Introduction
Rosenberg (Reference Rosenberg1965) defined self-esteem as an individual’s positive attitudes towards oneself. Self-esteem is considered a common factor in many mental health problems, including depression (Orth et al., Reference Orth, Robins and Roberts2008), anxiety (Greenberg et al., Reference Greenberg, Solomon, Pyszczynski, Rosenblatt, Burling, Lyon, Simon and Pinel1992) and eating disorders (Noordenbos et al., Reference Noordenbos, Aliakbari and Campbell2014). Some have argued that self-esteem plays a causal role in the development of mental health problems. This is exemplified by the vulnerability model (Orth et al., Reference Orth, Robins and Roberts2008), which posits that low self-esteem contributes to depression by increasing negative thoughts about oneself. Others have suggested that self-esteem can have a buffering effect in protecting against anxiety, as demonstrated in laboratory experiments (Greenberg et al., Reference Greenberg, Solomon, Pyszczynski, Rosenblatt, Burling, Lyon, Simon and Pinel1992). Despite its potentially important contributions to a variety of clinical psychological presentations, self-esteem has only recently been taken as a valid target for clinical psychological intervention.
A cognitive behavioural therapy (CBT) intervention for low self-esteem has been developed by Fennell (Reference Fennell1999). Fennell’s model includes a longitudinal formulation of low self-esteem stemming from early experiences which result in negative core beliefs about the self. These core beliefs dictate ‘rules for living’, such as ‘If I try, I will fail’. These rules are called into action during everyday life when there is a risk that they might be broken, for instance when being required to give a presentation at work. When this happens, it can result in anxiety, as core beliefs lead to both anxious predictions about what will happen and unhelpful behaviours, such as avoidance or safety behaviours, which can maintain anxiety. These feelings and behaviours can lead to further self-critical thoughts, low mood, and ultimately, further confirmation of negative core beliefs. Alternatively, if someone experiences a threat to their self-concept, such as criticism at work, then their negative core beliefs are directly confirmed, leading to self-criticism, low mood and further reinforcement of negative core beliefs.
Evidence is accumulating that Fennell’s (Reference Fennell1999) self-esteem programme is associated with increases in self-esteem. A recent meta-analysis by Kolubinski et al. (Reference Kolubinski, Frings, Nikčević, Lawrence and Spada2018) found that this intervention resulted in improvements in self-esteem and depression when delivered using weekly group or individual sessions, with large effect sizes. Shorter, one-off interventions based on the same model also seemed to improve both self-esteem and depression, even months later (Horrell et al., Reference Horrell, Goldsmith, Tylee, Schmidt, Murphy, Bonin, Beecham, Kelly, Raikundalia and Brown2014). In a randomised control trial, Waite et al. (Reference Waite, McManus and Shafran2012) found that Fennell’s CBT programme resulted in improvements in self-esteem which were significantly better than a waiting list control group. The programme is sometimes delivered in a group therapy format, and improvements have also been shown in this context. Rigby and Waite (Reference Rigby and Waite2006) used the Fennell (Reference Fennell1999) protocol in the context of a group intervention and found improvements in self-esteem from the beginning to the end of the group. In addition, there have been previous evaluations of the NHS Fife ‘Overcoming Low Self-Esteem’ group, which is the focus of the current paper, that have demonstrated statistically significant increases in self-esteem from the beginning to the end of the group (Doughty, Reference Doughty2015; Morton et al., Reference Morton, Roach, Reid and Stewart2012), including a controlled trial (McElhinney et al., Reference McElhinney, Reid and Morton2016).
However, critical reflection on this evidence base suggests that there is scope for building upon these evaluations to inform the design of future group-based instantiations of this programme. Firstly, there is currently limited evidence from follow-up data collection that improvements in self-esteem continue over time, after the intervention has ended, when individuals may be returning to an environment in which they have a long history of negative self-attributions and difficult interpersonal relationships. In the current study, we assess self-esteem, depression and anxiety 3 months after the intervention ended, to give participants time to confront any challenges within their everyday lives using the techniques recommended by the Fennell (Reference Fennell1999) protocol. Three-month follow-up data from interventions based on Fennell’s (Reference Fennell1999) protocol is available, but only from single-day, one-off interventions (Kolubinski et al., Reference Kolubinski, Frings, Nikčević, Lawrence and Spada2018). Follow-up data from longer-term group interventions based on the model seem to be less common.
