. A p-value of less than 0.05 was accepted as statistically significant.
Results
The patients consisted of 18 men and 43 women (mean age, 51.87 ± 1.91 years; range, 20–81 years). There were 21, 20 and 20 patients in groups one (Castellani's paint), two (dexamethasone ear drops) and three (non-impacted cerumen removal), respectively. The patients' age (p = 0.232) and gender (p = 0.065) did not differ significantly among the groups.
Mean subjective pruritus scores, desquamation scores and erythema scores of the patients in all groups before and after treatment are given in Table I.
Table I Pruritus, desquamation and erythema scores pre- and post-treatment

Data represent mean scores ± standard deviations, unless indicated otherwise. Regarding treatment, Castellani's paint (group one) or steroid ear drops (group two) were instilled, or non-impacted cerumen was removed (group three).
Erythema (p = 0.225) and desquamation (p = 0.371) scores before treatment did not show a statistically significant difference among the groups. Subjective pruritus scores of the patients in group three were found to be lower than those in group two before treatment (p = 0.007). However, there was no statistically significant difference (p > 0.05) in terms of the subjective pruritus scores before treatment between group one and group two, and group one and group three.
There was no difference between groups one, two and three in terms of the desquamation scores (p = 0.063) or subjective pruritus scores (p = 0.121) after treatment. Erythema scores for the patients in group one were lower than those for group two (p = 0.015) and group three (p = 0.001), after treatment. However, erythema scores for the patients in group two and group three after treatment did not show a statistically significant difference (p = 0.478).
In all groups, subjective pruritus scores after treatment were significantly decreased when compared to those before treatment (Table I). Erythema scores for the patients in group one after treatment were significantly decreased when compared to those before treatment (p < 0.001); however, there was no such statistically significant difference in groups two (p = 0.102) and three (p = 1.0). Desquamation scores after treatment were significantly decreased in groups one (p < 0.001) and two (p = 0.02) when compared to those before treatment; however, there was no such statistically significant difference in group three (p = 0.317).
Culture swabs were taken from the external ear canals of 58 patients before treatment, and from those of 56 patients after treatment (Table II). Analysis revealed that the reproduction density of bacteria including normal flora was decreased in group one after treatment.
Table II External auditory canal colonisation findings pre- and post-treatment*
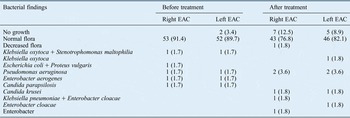
Data represent numbers (and percentages) of cases.
* For all treatment groups combined. EAC = external auditory canal
All patients reported that their itchy ear did not affect their lives, and many of the questions in the Dermatology Life Quality Index were not related to pruritus. In addition, scores for items related to overall health status (in the Short Form Health Survey) did not change after one month.
Discussion
Isolated itching of the external ear, with no underlying skin changes and normal physical examination findings of the external ear canal, can be defined as ‘itchy ear syndrome’.Reference King 9 It is more frequently seen in middle-aged and older women, as was the case in our study.Reference Acar, Simsek, Oguztuzun, Zaim and Karasen 2
The aetiology of itchy ear syndrome is not clear. Carcinoma of the external ear, seborrheic dermatitis, contact dermatitis, psoriasis and dermatomycosis are linked with an itchy external ear canal. Allergic contact dermatitis is also thought to cause itchy ears.Reference Djalilian and Memar 1 , Reference Acar, Simsek, Oguztuzun, Zaim and Karasen 2 Chemicals such as surfactants and preservatives found in hair cosmetics are believed to cause sensitisation of the external ear canal skin. The interaction of keratinocytes in the skin with small molecules called haptens, and cytokine secretion, results in irritation and itching of the skin. The thin skin covering the external ear canal is normally protected by secreted cerumen. In cases of hypocerumenosis or inappropriate cerumen removal, the surface becomes more vulnerable to haptens. Repetitive exposure of the skin to haptens starts the inflammatory process.Reference Djalilian and Memar 1 Secondary infections may also occur as a result of traumatisation of the external ear canal skin by foreign objects that are used to relieve itching. Accumulation of soft or paste-like cerumen at the external ear may also cause itching by contact irritation.
Psychological factors may also be the underlying cause of an itchy ear. In one study, the histopathological and immunohistochemical analyses of external ear canal skin biopsies revealed findings that were not consistent with dermatitis.Reference Acar, Simsek, Oguztuzun, Zaim and Karasen 2 Furthermore, in a study by Acar et al., the skin prick test results of patients with isolated itching of the external ear canal did not support the diagnosis of allergic contact dermatitis.Reference Acar, Karadag, Karabulut, Babademez, Zaim and Karasen 10
In our study, possible causes of itching such as diabetes mellitus, renal disease, malignancy, dermatological or allergic disease were excluded via clinical history and physical examination. We found that subjective pruritus scores after treatment were significantly lower than those before treatment, in all groups. There was no statistically significant difference between the groups in terms of subjective pruritus scores after treatment. Our results suggest that the use of Castellani's paint or mechanical removal of non-impacted cerumen can provide effective symptomatic relief in patients with an itchy external ear canal that is comparable to topical steroid use.
