Introduction
Vocal fold injection augmentation is a known treatment modality for glottal closure insufficiency. Causes of glottal closure insufficiency include vocal fold paralysis, paresis, atrophy, sulcus vocalis, scarring and vocal fold deficiency after laryngeal surgery.Reference Rosen1
The original materials used in injection augmentation, such as paraffin, silicone and Teflon, caused foreign body reactions,Reference King and Simpson2–Reference Rubin4 and safer materials have since replaced them. Injectable materials are currently categorised as temporary or long-term. The temporary materials available are collagen-based, hyaluronic acid based and carboxymethyl cellulose based. The long-term materials available are calcium hydroxyapatite and autologous fat.Reference Misono and Merati5,Reference King and Simpson2,Reference Kwon and Buckmire6–Reference Lagier, Polle-Pelletier, Giovanni and Marie8 Injecting material into the vocal fold should improve glottal closure, and consequently improve patients’ voice. Other important features include easy application, low cost and appropriate duration of action (12–36 months).Reference King and Simpson2,Reference Simpson and Amin9–Reference Mallur, Morrison, Postma, Amin and Rosen11 The ideal injectable would also have similar biomechanical properties as the vocal fold component that is augmented.Reference Kwon and Buckmire6 None of the materials currently available for injection augmentation have all the characteristics desired of an ‘ideal’ injectable material.Reference Simpson and Amin9,Reference Lagier, Polle-Pelletier, Giovanni and Marie8
Injectable materials differ in their physicochemical structure and their rheological properties.Reference Sundaram, Voigts, Beer and Meland12 The degree of viscosity and elasticity affect both the stiffness of the material during injection and its ability to maintain its shape under the tension of vocal fold movement.Reference Sundaram, Voigts, Beer and Meland12,Reference Kimura, Mau and Chan13 The rheometric measurement of viscosity and elasticity under conditions that simulated vocal fold movement was shown to differ by 3 per cent between bovine collagen, Cymetra®, calcium hydroxyapatite and hyaluronic acid, and to differ substantially from the vocal fold cover.Reference Kimura, Mau and Chan13 No data are currently available regarding whether the different rheological properties of an injectable material influence the improvement in voice following injection augmentation of the vocal folds.
Voice improvement after injection augmentation of the vocal folds (Table 1) has been reported for collagen,Reference Kimura, Nito, Sakakibara, Tayama and Niimi14–Reference Hoffman, McCabe, McCulloch, Jin and Karnell16 hyaluronic acid,Reference Szkiełkowska, Miaśkiewicz, Remacle, Krasnodębska and Skarżyński7,Reference Upton, Johnson, Zelazny and Dailey17,Reference Wang, Chang, Jiang, Lai, De Virgilio and Wang18 carboxymethyl celluloseReference Mallur, Morrison, Postma, Amin and Rosen11 and ArteSense®.Reference Jang, Lee, Ahn and Son19 Vocal improvement was also reported with the long-standing injectables calcium hydroxyapatiteReference Rosen, Gartner-Schmidt, Casiano, Anderson, Johnson and Remacle20–Reference Amin25 and autologous fat.Reference Laccourreye, Papon, Kania, Crevier-Buchman, Brasnu and Hans26 Other reports that investigated a few injectables together showed improvement of the voiceReference Carroll and Rosen27–Reference Fritz, Peng, Born, Cerrati, Verma and Wang29 and glottal closure,Reference Andrade Filho, Carrau and Buckmire30 and an increased likelihood of undergoing permanent medialisation laryngoplasty.Reference Yung, Likhterov and Courey31 Comparable voice improvement was shown following the use of hyaluronic acid versus collagen,Reference Hertegård, Hallén, Laurent, Lindström, Olofsson and Testad32 and following autologous fat versus calcium hydroxyapatiteReference Zeleník, Walderová, Kučová, Jančatová and Komínek33 for vocal fold augmentation. A meta-analysis of voice outcome with calcium hydroxyapatite versus silicone thyroplasty also showed comparable results.Reference Shen, Damrose and Morzaria34 While both carboxymethyl cellulose and calcium hydroxyapatite are established vocal fold injectables, no published research has compared the two in terms of either voice improvement or action duration.