This evaluation aims to address the above issues by analysing data from the National Health Service in Fife, Scotland, UK. The psychology service in Fife has been running an ‘Overcoming Low Self-Esteem’ group based on Fennell’s (Reference Fennell1999) programme for several years. The data from this group will be used to determine whether improvements in self-esteem, depression, and anxiety persist after the Overcoming Low Self-Esteem group is completed.
Method
Participants
Participants were 229 individuals who were registered to attend the Overcoming Low-Self Esteem course in the Psychology Department, NHS Fife, between October 2011 and January 2019. Participants were women (83.8%) and men (15.7%) referred to the department for a broad range of psychological concerns. Average age was 40.9 years old (standard deviation 12.6). Participants were referred during or after a period of therapy with a clinician in the department or following an initial assessment with a clinician who then referred the participant to the group as a first line of treatment. Participants were deemed to have ‘dropped out’ from the group if they missed three or more of eight sessions; in total, 27.2% of participants dropped out of the group. Participants who dropped out of the group did not differ from those who remained in terms of age (t 223 = 0.46, n.s.), social deprivation (t 222 = 0.75, n.s.), or gender (χ2 (1, n = 227) = 2.27, n.s.). However, participants who dropped out reported significantly higher levels of depression (t 221 = –2.90, p = 0.004); mean depression scores were 32.3 (SD 11.2) for those who stayed in and 37.2 (SD 11.4) for those who dropped out. Anxiety scores also differed between the two groups at baseline (t 223 = –2.64, p = 0.009); mean anxiety scores were 24.5 (SD 12.0) for those who stayed in the group and 29.3 (SD 12.7) for those who dropped out of the group. For self-esteem, there was a trend towards a significant result indicating lower levels of self-esteem at baseline among those who dropped out, although this did not reach significance (t 222 = 1.91, p = 0.057). Mean self-esteem scores were 82.2 (SD 23.8) for those who stayed in the intervention and 75.4 (SD 22.2) for those who dropped out.
Intervention
The Overcoming Low Self-Esteem intervention is delivered as a group-based adaption of Fennell’s (Reference Fennell1999) self-help workbooks. Groups were run with a minimum of two and a maximum of 13 participants, with an average of nine participants. Only one group had two participants out of a total of 26 groups included in this study. All other groups included at least four participants, with a mode of 11 and a mean of 9.2 participants. Groups took place in community venues around Fife, a region of Scotland. The group was run over eight sessions, with a ninth follow-up session held 3 months later. Sessions were organised broadly around the sequential chapters of the workbooks. Material was presented in each session alongside group discussions and individual exercises. The group was initially run as a women-only group based on the view that women would be more open and able to disclose stories of abuse in a single-gender group (Morton et al., Reference Morton, Roach, Reid and Stewart2012). However, it has recently been changed into a mixed-gender group.
Measures
At the first group, last group and follow-up session, participants were administered the Robson Self-Concept Questionnaire (RSCQ; Robson, Reference Robson1989), the Beck Anxiety Inventory (BAI; Beck and Steer, Reference Beck and Steer1993), and the Beck Depression Inventory (BDI; Beck et al., Reference Beck, Steer and Brown1996). We attempted to collect follow-up via post at 2 and 6 months, but the return rate was very low, so we scheduled follow-up sessions where participants could fill out questionnaires. The follow-up session was held at 3 months as longer latencies might have resulted in a greater number of participants being lost to follow-up. The RSCQ is a 30-item self-report questionnaire measuring self-esteem; it has demonstrated good reliability, convergent validity and discriminant validity (Robson, Reference Robson1989). The BDI is a widely used self-report measure of depression demonstrating good psychometric properties across a number of indicators (e.g. Wang and Gorenstein, Reference Wang and Gorenstein2013). Likewise, the BAI is a well-known instrument assessing anxiety and demonstrating good psychometric properties (e.g. Osman et al., Reference Osman, Kopper, Barrios, Osman and Wade1997).
Design
This study utilised an observational within-subjects design, with participants completing three sequential sets of measures (pre-group measures at the first session, post-group measures at the last session, and follow-up group measures at a follow-up 3 months later).
