The functional outcome after the Fontan procedure for patients with non-correctable CHD is entirely dependent on, first, the adequate size and low vascular resistance of the pulmonary circulation and, second, on the preserved function of the systemic ventricle and the systemic atrioventricular valve.Reference Gewillig and Goldberg 1 Obstruction at any level of pulmonary blood flow constitutes further important resistance to a circulation in series, which is burdened by a chronic low output state. A restrictive atrial septum in Fontan patients with stenosis of any of the systemic atrioventricular valve creates significant obstruction to pulmonary venous return, and thus impacts the overall pulmonary vascular resistance. The diagnosis and management of this rare, but important, lesion has not/rarely been reported in the literature.Reference Nemeh, Reddy, Walters, Hakimi and Ross 2 – Reference Misumi, Hoashi, Kagisaki and Ichikawa 4
Materials and methods
Out of more than 650 patients who underwent Fontan completion between 1988 and 2013, we have identified three patients with a significantly restricted atrial septum at early or late follow-up; two patients presented with early postoperative complications and one with protein-losing enteropathy some 2.5 years after Fontan completion for hypoplastic left heart syndrome. The diagnostic steps and management of these cases are described in this report.
Results
Case 1
A 9-year-old girl with hypoplastic left heart syndrome presented with protein-losing enteropathy 2.5 years after completion of a fenestrated lateral tunnel Fontan. Transthoraic echocardiography documented approximation of the lateral tunnel to the native atrial septum, leaving a slit-like atrial septal defect as the only means for pulmonary venous return. Baseline cardiac catheter documented low pulmonary arterial pressures of 12 mmHg and only a 1 mmHg mean gradient across the atrial septum during catheter pull-back from the left to the right atrium. In order to assess the haemodynamics mimicking physiological stress, she was commenced on Dobutamin infusion up to 20 mcg/kg/minute during pharmacological stress testing to achieve a heart rate of some 160 beats per minute (Fig 1). Repeat measurements revealed a near uniform pressure in the Fontan pathways of 19 mmHg mean, a left atrial pressure of mean 11 mmHg, and a right atrial pressure of 7 mmHg mean – thus, there was a transpulmonary gradient of 8 mmHg added to a trans-septal gradient of 4 mmHg with increased output during stress testing. The patient was referred for surgical conversion to an extra-cardiac Fontan and resection of the atrial septum. She made good recovery and had long-standing resolution from her protein-losing enteropathy.

Figure 1 Catheter pressure pull back across the atrial septum at rest (top panel) and during Dobutamine stress testing at 20 mcg/kg/minute (bottom).
Case 2
A 6.2-year-old girl with double-inlet left ventricle, transposition of the great arteries, and pulmonary stenosis was referred for Fontan completion after previous cavopulmonary shunt. There was mild hypoplasia of the left atrioventricular valve and a small central atrial septal defect. Preoperative haemodynamics were satisfactory and no septectomy was performed. Postoperatively, she suffered from significant low output state and severe prolonged pleural effusions. Ultrasound documented a small atrial communication with turbulence on colour flow mapping and increased inflow velocities across the left atrioventricular valve up to 2.2 m/s peak. Cardiac catheter documented a trans-septal gradient of 5 mmHg mean and Fontan pressures of 18 mmHg mean (Fig 2a). The Fontan fenestration was crossed from the femoral vein and the catheter was passed across the atrial septum to the left pulmonary veins. A Genesis stent (Cordis, Bridgewater, NJ, USA) mounted onto a 16-mm balloon was placed via a 10-Fr-long sheath with good result and abolition of the gradient (Fig 2b). Further, the fenestration was enlarged by a separate short stent. The final Fontan pressure was 15 mmHg and saturations were 89%. She made good recovery and was discharged on day 6 after the procedure. She continues to do well 16 months after the procedure.
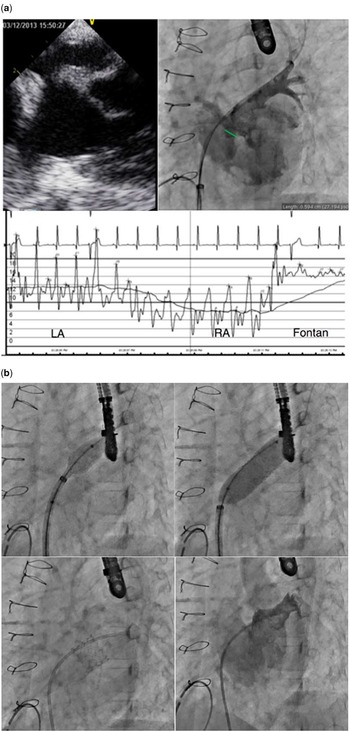
Figure 2 ( a ) Initial trans-oesophageal echo and catheter assessment in patient 2. The echocardiographic and angiographic analyses documented a communication of some 6 mm with a pressure gradient of 5 mmHg mean. ( b ) Sequence of angio still frames during stent placement within the restrictive atrial septum.
Case 3
A 5.6-year-old boy after staged Norwood Fontan palliation for hypoplastic left heart syndrome suffered from severe prolonged effusions 20 days after extra-cardiac Fontan completion. Despite having previously undergone open surgical septostomy, the atrial septal defect only measured 5.8×6.3 mm on biplane trans-oesophageal imaging. Baseline catheter gradient was 4 mmHg mean. He underwent stenting of the atrial septum using a Genesis stent mounted onto a 18-mm balloon delivered through the fenestration; however, the delivery balloon was too long and the stent got partially caught in the fenestration. Despite a wide open atrial septum, he required surgical retrieval with resection of the atrial septum. He made overall good recovery.
Discussion
The Fontan palliation is the accepted treatment for children born with functionally univentricular hearts. The outcome is dependent on an intact pulmonary circulation with low resistance. In cases with a systemic right atrioventricular valve, such as in hypoplastic left heart syndrome or mitral atresia, the pulmonary venous return has to pass through the atrial septum before entering the systemic ventricle. Universally, the atrial septum is excised during the first surgical bypass procedure. Although this is normally effective, the atrial septum can become restrictive over time, either due to re-growth or due to initial inadequate resection. This may not be apparent at the pre-Fontan haemodynamic evaluation, as there is only limited pulmonary blood flow and conversely pulmonary venous return in the setting of only a superior cavopulmonary shunt – typically only 50%. Re-directing the inferior caval venous return to the pulmonary circulation at the time of Fontan completion may unmask such restriction. Observed pressure gradients across the atrial septum at baseline haemodynamic study under general anaesthesia are normally very low. In some cases, it may be warranted to repeat haemodynamic assessment with pharmacological stress testing.
In the setting of early or late post-Fontan problems, it is warranted to address restriction of the atrial septum in these patients either by interventional cardiac catheter techniques or surgical Fontan revision with resection of the atrial septum. Redo Fontan surgery carries significant mortality and morbidity.Reference Petko, Myung and Wernovsky 5 Transcatheter stenting of the atrial septum is an established technique in the hybrid treatment of hypoplastic left heart syndrome or after cavopulmonary shunt.Reference Schranz, Bauer and Reich 6 , Reference Moszura, Dryżek and Góreczny 7 It has not been previously reported after Fontan completion. It is important to use short delivery balloons so as to allow placement of the large diameter stent within the confined atrial chambers.
Acknowledgements
None.
Financial Support
Dr D. Quandt was supported by a research grant by the “Kinderspital Zürich – Eleonorenstiftung” and “EMDO Stiftung”, Switzerland.
Conflicts of Interest
None.