Table 1. Vocal improvement after vocal fold injection augmentation – literature review

*Exact distribution of direct laryngoscopy and in-office injection augmentation not specified. GRBAS = grade, roughness, breathiness, asthenia and strain scale; MPT = maximal phonation time; MFR = mean flow rate; S/Z ratio = standard test of vocal function (obtained by timing the longest duration that a patient can sustain the individual phonemes /s/ and /z/); VHI = Voice Handicap Index; GFI = Glottal Function Index; DSI = dysphonia severity index; CMC = carboxymethyl cellulose; HNR = harmonic-to-noise ratio; CaHA = calcium hydroxyapatite; CAPE-V = Consensus Auditory-Perceptual Evaluation of Voice; VPQ = voice performance questionnaire; VAS = visual analogue scale
When we first started treating patients with injection augmentations at our centre, we preferred to assess the success of vocal fold injection augmentations using a short-action injectable, namely carboxymethyl cellulose. Once the effect of the carboxymethyl cellulose injection wore off, the same patients were injected with calcium hydroxyapatite. Only after gaining experience did we eventually feel confident in using a long-action injection augmentation, namely calcium hydroxyapatite, for the first injection. This scenario of events created a research opportunity: specifically, the possibility of comparing voice improvement after injection augmentation using carboxymethyl cellulose or calcium hydroxyapatite in the same group of patients.
Materials and methods
This retrospective study included all patients treated in our clinic between July 2013 and February 2017 who received vocal fold injection augmentations for the treatment of glottal closure insufficiency confirmed by videostroboscopy. Study exclusion criteria included a patient's inability to provide informed consent and age of younger than 18 years. Demographic information, including patients’ age, gender and the cause of glottal closure insufficiency was collected. The study was approved by the Institutional Review Board of the Rambam Healthcare Campus (approval number 0021-17 RMB).
Injection augmentation protocol
Under video-endoscopic guidance, the designated material was injected transorally into the thyroarytenoid muscle. The injection materials were carboxymethyl cellulose (Radiesse Voice Gel; Merz North America, Franksville, Wisconsin, USA) and calcium hydroxyapatite (Radiesse Voice; Merz North America). The volume of material injected was determined visually, according to the glottic airway. The maximal total volume injected was 1 ml. If the injection was bilateral, the total volume used to inject both vocal folds was reported.
Voice assessment
Patients assessed their own voices using the Voice Handicap IndexReference Amir, Ashkenazi, Leibovitzh, Michael, Tavor and Wolf35 and the Glottal Function Index.Reference Bach, Belafsky, Wasylik, Postma and Koufman36 The ranges of these scales are 0–120 and 0–20, respectively. Objective voice assessment was conducted using the grade, roughness, breathiness, asthenia and strain (‘GRBAS’) scale,Reference Hirano37 with a score range of 0–15. Acoustic analyses were performed using the Praat program (Amsterdam, the Netherlands),Reference Boersma and Weenink38 and included assessment of jitter, shimmer and the harmonic-to-noise ratio. For the Voice Handicap Index, Glottal Function Index, grade, roughness, breathiness, asthenia and strain scale, jitter and shimmer, lower scores indicated better function. For the harmonic-to-noise ratio, a higher score indicated better function. The period between injection augmentation and the first follow-up appointment was two to four weeks.
Duration of action
The duration of action of the injectable materials was measured according to the time interval between the injection augmentation and: the next injection augmentation, the wearing off of the injection augmentation (according to patients’ report and videostroboscopy findings), ongoing effective injection augmentation at the last follow up, or the patient's demise.
Statistical analysis
Demographic descriptors were summarised as means (and standard deviations) for continuous variables and as percentages of total procedures for categorical variables. In order to evaluate the effect of injection augmentation on subjective and objective vocal parameters, we compared the Voice Handicap Index, Glottal Function Index, grade, roughness, breathiness, asthenia and strain scale, jitter, shimmer, and harmonic-to-noise ratio before injection and at two to four weeks after injection. Differences between injection materials in each outcome measure were analysed via the Wilcoxon non-parametric (paired) test. We considered p-values of less than 0.05 as statistically significant. Statistical analysis was performed using SPSS® software, version 21.
Results
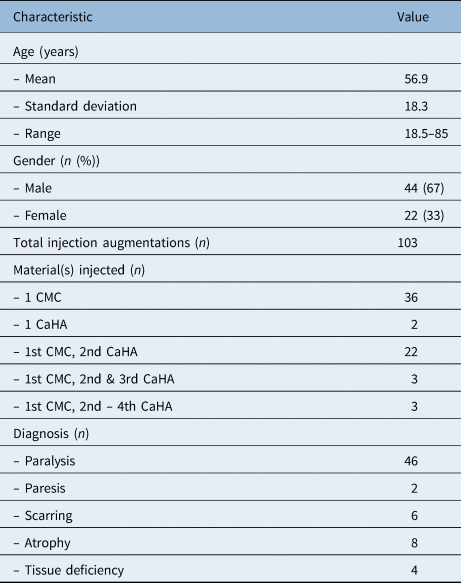
During the study period, 66 patients received 103 in-office vocal fold injection augmentations. Patients’ mean age was 56.9 years (standard deviation ± 18.3 years); the male to female ratio was 2:1. The patient population is characterised in Table 2. Data were incomplete for some of the measures assessed.