Data analyses
Analyses were conducted in IBM SPSS Statistics version 24. Differences between pre-, post- and follow-up scores were assessed using a repeated measures ANOVA. We used an intention-to-treat design whereby participants’ initial scores were imputed when subsequent questionnaires were missing, normally due to participant drop-out. We also calculated descriptive statistics, as reported below. Clinical significance was investigated by calculating a cut-off score for ‘recovery’ as per the recommendations of Jacobson and Truax (Reference Jacobson and Truax1991), and calculating how many participants improved without recovering, recovered, stayed the same, or deteriorated.
Sample size required for the main analysis of variance analysis was calculated using G*Power (Faul et al., Reference Faul, Erdfelder, Lang and Buchner2007). Sample size calculations were based on the primary aim of the study, which was to investigate whether there were differences between the first session, the last session, and the follow-up session in terms of psychological outcomes. A medium effect size was expected based on previous research on the group (Doughty, Reference Doughty2015). Alpha was set to 0.05 and desired power to 80%. A standard 0.50 correlation between each of the three measurements was stipulated. Sample size analyses were based on the data meeting the assumption of sphericity. Using a one-way repeated-measures ANOVA design, we calculated that a sample size of 28 participants completing each measure was required for an 80% chance that a true effect would be detected. Therefore, the analyses were sufficiently powered to detect an effect.
Results
Descriptive statistics
The means and standard deviations for each variable of interest, alongside the number of people completing pre-, post- and follow-up group measures, are shown in Table 1.
Table 1. Means and standard deviations of pre-, post- and follow-up self-esteem, depression and anxiety
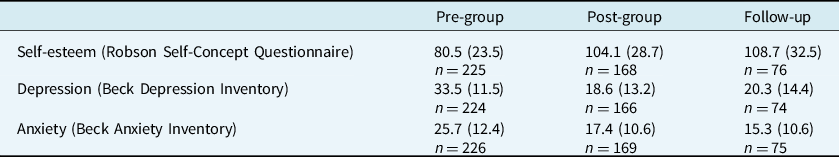
Results are displayed as means (SD).
Comparing those who completed follow-up measures with those who did not, as Table 1 shows, fewer participants completed follow-up measures than completed pre-group or post-group measures. We conducted analyses to determine whether participants completing follow-up measures differed from those who did not complete follow-up measures. Participants who completed follow-up measures did not differ from those who did not in terms of age (t 224 = –1.37, n.s.), social deprivation (t 222 = –0.34, n.s.), baseline self-esteem (t 223 = –0.65, n.s.) or baseline depression (t 222 = 1.64, n.s.). However, women were less likely to complete follow-up questionnaires than men (χ2 (1, n = 228) = 3.98, p = 0.046). In addition, those who completed the follow-up questionnaires had lower baseline anxiety scores than those who did not complete measures (t 224 = 2.66, p = 0.009).
Main analyses
Pre-, post- and follow-up differences in self-esteem, anxiety and depression scores were assessed using a repeated measures ANOVA using an intention-to-treat design. For all three variables, test assumptions were met apart from the assumption of sphericity; therefore, the Greenhouse–Geiser correction for violations of sphericity was used. There was a statistically significant effect of time on self-esteem, F 1.4,221 = 84.5, p < 0.001; depression, F 1.3,219 = 134.3, p < 0.001; and anxiety, F 1.1,222 = 75.5, p < 0.001. The corresponding effect sizes, partial eta squared, for these analyses were all large or medium-to-large: for self-esteem, η2 = 0.28; for depression, η2 = 0.38; and for anxiety, η2 = 0.25. Figure 1 depicts these changes in scores over time.
