Any event resulting in the emergent evacuation of a children’s hospital would, by definition, be a disaster requiring regional cooperation. 1 There has been a call for improved pediatric disaster planning and tools to help allocation of resources. 2 - Reference Cohen, Murphy, Ahern and Hackel 4 However, there are no tools for assessing neonatal and pediatric inpatients for resource needs in an emergency evacuation.Reference Cohen, Murphy, Ahern and Hackel 4 , Reference Antommaria, Sweney and Poss 5
Preparedness for pediatric disaster response to date is poor.Reference Gausche-Hill 6 The National Advisory Committee on Children and TerrorismReference Diaz, Dinnin, Green, Kelter, Maniece-Harrison, Marans, Mickalide, Mollica, Ricciardi, Rumm and Wright 7 has recommended improving pediatric preparedness at local, state, and federal levels. The Institute of Medicine 2 recommends developing disaster plans that address pediatric preparedness and surge capacity. Resource availability is a critical aspect of disaster preparedness. KleinReference Klein, Pepe, Burkle, Nagel and Swienton 3 analyzed triage during Hurricane Katrina and found that triage assessment tools need to be developed for accessing care and resources. During the Northridge Earthquake, basic needs were not anticipated, and systems were not in place to transport patients to medical care or to community resources.Reference Stratton, Hastings and Isbell 8 Furthermore, disaster response to Hurricane Katrina revealed that effective communication and resource mobilization were major challenges.Reference Mattox 9
The optimal triage tool would be simple and would address three major issues identified in the wake of Katrina as described above: (1) evacuation, (2) surge capacity, and (3) communication. Ideally, all institutions regionally, or even nationally, would implement it. Currently available triage tools are based on severity of illness or predictors of mortality, and were validated for patients in the prehospital setting or at the time of hospital admission. Thus, they may not be applicable to patients who have had more prolonged hospitalizations.Reference Meadow, Lagatta and Andrews 10 - Reference Antommaria, Sweney and Poss 12 Even a sequential daily scoring system predicting a worst-case scenario of 50% mortality in the most critically ill pediatric patient does not address the question of how to triage this patient for hospital evacuation.Reference Leteurtre, Duhamel and Grandbastien 13 Available triage tools do not meet these 3 needs in the setting of disaster necessitating the evacuation of a single large children’s hospital, let alone multiple institutions.
Approximately 250 pediatric hospitals nationwide account for 2% of the total number of hospitals in the United States. 14 Since children account for 26% of the population, 15 this gap represents a major vulnerability in disaster response. This vulnerability would be more apparent should a disaster necessitate evacuation of a major pediatric center. Nearby facilities would need to increase surge capacity rapidly to accommodate this influx of patients. This would be particularly problematic for high acuity complex patients whose management requires special resources that may not be readily available at nearby centers.
The purpose of this project was to develop a disaster triage tool for the evacuation of hospitalized neonatal and pediatric patients. The Stanford University Institutional Review Board designated the research protocol as a quality improvement project.
METHODS
Study Design
Since a rapid triage tool that would address the needs for our pediatric inpatient population during a disaster requiring complete vertical evacuation from our hospital does not exist, we modified an existing neonatal disaster triage tool called Triage by Resource Allocation In Neonates (TRAIN).Reference Cohen, Murphy, Ahern and Hackel 4 , Reference Cohen 16 , Reference Carbine, Cohen and Hopper 17 It uses resource allocation to determine the level of transport required for hospital evacuation of neonatal intensive care unit populations. Primary outcome was to use the tool to determine the number of each level of transport required for vertical evacuation of our hospital. Secondary outcome was to improve the efficiency of obtaining information about specific transport needs for evacuation.
This project received executive support and the team drew from multiple specialties including emergency management, pediatric hospital medicine, neonatology, medical transport, and clinical nursing. Since the neonatal tool was found to be effectiveReference Cohen 16 - Reference Cohen, Murphy, Ahern and Hackel 18 during statewide drills, this triggered an institution-wide effort to standardize the tool for all neonatal and pediatric inpatients at Lucile Packard Children’s Hospital Stanford (LPCHS).
LPCHS is a tertiary care 311 bed freestanding academic hospital located in Palo Alto, CA, USA. The facility contains 5 acute care units, 3 intensive care units, 2 obstetric units as well as perioperative services. It is part of the Stanford Children’s Health network and affiliated with Stanford University School of Medicine.
Executive sponsorship from administrative and emergency management leadership provided resources for the creation of the TRAIN Work Group. The work group consisted of clinical providers, including nurses, physicians, transport specialists, and administrators. Nurses initially used the neonatal version of TRAIN to assess its appropriateness in the general pediatric population. Plan Do Study Act (PDSA) cycles were used to expand the applicability of neonatal TRAIN to incorporate all neonatal and pediatric patients within the hospital. Experts from specialty areas with guidance from local emergency medical services (EMS) guidelines facilitated modification of the tool during each cycle. This observational study took multiple cycles of patient data to generalize the disaster triage tool and apply it to the entire neonatal and pediatric inpatient census using the modified TRAIN tool. We used 5 PDSA cycles over a 5-month period. The team met at least 2 times per cycle to refine the tool. Each patient was assessed by resource needs, potential resources not addressed by the original tool, and then evaluated for appropriate level of transport by the expert panel. The panel then defined each category and level of transport.