Table 2. Demographic and clinical characteristics of individuals who received vocal fold injection augmentation

CMC = carboxymethyl cellulose; CaHA = calcium hydroxyapatite
In total, 64 patients received an injection with carboxymethyl cellulose. Of these, 28 became symptomatic again after the effect of the carboxymethyl cellulose injection had worn off, and received one or more subsequent injections with calcium hydroxyapatite. Six patients received more than one calcium hydroxyapatite injection (Table 2). For the current study, voice symptoms were analysed according to the end results of the first calcium hydroxyapatite. Two patients received their first injections after we had started administering calcium hydroxyapatite as the first injection.
The indication for injection augmentation was glottal closure insufficiency, due to: vocal fold paralysis (n = 46), vocal fold paresis (n = 2), scarring (n = 6), atrophy (n = 8) or vocal fold tissue deficiency after laser cordectomy for laryngeal cancer (n = 4). The mean injection volume was 0.8 ml (range, 0.45–1 ml) for each patient's treatment. Eight patients received bilateral injections.
All patients who had two or more injection augmentations had complete resorption of carboxymethyl cellulose prior to the calcium hydroxyapatite injection, with a time lapse between injections of more than three months.
Outcomes
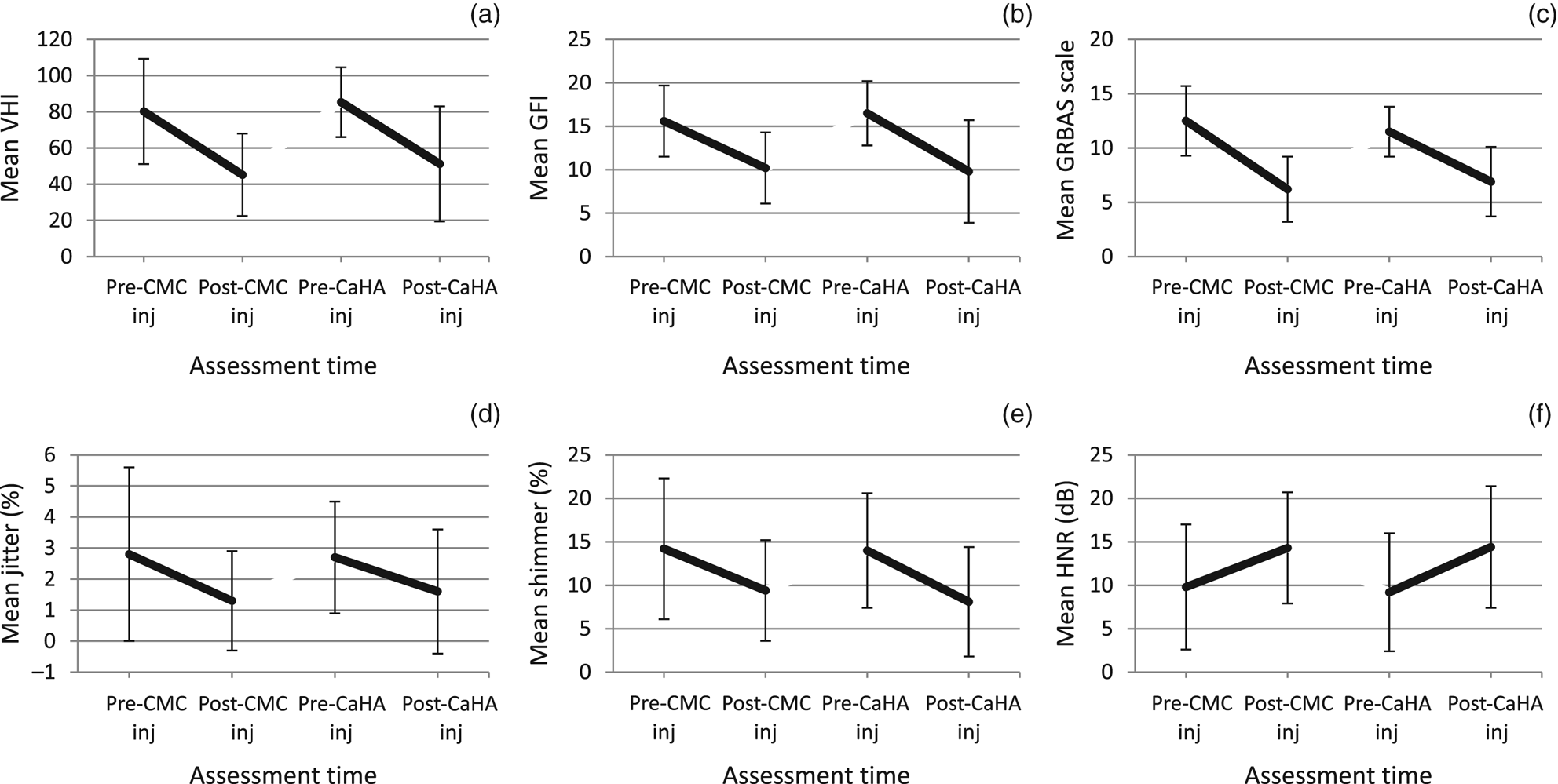
Patients’ voice significantly improved after injection augmentation using either carboxymethyl cellulose or calcium hydroxyapatite (Table 3). As the same individuals received both carboxymethyl cellulose and calcium hydroxyapatite, voice improvement after injection augmentation could be compared between these injectables. Among the patients who received their first injection augmentation with carboxymethyl cellulose and their second injection augmentation with calcium hydroxyapatite (n = 28), voice quality improved significantly after both injection augmentations according to all the parameters assessed (p < 0.001). The differences between pre-carboxymethyl cellulose and pre-calcium hydroxyapatite assessments, and between post-carboxymethyl cellulose and post-calcium hydroxyapatite measurements, were not statistically significant for Voice Handicap Index, grade, roughness, breathiness, asthenia and strain scale, jitter, shimmer or harmonic-to-noise ratio (Figure 1).