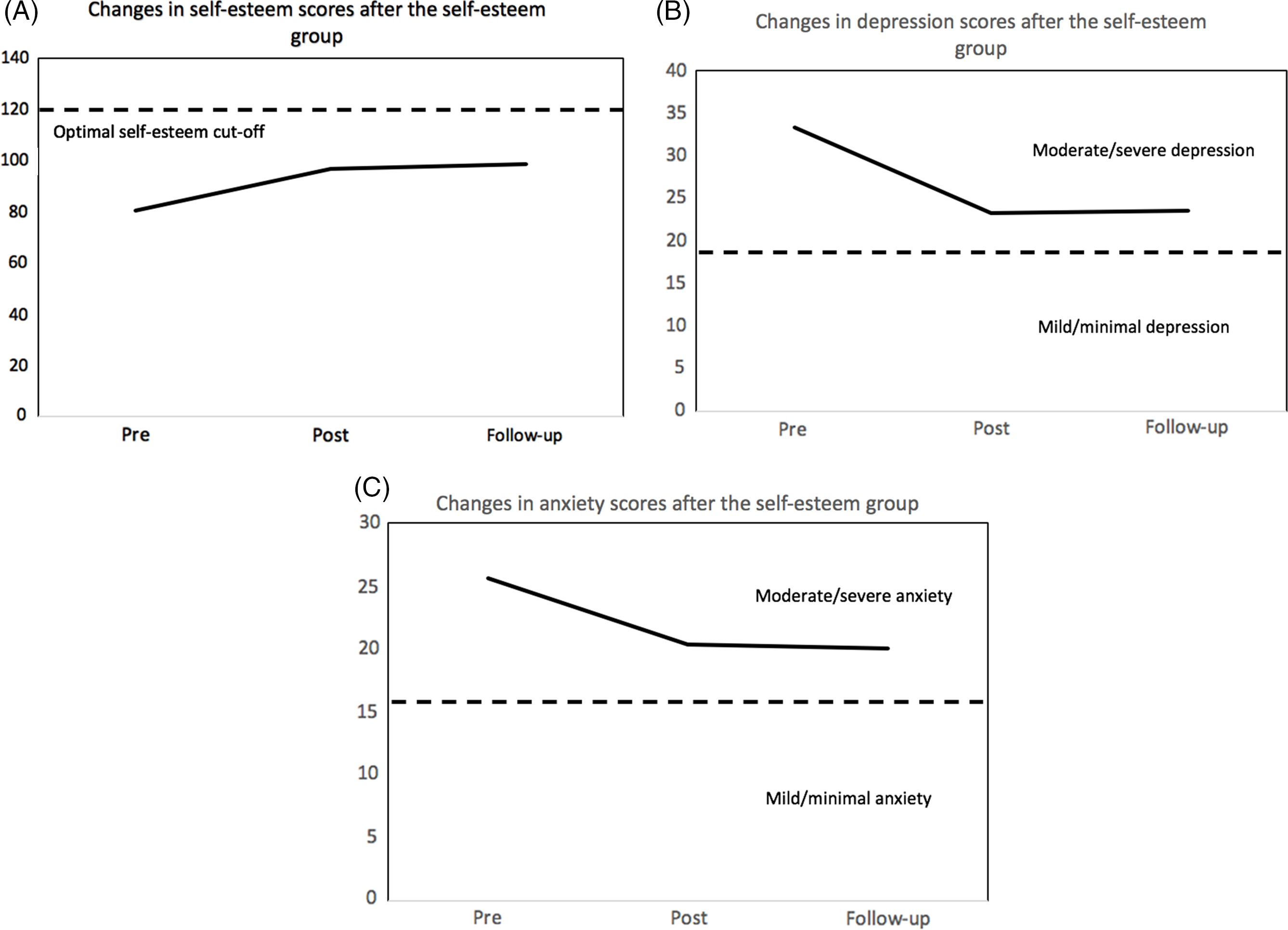
Figure 1. Changes in average self-esteem scores (A), depression scores (B) and anxiety scores (C) from the beginning (‘pre’) to the end (‘post’) and follow-up of the Overcoming Low Self-Esteem group.
Post-hoc pairwise comparisons using a Bonferroni correction indicated that, for all three variables, pre-group scores differed significantly from post-group scores (p < 0.001 for self-esteem, depression and anxiety) and follow-up scores (p < 0.001 for self-esteem, depression and anxiety), but there was no significant difference between post-group and follow-up scores. As these analyses suggest, all indicators seem to improve from the beginning of the group to a follow-up session 3 months after the group has ended.
Clinical significance
According to Jacobson and Truax (Reference Jacobson and Truax1991), one method for investigating clinical significance is by calculating a cut-off point past which participants might be said to have recovered from problems with self-esteem, depression or anxiety. The authors present several methods for calculating this cut-off; we chose to use their calculation ‘a’. Using calculation a, Jacobson and Truax (Reference Jacobson and Truax1991) suggest that participants improving by two standard deviations from the mean pre-group score might be said to have recovered following treatment.
For self-esteem, the pre-group mean was 80.5 with a standard deviation of 23.5. Therefore, participants scoring higher than 127.5 might be said to have recovered from low self-esteem. For depression, the pre-group mean was 33.5 with a standard deviation of 11.5, meaning that participants scoring 10.5 or lower at follow-up might be said to have recovered. For anxiety, the pre-group mean was 25.7, with a standard deviation of 12.4, meaning that only participants scoring less than 1 might be said to have recovered. Table 2 summarises the number of participants who recovered, improved without recovering, stayed the same, and deteriorated at follow-up. Please note that deteriorations were often small, potentially reflecting variations in scoring due to test–re-test reliability issues.
