Introduction
Nation-wide, there has been a growing epidemic of opioid narcotic abuse. The US Centers for Disease Control and Prevention (CDC; Atlanta, Georgia USA) has reported that the age-adjusted rate of drug overdose deaths has more than tripled in 2016 compared to 1999.Reference Hedegaard, Warner and Miniño1 Specifically, the number of overdose deaths involving opioids (both prescription and illegally obtained) was five-times higher in 2016 than in 1999.2 Naloxone, a non-selective and competitive opioid receptor antagonist, was patented and approved by the US Food and Drug Administration (FDA; Silver Spring, Maryland USA) for use several decades ago.Reference Dean, Bilsky and Negus3 While serious complications, such as pulmonary edema, are well-documented, these are rare, and the benefits of administration often heavily outweigh the associated risks.Reference Tintinalli, Stapczynski, Ma, Yealy, Meckler and Cline4
Given the safety profile and preponderance of opioid overdose, Advanced Life Support (ALS) providers have been carrying naloxone for many years. Early in 2016, the National Emergency Medical Services Advisory Council (NEMSAC; Washington, DC USA) received a request from the National Highway Traffic Safety Administration (NHTSA; Washington, DC USA) to allow for wider use of opioid antagonists such as naloxone, specifically for Basic Life Support (BLS) providers such as emergency medical responders (EMRs) and emergency medical technicians (EMTs). This prompted meetings later that year, with a formal change in the Scope of Practice Model in 2017.5 The change noted:
The benefits outweigh the risks of incorporating opioid antagonist administration into the scope of practice at the EMR and EMT level for patients with suspected opioid overdose. EMRs and EMTs shall only undertake the practice if they possess the necessary educational preparation, experience, and knowledge to properly administer an opioid antagonist via unit-dose, premeasured, intranasal or auto-injector routes.
This change was made despite a lack of applicable literature at the time comparing ALS to other responders, such as BLS, as they deemed the benefits to outweigh the risks.6
Previously, BLS providers were limited to simple maneuvers such as airway support in suspected drug overdoses. However, studies have demonstrated that the administration of naloxone is within the capability of trained BLS personnel.Reference Davis, Southwell, Niehaus, Walley and Dailey7 Similarly, studies are now demonstrating how BLS providers can effectively administer naloxone.Reference Gulec, Lahey, Suozzi, Sholl, MacLean and Wolfson8, Reference Weiner, Mitchell, Temin, Langlois and Dyer9 Other sources have acknowledged the potential for earlier delivery of naloxone if BLS is allowed to carry it, though data to support this further have been limited.Reference Belz, Lieb, Rea and Eisenberg10
While opioid overdose events and deaths have increased across the United States, the Northeast, Midwest, and South regions showed significantly higher rates compared to other areas. Delaware has consistently been in the top one-third of states for drug overdose deaths per population.Reference Hedegaard, Warner and Miniño1 In an effort to curtail this trend, the Delaware Office of Emergency Medical Services (OEMS; New Castle, Delaware USA) developed a pilot program to allow certain, specially trained BLS providers to carry and administer naloxone in carefully selected patient populations. This pilot program was then studied to evaluate the change in patient condition with BLS naloxone administration, as well as to see if there was a significant time difference in administration compared to ALS.
Methods
This was a retrospective, observational study using data collected from February 2014 through April 2015 throughout the Delaware State BLS Naloxone pilot program. The study was approved by review from the Christiana Care Health System Institutional Review Board (Newark, Delaware USA). The State of Delaware has a total population of approximately 960,000 and a total square mileage of 1,949. The state is comprised of three counties with a population per square mile of 460.8 as of 2010, making it one of the most densely populated states in the country. 11 A total of 72 prehospital BLS agencies exist throughout the state. Delaware BLS providers receive their state certification from the Delaware State Fire Prevention Commission (DSFPC; Dover, Delaware USA), and most in-state training is provided by the Delaware State Fire School (DSFS; Dover, Delaware USA). Delaware utilizes a two-tiered Emergency Medical Services (EMS) system, with separate BLS and ALS response. This system is based on Medical Priority Dispatch, with alpha through echo response. A BLS crew is sent alone for alpha and bravo, while both BLS and ALS are deployed for charlie through echo. State EMS medical direction is provided by the Delaware OEMS utilizing board-certified emergency medicine physicians.