Fig. 1. Vocal characteristics of patients who had a first vocal fold injection augmentation with carboxymethyl cellulose (CMC) and a second injection with calcium hydroxyapatite (CaHA). The graphs show mean scores for: (a) Voice Handicap Index (VHI) (n = 18) (scale range = 0–120; a higher score indicates more voice symptomsReference Amir, Ashkenazi, Leibovitzh, Michael, Tavor and Wolf35), (b) Glottal Function Index (GFI) (n = 18) (scale range = 0–20; a higher score indicates more symptoms related to glottal closure insufficiencyReference Bach, Belafsky, Wasylik, Postma and Koufman36), (c) grade, roughness, breathiness, asthenia and strain (GRBAS) scale (n = 18) (score range = 0–15; a higher score indicates a worse voiceReference Hirano37), (d) jitter (n = 19) (jitter of 1.040 per cent was considered the threshold for pathologyReference Boersma and Weenink38), (e) shimmer (n = 19),Reference Boersma and Weenink38 and (f) harmonic-to-noise ratio (HNR) (n = 19) (if 99 per cent of the voice energy is periodic and 1 per cent is noise, the harmonic-to-noise ratio is 10*log10(99/1) = 20 dB. A harmonic-to-noise ratio of 0 dB indicates that the harmonics and the noise have the same energy level).Reference Boersma and Weenink38 All parameters examined improved significantly from pre- to post-injection assessments, both with carboxymethyl cellulose injection (p < 0.001) and with calcium hydroxyapatite injection (p < 0.001). For all parameters examined, the difference between values for pre-carboxymethyl cellulose injection and pre-calcium hydroxyapatite injection, and the differences between post-carboxymethyl cellulose injection and post-calcium hydroxyapatite injection, did not differ statistically.
Table 3. Summary of voice analysis following injection augmentation with carboxymethyl cellulose and calcium hydroxyapatite

SD = standard deviation; VHI = Voice Handicap Index; CMC = carboxymethyl cellulose; CaHA = calcium hydroxyapatite; GFI = Glottal Function Index; GRBAS = grade, roughness, breathiness, asthenia and strain; HNR = harmonic-to-noise ratio
The action duration of carboxymethyl cellulose versus calcium hydroxyapatite was assessed for 71 injection augmentations: 39 carboxymethyl cellulose and 32 calcium hydroxyapatite injections. The action duration was determined by calculating the time lapsed until: the subsequent injection augmentation (n = 37), the completion of action in the follow up and patients’ lack of interest in a second injection augmentation (n = 7), ongoing action in the follow up (n = 25), and patients' demise during follow up for non-laryngeal reasons (n = 2). Excluded from this analysis were: cases of unsuccessful injection augmentation (n = 17), loss to follow up (n = 14) and the spontaneous recovery of vocal fold movement (n = 1).