Table 2. Number of participants falling into different categories of change on self-esteem, anxiety and depression at follow-up
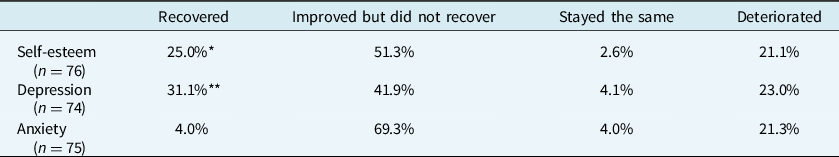
*One participant counted in this cell had a self-esteem score higher than the cut-off for recovery before the intervention.
**Two participants counted in this cell had depression scores below the cut-off for recovery before the intervention.
Discussion
Main findings
This evaluation builds on prior research demonstrating improvements in self-esteem following the use of Fennell’s (Reference Fennell1999) cognitive behavioural therapy programme for low self-esteem. From the findings above, it seems that improvements in self-esteem persist past the end of the group. Similarly, improvements in anxiety and depression seem to be maintained after the group has finished. These changes are statistically significant and are accompanied by large effect sizes. However, it should be noted that average scores after the group did not fall into the optimal range for either self-esteem, depression or anxiety, despite moving in a favourable direction.
Our clinical significance calculations demonstrated that a majority of participants completing the 3-month follow-up questionnaires improved on all three measures (self-esteem, depression and anxiety) from baseline. Of those who improved, a smaller number could be said to have fully ‘recovered’, according to Jacobson and Truax’s (Reference Jacobson and Truax1991) criterion, and some participants deteriorated to some extent from the beginning of the group to the 3month follow-up. Jacobson and Truax (Reference Jacobson and Truax1991) acknowledge that clinical significance calculations can sometimes reflect on an intervention less favourably than statistical significance. Furthermore, these calculations might be considered quite conservative. For instance, according to our calculations, participants needed to score less than 1 on the BAI in order to be said to have fully recovered. However, the BAI includes several questions about physical symptoms that might be present to some degree in those without substantial anxiety. Therefore, a cut-off of 1 is an extremely stringent criterion for recovery, requiring essentially no symptoms. A less stringent measure may have been calculating the number of people falling into the clinical and non-clinical ranges for each measure.
While this calculation is helpful in determining the extent to which participants improved using an objective criterion for recovery, there is also an argument to be made that full remission from mental health problems is difficult to define in operationalized terms. Furthermore, elimination of symptoms may not always be a realistic outcome of intervention; rather, a long-term management model of mental health might advocate understanding one’s symptoms and developing strategies to cope with symptoms that enable improved functioning or quality of life.
Our results also demonstrate that the group seems to be targeted to the right population; 95.1% of participants completing measures at the beginning of the group gave scores falling within the ‘low self-esteem’ range on the RSCQ. At the follow-up session, 68.4% reported low self-esteem, which might be considered a small improvement. It is possible that self-esteem might continue to increase after the group as techniques are introduced and practised in everyday life, although this study did not incorporate a long-term follow-up. Furthermore, for those with difficult early life experiences causing low self-esteem, the problem may be pernicious and difficult to shift in a short time frame. In these terms, the decrease in the number reporting low self-esteem following the group might be considered meaningful.
Implications of these findings
These results suggest that a time-limited group intervention targeting self-esteem based on the Fennell (Reference Fennell1999) model is associated with improvements in self-esteem, depression and anxiety at a 3-month follow-up. Concurrent improvements in self-esteem and depression are perhaps unsurprising, given there is some suggestion that CBT-based interventions for self-esteem and depression might overlap, and given the evidence that self-esteem and depression both improve following interventions based on the Fennell model (Kolubinski et al., Reference Kolubinski, Frings, Nikčević, Lawrence and Spada2018). However, our study cannot provide direct support for the ‘vulnerability’ model, as discussed in the Introduction, which suggests that low self-esteem causes depression by increasing negative thoughts about oneself (Orth et al., Reference Orth, Robins and Roberts2008), because our study could not determine causal links between depression and self-esteem.