In an attempt to achieve symptomatic relief, many physicians prescribe salicylic acid, acetic acid or boric acid solutions, alone or in combination with steroid-containing drops, creams or ointments. However, all of these treatment options can result in some unwanted effects; furthermore, they may be ineffective in some patients, and symptoms tend to recur after the treatment has ceased. A disadvantage of alcohol or boric acid solutions is that they have to be applied repeatedly by the patient. Castellani's paint, however, can be easily applied by the doctor and, as demonstrated in our study, a few applications are effective in achieving symptomatic control.
Short-term symptomatic control is frequently achieved in patients with an itchy ear with the use of topical steroids. In our study, subjective pruritus scores of the patients decreased significantly after using steroid-containing ear drops for 12 days. Although the erythema scores did not show a significant change with steroid treatment, there was a significant decrease in desquamation scores. Moreover, the external ear canal skin swab culture results revealed no significant changes after the use of steroid-containing ear drops. Our results suggest that the short-term use of steroid drops is effective both in suppressing the inflammatory process and in reducing symptoms. Long-term steroid treatment, however, is not preferred, because it can cause a decrease in keratinocytes, permanent skin atrophy and telangiectasia.Reference Li and Cruz 11 , Reference Kolbe, Kligman, Schreiner and Stoudemayer 12
Topical immunosuppressive agents have emerged as potential alternatives that do not cause side effects related to steroid usage. Recently, the topical use of two immunomodulatory drugs, pimecrolimus cream and tacrolimus ointment, was approved by the US Food and Drug Administration (FDA) in the treatment of atopic dermatitis.Reference Meurer, Fartasch, Albrecht, Vogt, Worm and Ruzicka 13 , Reference Amrol, Keitel, Hagaman and Murray 14 Pimecrolimus inhibits T cell activation by preventing the transcription of cytokines such as interleukins 2, 4 and 10 and interferon gamma, and it inhibits the release of inflammatory substances from mast cells.Reference Amrol, Keitel, Hagaman and Murray 14 Because of a potential risk of cancer development, however, the FDA recommends these agents only as a second-line treatment, for short-term, intermittent use, in patients with atopic dermatitis who do not respond to other treatments. Thus, pimecrolimus should be reserved as a short-term, second-line option in the treatment of an itchy ear.
Castellani's paint is frequently used in otolaryngological practice for its antiseptic, acidifying and dehydrating properties. It can be used topically as a reliable, efficient and cost-effective treatment in bacterial and mycotic infections of the external ear canal. Gultekin et al. showed that the passage of Castellani's paint into the middle ear did not affect distortion product otoacoustic emissions.Reference Gultekin, Yener and Ozdemir 8 However, the effect of Castellani's paint on external ear canal itching is not known. In our study, we demonstrated that Castellani's paint significantly decreased erythema, desquamation and pruritus scores in patients with an itchy external ear canal. It also caused a decrease in the reproduction density of the normal flora bacteria, without affecting the type of bacteria that colonised on the external ear canal skin.
-
• This study investigated the effects of Castellani's paint on symptomatic relief and skin flora in patients with an itchy external ear canal
-
• Itchy ear aetiology and best treatment remain unclear
-
• Various topically applied medications are used in an attempt to achieve symptomatic control
-
• Each treatment option has limitations and alternative treatment approaches are needed to manage patients with itchy ears
-
• Castellani's paint is frequently used in otolaryngological practice for its antiseptic, acidifying and dehydrating properties
-
• Castellani's paint significantly decreased erythema, desquamation and pruritus scores in patients with an itchy external ear canal
Patients with an itchy ear and normal otoscopic findings do not necessarily have normal external ear canal flora. In a study by Karakuş et al., external ear canal skin swab cultures taken from patients with asteatosis and itching revealed bacterial pathogenic flora in 13.1 per cent and mycosis in 1.3 per cent of the ears.Reference Karakuş, Arda, Ikincioğullari, Gedikli, Coşkun and Balaban 4 In our study, microbiological evaluation of 228 external ear canal skin swab cultures revealed bacterial pathogenic flora in 6.5 per cent and mycosis in 1.7 per cent of the ears. Cevik et al. reported that patients using topical steroid ear drops for a persistent itchy ear had more parasites (demodex species) in their ear canals when compared to patients who did not use a local treatment.Reference Cevik, Kaya, Akbay, Yula, Yengil and Gulmez 15 It is important that the itchy ear treatment does not create a potential for secondary bacterial or mycotic infection. In this context, Castellani's paint is suggested to be effective and safe in the treatment of an itchy ear because of its antifungal and antibacterial properties.
In conclusion, Castellani's paint can be administered safely, effectively and easily, without affecting the type of bacterial and fungal growth of normal flora of the skin in patients with an itchy external ear canal. Further studies should be conducted to investigate the long-term effects of Castellani's paint in patients with an itchy ear.