In July 2013, the Delaware OEMS and DSFS devised a pilot protocol to allow BLS to have standing orders to permit the administration of intranasal naloxone in suspected opioid overdose cases. The specific product utilized was 1mg Narcan (Adapt Pharma, Inc.; Radnor, Pennsylvania USA) intranasal via the LMA MAD Nasal device (Teleflex, Inc.; Research Triangle Park, North Dakota USA). A total of 14 out of 72 state prehospital BLS agencies participated in the pilot protocol. Pilot BLS agencies attended a three-hour training session on the indications and administration of naloxone, including lectures and skills-based learning. Following this training, participants were required to demonstrate proficiency and pass a written quiz before being authorized to carry and administer naloxone. These educational materials and assessments were developed and reviewed by the state OEMS and DSFS with training provided by the DSFS instructors.
The pilot protocol trained BLS companies to consider administration of naloxone if there were indications of possible opioid overdose; such indications included respiratory distress or apnea, decreased responsiveness, appropriate history provided by bystanders, or surrounding paraphernalia. The BLS crews were instructed to continue appropriate airway management, while looking for other signs of altered mental status with their alternative standing orders, such as hypoglycemia or trauma. If naloxone administration was deemed appropriate, the pilot protocol (Figure 1) called for assembly and application of the MAD device into the patient’s larger nares, subsequently providing 1mg of naloxone. A second dose of naloxone 1mg was administered in the second nares if the patient did not have a significant response within two minutes. In addition to BLS, ALS crews are dispatched to all opiate overdose, respiratory distress, or unresponsive persons, which would have included nearly all the patients in this study who received naloxone. If BLS arrived to find a patient who unsuspectingly met naloxone criteria, ALS was contacted for assistance. The BLS crews would then converge with ALS, unless the nearest appropriate hospital was closer than the paramedic unit. Patients successfully revived with naloxone were not able to refuse service without contact to Medical Control.
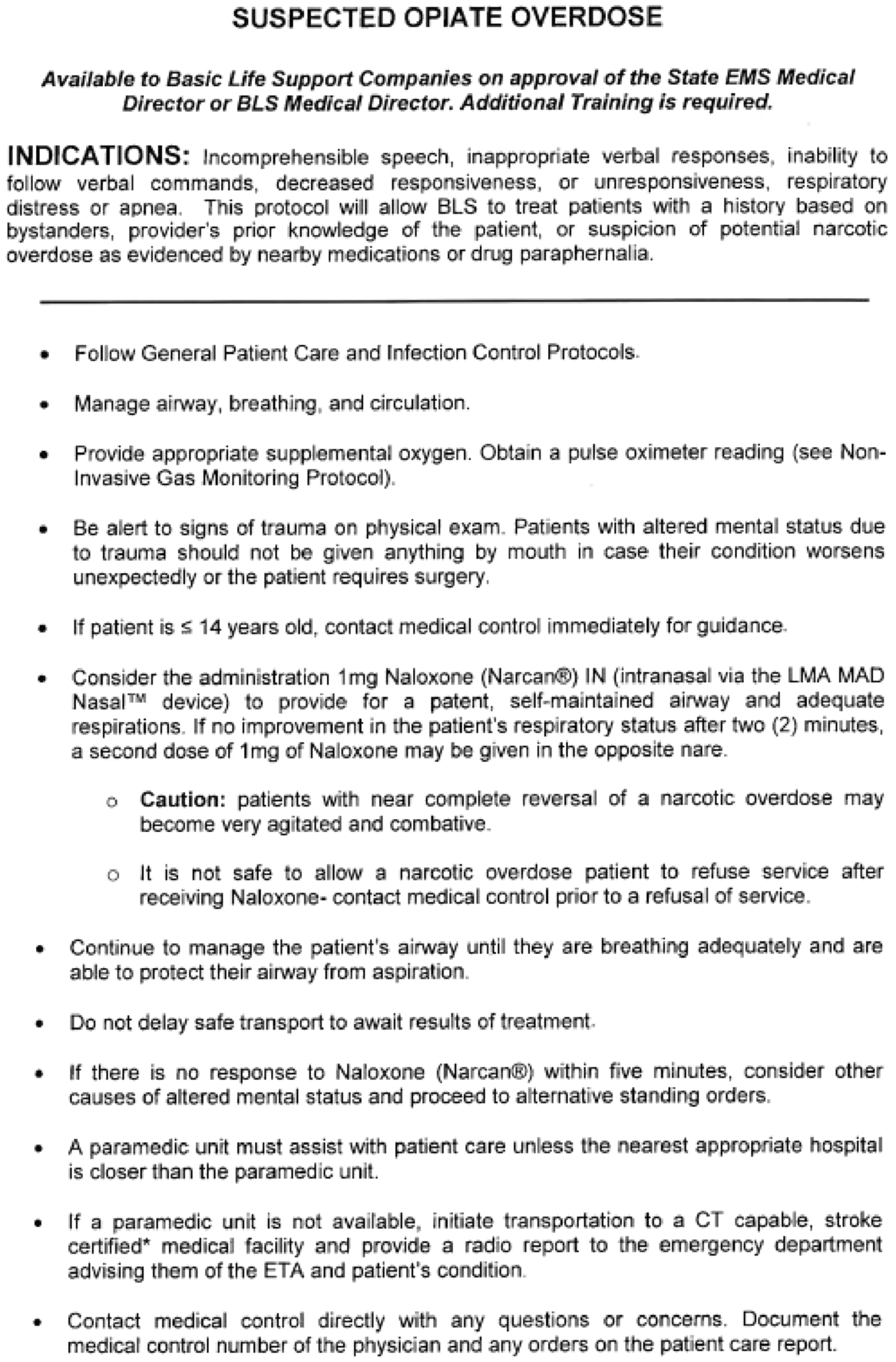
Figure 1. Delaware OEMS Suspected Opiate Overdose Standing Orders Protocol.