The duration of action was significantly shorter for carboxymethyl cellulose than for calcium hydroxyapatite. At nine months, the action of the injectable materials was ongoing in 26 per cent of cases following carboxymethyl cellulose injections and in 86 per cent of cases following calcium hydroxyapatite injections (p = 0.002, hazard ratio = 3.2 (95 per cent confidence interval (CI) = 1.6–6.6)). The median duration of action was 6.8 months (95 per cent CI = 5–8.6) for carboxymethyl cellulose and 13.7 months (95 per cent CI = 10.9–16.6) for calcium hydroxyapatite.
The duration of action of injectable materials was not associated with patients' gender, age or any of the pre-injection vocal parameters examined (Voice Handicap Index, Glottal Function Index, grade, roughness, breathiness, asthenia and strain scale, jitter, shimmer, or harmonic-to-noise ratio). In addition, a comparison of vocal fold paralysis versus other causes of glottal closure insufficiency showed no association with action duration for either carboxymethyl cellulose or calcium hydroxyapatite.
Discussion
Numerous reports have shown that injection augmentation for medialisation of the vocal folds improves the voice of patients with glottal closure insufficiency.Reference Szkiełkowska, Miaśkiewicz, Remacle, Krasnodębska and Skarżyński7,Reference Mallur, Morrison, Postma, Amin and Rosen11,Reference Kimura, Nito, Sakakibara, Tayama and Niimi14,Reference Kimura, Nito, Imagawa, Tayama and Chan15,Reference Upton, Johnson, Zelazny and Dailey17–Reference Amin25,Reference Powell, Carding, Birdi and Wilson28,Reference Fritz, Peng, Born, Cerrati, Verma and Wang29,Reference Yung, Likhterov and Courey31–Reference Zeleník, Walderová, Kučová, Jančatová and Komínek33 However, most reports that investigated voice improvement in this setting did not compare between injection materials (Table 1).Reference Hertegård, Hallén, Laurent, Lindström, Olofsson and Testad32–Reference Shen, Damrose and Morzaria34 While both carboxymethyl cellulose and calcium hydroxyapatite are established vocal fold injectables, no published research has compared the two injectable materials in terms of voice improvement or duration of action. The use of the two materials at our centre provided a unique research opportunity. All patients in the study who were treated before January 2016 were first injected with carboxymethyl cellulose. Once the effect of the injected carboxymethyl cellulose had worn off, symptomatic patients who had returned to their baseline level of glottal closure insufficiency were subsequently injected with calcium hydroxyapatite.
The strength of this study is that voice improvement following the injection of two materials was compared in the same patients. We found no differences in terms of the improvement of any of the voice parameters examined following injection augmentation between injection with carboxymethyl cellulose and calcium hydroxyapatite.
The injection materials compared contain some similar and some different compounds. According to the manufacturer, Radiesse Voice Gel is a semi-solid cohesive implant, consisting of glycerine and sodium carboxymethyl cellulose in a phosphate buffer solution. In contrast, Radiesse Voice is an injectable implant containing synthetic calcium hydroxyapatite microspheres, suspended in an aqueous carrier gel that contains glycerine, sodium carboxymethyl cellulose and sterile water.
• Vocal fold injection augmentation is a known treatment for glottal closure insufficiency
• Carboxymethyl cellulose and calcium hydroxyapatite are established vocal fold injectables
• No published research has compared the two injectables in terms of voice improvement or action duration
• Initially, patients were treated using carboxymethyl cellulose; once effects had worn off, the same patients were injected with calcium hydroxyapatite
• This scenario enabled comparison of voice improvement and action duration between the two injectables, in the same patients
The observed activity of the two preparations differed. During the treatment, the injection of calcium hydroxyapatite through the needle required more force than did the injection of carboxymethyl cellulose. Moreover, carboxymethyl cellulose immediately dispersed along the vocal fold, while calcium hydroxyapatite dispersed only locally. This stems from the different viscoelastic properties of the injectables. In addition, as expected, the duration of action of calcium hydroxyapatite was substantially longer than that of carboxymethyl cellulose. Although calcium hydroxyapatite is considered a long-term injectable, its duration of action is limited and several recurrent injection augmentations are required throughout a patient's lifetime.
We conclude that voice improvement after injection augmentation depends mainly on the improvement of glottic closure, rather than the injection material used. Therefore, we believe that future searches for a new injectable material for glottal closure insufficiency should focus on extending the duration of action of the injectable material.
Competing interests
None declared