The qualitative data reviewed included bedside visual assessments and chart review. Appropriate levels of transportation were based on local (EMS) transport guidelines and expert panel discussion. Primary data about transport resource needs to evacuate the hospital were collected after tool refinement to include both neonatal and pediatric inpatient populations. Secondary outcome was assessed using a time study performed during a mandated statewide disaster exercise requesting information for evacuation from all units in the hospital without the tool and with a manual tool. Finally, we used previously collected data from the original neonatal TRAIN and compared it to the subset of neonatal data collected from the new TRAIN tool to ensure that the new tool still applied to this patient population.
To assure data quality, 2 separate nurses received specific training regarding the tool usage by the expert panel. They gathered information independently and were blinded to each other’s assessments during data collection. Their assessments were then compared to level of transport required for accuracy.
Statistical Analysis
To assess the accuracy of the original neonatal triage tool for generalized neonatal and general pediatric inpatient populations, we reviewed qualitative measures to determine the level of transport of each patient evaluated. Using the neonatal tool, the expert panel decided whether the determined level of transport was appropriate for each patient and collected aggregate numbers. The expert panel continued to adjust the tool until all types of resources required for patient transport met saturation.
We compared the data set percentages from neonatal data previously collected with the original tool to data collected with the new tool over the course of the study. Furthermore, during a mandated statewide disaster drill, time to complete requests for information on transport requirements without the tool was measured and compared against a single nurse using the tool to gather the information requested.
RESULTS
We evaluated a total of 1382 patients both visually and through electronic chart review over 10 random days. Accordance between visual assessment and electronic chart review reached 96.3% (Figure 1). After incorporating the final PDSA cycle, we used the TRAIN tool on the patient population on a random day (Figure 2). We reviewed the subset of neonatal patients and compared categorization breakdown to previously obtained data from the original neonatal version of the tool. The proportion of patients who require critical care transport or higher was the same (46%).

Figure 1 Example of Sunflower Plot Representing Electronic Chart Review Versus Visual Assessment.

Figure 2 Estimated EMS Transport Needs Based on TRAIN. Abbreviations: BLS, Basic Life Support; ALS, Advanced Life Support;CCT, Critical Care Transport; EMS, emergency medical services; TRAIN, Triage by Resource Allocation In Neonates.
The time study data was collected during a mandatory 2 hour statewide disaster exercise. At the end of the exercise, no hospital units had completed their assessment of transport needs for their patients. A single nurse determined the transport needs by visual assessment of the entire neonatal and pediatric inpatient populations (n=148) in 57 minutes.
DISCUSSION
The TRAIN triage tool we developed initially for neonatal intensive care unit evacuation addresses all 3 of the needs defined above.Reference Cohen, Murphy, Ahern and Hackel 4 This tool was modified to be applicable to all neonatal and pediatric inpatients (Triage by Resource Allocation for INpatients). The new TRAIN tool categorizes inpatients according to their resource needs at the time of a disaster. The implementation of this tool facilitates (1) rapid determination of resource requirements for pediatric transport, (2) augmentation of surge capacity by identifying candidates for rapid discharge or transfer to lower levels of care, and (3) communication with receiving institutions and supporting agencies such as EMS.
We continue to use TRAIN in institutional and statewide disaster drills. Our experience has shown that TRAIN decreases the time needed to assess resource needs for the movement of inpatients in our institution. Without TRAIN, determining transport needs relies upon staff on each unit subjectively assessing their patients. However, a single nurse using TRAIN objectively was able to assess the entire inpatient population and reported transportation needs in less than 1 hour. This expedited the ability to more accurately request resources from outside institutions and agencies. At the same time, inpatients with low resource needs were identified for potential rapid discharge which could augment surge capacity. A lack of standardization may lead to incorrect resource requests which could raise ethical questions about transport decisions.
Although we did not achieve 100% accordance, we had over 96% agreement between the visual assessment and electronic chart review. This encouraged us to automate the TRAIN tool within the electronic health record which allows an automatic triage process for patient evacuation with minimal impact to daily workflow. In the event the automated tool is not available, patients can still be triaged quickly with the manual tool.
This tool is designed for hospital disaster pre-planning to give an estimate of transport resource needs in order to mobilize patients for evacuation or rapid discharge. It serves as a guide to identify patient needs to assist the organization in requesting resources for transport and ongoing care. This tool does not determine the level of care or acuity of the patient or identify receiving institutions for evacuated patients. In recognition that neonatal and pediatric patients often have rapid status changes within hours as well as acute changes due to disaster, medical personnel must verify TRAIN categorization at the time of evacuation. Provider expertise is still required for medical transfers and discharge needs such as medication or durable medical equipment orders.