Throughout the pilot study, crews were required to fill out a data collection form devised by the Delaware OEMS. In addition to demographics information, this form called for documentation of the initial vital signs, including respiratory rate (RR), pulse oximetry (spO2), level-of-consciousness, heart rate (HR), blood pressure, and blood glucose level. The providers then recorded if ALS was available on-scene, and their initial interventions. This section included options to document if and why narcotic overdose was initially suspected. The patient would then be re-evaluated following any intervention, again with documentation of vital signs and any comments/complications. The data forms for incidents in which naloxone was administered by BLS were collected and reviewed during the BLS pilot program and compared to incidents in which ALS crews administered naloxone from a comparatively similar time. As the ALS crews were not involved in the BLS study protocol, ALS data were collected from aggregate state-wide collection. The study patients in the ALS group received no intervention from BLS crews in the pilot program carrying naloxone. In order to ensure accuracy and appropriateness of naloxone use, the forms were reviewed and signed by a provider with advanced training en route or upon arrival to the emergency department (ED) to include paramedics, registered nurses, mid-level providers, respiratory therapists, and physicians. Each data collection form was then collected by OEMS and reviewed by the researchers.
The ALS crews already had opioid overdose protocols in place, giving them the capability to administer naloxone intranasally, similar to the BLS pilot program, but also via intravenous, intraosseous, and intramuscular routes determined by the provider’s discretion. This was not changed for this study. The study protocol compared vital signs before and after naloxone between BLS (pilot group) and ALS (control group) patients, as well as the time of BLS arrival to the time of naloxone administration by BLS or ALS providers. In order to standardize the time references, the recorded times were pulled directly from the state-wide electronic patient care report system, which utilizes universal, synchronized times throughout the counties in the state. Data were analyzed using paired and independent sample t-tests, as well as chi-square, as appropriate.