Using TRAIN routinely allows an institution to understand its vulnerabilities and plan for future disasters. Although designed specifically for evacuation, TRAIN has been used to optimize patient flow by identifying patients with lower resource needs who could potentially be transitioned from critical to acute care or discharged home. This has implications for increasing surge capacity within the hospital.
Adopting TRAIN regionally would facilitate the ability to communicate resource allocation needs for inter-hospital patient movement. Reviewing our TRAIN data over time with local emergency agencies and county EMS has improved their awareness of our hospital’s potential needs during disaster and resulted in better collaboration. The TRAIN report can be shared with outside agencies involved in disaster mitigation such as county EMS and regional emergency operation centers. Although the study and implementation of TRAIN occurred at a single institution, we believe it is most powerful when all institutions within a region use it to facilitate collaboration and communication. It has helped us understand the gaps between our transport needs in the case of vertical evacuation and available resources at the local and regional level which will need to be allocated across the county, state, and nation depending on the magnitude of a disaster.
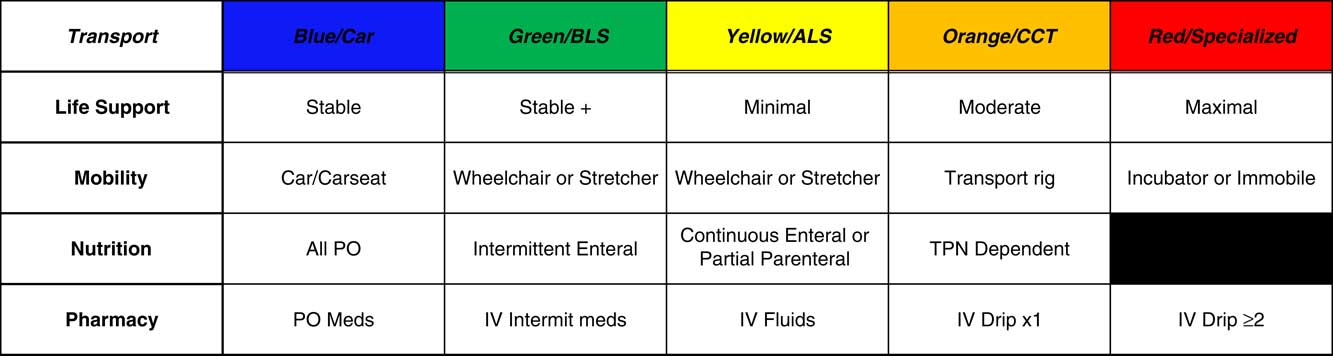
TRAIN was presented at multiple local and national conferences. Based on feedback from these sources, the tool was modified to better delineate differences between basic and advanced life support (Figure 3). TRAIN has been included in the California Association of Neonatologists disaster planning toolkit,Reference Carbine, Cohen and Hopper 17 has been presented at the national Integrated Training Summit,Reference Lin, Taylor and Wintch 19 and now has been incorporated into the course on Pediatric Disaster Response and Emergency Preparedness funded by the Department of Homeland Security and Federal Emergency Management Agency. 20

Figure 3 Triage by Resource Allocation for INpatients [TRAIN] Tool.
At an institutional level, an obstetrical version of TRAIN has been developed and implemented.Reference Daniels, Oakeson and Hilton 21 We expect that this will shortly be automated into the electronic health record. Validation studies are ongoing for TRAIN in the adult inpatient population at Stanford University Hospital.
To date, this tool has only been tested in exercises within our institution, in county disaster exercises and across neonatal intensive care units within our region. It has garnered intense interest by state disaster planners for the movement of hospitalized patients, the National Disaster Medical System and over 43 institutions and agencies across the nation. Future studies are needed to evaluate, improve, and validate the TRAIN tool at multiple institutions across the nation.
CONCLUSION
We believe the TRAIN tool helps address 3 goals of hospital disaster mitigation: evacuation, surge capacity, and communication. We have successfully modified, tested and implemented the TRAIN tool for the entire pediatric inpatient population. We have also leveraged the electronic health record by creating an algorithm to automate the TRAIN tool to enhance our hospital disaster pre-planning with minimal impact to daily workflow.
TRAIN would be most beneficial when all hospitals and agencies within a region adopt its use. Incorporating TRAIN into daily management and routine hospital disaster drills allows hospitals to collaborate with each other using a common language. It also can inform outside agencies regarding resource needs for disaster planning. As seen in Hurricanes Katrina and Sandy, patient movement across state lines implies that regional disasters can have national impact. Thus, we would urge the implementation of TRAIN by all pediatric hospitals nationally.
Funding
No funding was secured for this study.
Conflicts of Interest
The authors have no conflicts of interest to disclose.
Author Contributions
Dr Lin conceptualized and designed the study, performed initial analyses of the data, drafted the initial manuscript, and approved the final manuscript as submitted.
Ms. Taylor collected and compiled the data for this study, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Dr Cohen conceptualized the original triage tool in the neonatal population, assisted in the design of the study, critically reviewed and revised the manuscript, and approved the final manuscript as submitted.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/dmp.2017.139