Results
A total of 131 incidents of naloxone administration were reviewed from the study period. Of these incidents, 62 patients received naloxone by BLS and 69 patients received naloxone by ALS. There was a statistically significant difference in the mean age (P < .01) and race categories (P < .01) between ALS and BLS providers. There was no statistically significant difference in gender (P = .33) or ethnicity (P = .146) between ALS and BLS groups (Table 1).
Table 1. Description of Patient Population (by ALS/BLS Group)

Abbreviations: ALS, Advanced Life Support; BLS, Basic Life Support.
After naloxone administration, BLS patients showed increases in HR (mean baseline HR = 102.69 bpm; mean change in HR = 31.88 bpm; 95% CI, 21.09-42.67; P < .01). There was also a significant change in respiratory status, as BLS patients showed improvements in RR (mean baseline RR = 5.29 breaths/min; mean change in RR = 8.94; 95% CI, 6.96-10.93; P < .01). There were also improvements in spO2 for patients treated by BLS providers (mean baseline spO2 = 73.56%; mean change in spO2 = 23.25%; 95% CI, 13.67-32.83; P < .01).
During the study period, ALS patients similarly showed improvement in RR (mean baseline RR = 10.44 breaths/min; mean change in RR = 9.09 breaths/min; 95% CI, 6.91-11.27; P < .01). The ALS patients also showed improvements in spO2 (mean baseline spO2 = 85.52%; mean change in spO2 = 8.54%; 95% CI, 2.76-14.33; P = .005). There was no significant change in HR for ALS providers (mean baseline HR = 100.32 bpm; mean change in HR = 2.32 bpm; 95% CI, -5.82 to 1.18; P = .189; Table 2).
Table 2. Before and After Naloxone Results for BLS and ALS

Abbreviations: ALS, Advanced Life Support; BLS, Basic Life Support.
A significant difference in arrival time of BLS to the time to naloxone administration between the two groups existed with shorter times in the BLS group compared to the ALS group (1.9 minutes; 95% CI, 1.36-2.58 versus 9.8 minutes; 95% CI, 8.4-11.1, respectively; P < .01). Time from BLS arrival to naloxone administration was 7.8 minutes faster in the BLS group when compared to ALS (95% CI for difference, 6.2-9.3 minutes).
Discussion
This pilot study of BLS administering naloxone for patients with suspected opioid overdose shows similar results to a growing field of knowledge on the subject.Reference Gulec, Lahey, Suozzi, Sholl, MacLean and Wolfson 8 , Reference Weiner, Mitchell, Temin, Langlois and Dyer 9 The BLS providers involved in the study were able to identify patients with opioid overdose, as demonstrated by the significant changes in vital signs after administering the naloxone. The initial vital signs in both the study and control groups demonstrated degrees of hypoxia and bradypnea, consistent with opioid overdose. Both BLS and ALS providers had significant improvements in RRs (change of 8.94 and 9.09, respectively) and spO2 (change of 23.25% and 8.54%, respectively) following intervention. In addition to the response to treatment, this study also demonstrated that patients treated by BLS providers carrying naloxone received the medication in significantly less time than patients treated by BLS providers without naloxone who waited for ALS arrival, an average of 7.8 minutes faster. In most cases, Delaware BLS crews are the first to respond on-scene, so allowing them to carry and administer naloxone could eliminate the time they would have previously needed to wait for ALS to arrive and treat with naloxone.
While more and more states are allowing their BLS agencies to carry and administer naloxone, some hesitancy or concern may exist that these providers may not have adequate training. However, there were no documented adverse effects in any of the patients on the self-reported study forms completed by the prehospital providers, or upon review of the Quality Assurance program files. This study demonstrated a larger change in HR in the pilot group compared to the control group, with the BLS group having more marked tachycardia after intervention. This may represent the difference in training between BLS and ALS, as the increased tachycardia is not necessarily an improvement in vital signs due to the intervention. Other possible explanations for the lack of significant change in HR amongst ALS patients could include more tailored doses of naloxone with other routes of administration, rather than the required 1mg intranasal dose required by BLS. The ALS providers also did not have to follow as stringent inclusion requirements and administration requirements as the providers in the BLS pilot, meaning they may have seen other indications for administration of naloxone rather than frank respiratory distress or decreased responsiveness. This may also explain the smaller change in spO2 demonstrated in the ALS patients compared to BLS patients. In addition, the time of intervention reported was the time of administration of naloxone, rather than arrival of ALS. Therefore, ALS patients may have had a longer time to intervention because they received the medication later in transport, again if the ALS crews perceived an indication less-obvious than impaired mentation or respiration.
While this study was able to demonstrate significant improvement in vital signs following intervention by the BLS pilot program, these changes may have been limited by the geography of the study area. Delaware is the second smallest state in the country, leading to potentially shorter transport times to receiving EDs. In states with more rural area and longer transport and intervention times, there may have been an even larger impact of administration of naloxone. In addition, the arrival times of ALS may be significantly longer, further highlighting the importance of the BLS providers having the ability to intervene with naloxone before waiting for the arrival of ALS. Despite the small size of the state, Delaware has several different geographical variations, including urban, suburban, and rural. Therefore, the results demonstrated in this study would likely be generalizable to other states and areas.
Limitations
Limitations of this study include the small sample size of patients evaluated, 62 in the pilot arm and 69 in the control arm. While significant changes were seen with this sample, larger numbers may have provided more information regarding the intervention. With the two-tiered system, there may have been cross-over in BLS and ALS patients, though this is likely similar to other EMS systems. As the BLS pilot crews were aware of the study they were involved in, this may have caused bias in the intervention they provided, some being more eager to demonstrate their ability to administer naloxone. This could have affected both the administration time and vital sign changes. In a similar sense, the information sheets that the data were pulled from were self-reported. While the vital signs provide objective information, there may have been some bias in the time of administration and when vital signs were recorded. In addition, while providers in the study were able to provide subjective report of adverse events, of which none were reported, a more objective measure of this may have provided more useful information.
Future Studies
This pilot program study evaluated the changes following naloxone administration in opioid overdoses only in the prehospital setting. There was no collection of data following patients’ arrival to the receiving ED. Therefore, it is not possible to evaluate any longer-term outcomes of these patients following BLS or ALS intervention. A future study may better evaluate long-term outcomes if able to track patients through the completion of care of the ED visit, and subsequent disposition. Further studies may also compare outcomes of suspected opioid overdoses following care of BLS crews carrying naloxone versus those not carrying naloxone. While this study showed significant changes in vital signs, it did not evaluate how these vital signs may have changed if naloxone was not administered based on BLS supportive care performed by crews not approved to provide this intervention. A study of this characteristic may add more credence to allowing BLS crews to administer naloxone, or conversely may show no benefit to this intervention.
Conclusion
Following appropriate training and demonstration of knowledge and skills, BLS providers are able to successfully administer naloxone to suspected opioid overdose victims. Patients treated with naloxone by BLS had significant improvements in RRs and spO2, similar to ALS administration. In addition, for patients served by a two-tiered EMS system, such as that utilized by the state of Delaware, the time of administration of naloxone from BLS arrival on-scene was significantly shorter when administered by BLS compared to ALS. Future studies may provide more information regarding long-term outcomes of opioid overdose patients who receive naloxone from BLS providers rather than only allowing ALS providers to administer naloxone.
Acknowledgements
The authors acknowledge the research team of the Department of Emergency Medicine, Christiana Care Health System; the staff of the Delaware Office of Emergency Medical Services, who helped with protocol implementation and data collection; the Delaware State Fire School, who helped with training; and all of the Delaware EMS providers, who helped by caring for and transporting these patients, as well as with data collection.
Conflicts of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.