The impact of Fennell’s (Reference Fennell1999) model on anxiety seems to be less well-researched; it was not an outcome of interest in the meta-analysis of Kolubinski et al. (Reference Kolubinski, Frings, Nikčević, Lawrence and Spada2018). In our study, we found that improvements in anxiety seem to be sustained following a group intervention for self-esteem. However, the link between self-esteem and anxiety in our sample is not clear. It is unclear, for instance, whether self-esteem buffers against anxiety, a possibility discussed in the Introduction, as our study was not designed to evaluate such causal claims.
More broadly, our study has implications for conceptualisations of ‘self-esteem’, a concept that has gone through several transformations in the history of psychology. Rosenberg (Reference Rosenberg1965), writing in the mid-1960s, borrowed his ideas from the literature on public relations (PR). His insight was that individuals might take a PR approach to their view of themselves, in much the same way that individuals might have a positive or negative view of a brand. He wrote that ‘there is no qualitative difference in the characteristics of attitudes towards the self and attitudes towards soup, soap, cereal, or suburbia’ (p. 6).
However, there are several complications to this conceptualisation of self-esteem. In light of more contemporary ideas of power and identity politics, which might suggest that members of disenfranchised groups within society are made to feel negatively about themselves, this PR perspective seems somewhat dated and simplistic. Furthermore, developments in the Social Identity Approach might suggest that self-image is a multi-faceted construct based on currently active group affiliations, such as ‘millennial’, ‘woman’ or ‘working class’ (Ellemers, Reference Ellemers2012). This picture is further complicated by research on trauma, which suggests that negative life experiences, particularly those early in life, might impact on core beliefs or schemas about the self (Dutra et al., Reference Dutra, Callahan, Forman, Mendelsohn and Herman2008). While Rosenberg might have seen self-esteem as a problem of personal brand image, a manipulable view of oneself that can be improved through the right PR campaign, this term seems to have become more multi-dimensional over time, incorporating, for instance, an internalisation of society’s views of one’s class, gender or race, and an internal assimilation of life events that may leave lasting imprints on one’s view of oneself. The findings of the current intervention suggest that a multi-faceted conceptualisation of self-esteem based on one’s life events, current maintaining factors and personality, such as Fennell’s (Reference Fennell1999) model, may be more helpful in therapeutic work than a conceptualisation based on a ‘PR’ approach, which might instead suggest simply bolstering positive views of oneself.
There are also those who argue that self-esteem is an unhelpful goal. Neff and Vonk (Reference Neff and Vonk2009) argue that what we call self-esteem can fluctuate greatly from moment to moment, contingent on environmental circumstances, and that the quest for positive self-evaluation is, at worst, a futile endeavour, and at best, an exercise in narcissism. She argues that self-compassion, which incorporates ‘self-kindness’, a sense of common humanity in suffering, and mindful acceptance of difficulty (Neff, Reference Neff2003), is more beneficial than high self-esteem. Some aspects of Fennell’s (Reference Fennell1999) programme relate only to self-esteem (for instance, keeping a positive qualities diary) but, in some areas, there may be conceptual overlap between the target of her intervention and self-compassion. Still other aspects of self-compassion, such as a sense of commonality with others experiencing difficulty, are not explicitly represented in Fennell’s programme. Yet informal feedback from group members indicated that connecting with others in the group was helpful, supporting the notion that connection with others and views of oneself are linked.
Limitations
Participants were not randomised to treatment groups in this study; therefore, it is not possible to make causal claims about the link between the programme and the improvements in self-esteem, anxiety and depression. A controlled trial has already been conducted on this programme (McElhinney et al., Reference McElhinney, Reid and Morton2016), but a randomised design would provide further evidence that changes are attributable specifically to the programme. Furthermore, it is important to recognise that these results are based on self-report data. It is possible that individuals might misrepresent their improvements, either consciously (i.e. exaggerating to thank the facilitators for their input) or unconsciously (i.e. unintentionally describing their hopes for improvement rather than their actual improvement).
In addition, participants belonged to their intervention groups, and the analyses above do not take into account the dynamics of the particular group that they were in. It is possible, for instance, that larger groups or smaller groups were more beneficial for participants. A multi-level modelling approach might have allowed us to investigate this, but our sample size was too small for such an analysis. In addition, due to attrition, the number of people from each group would be very small, and this would potentially over-represent responders, who tended to have better psychological measures at baseline. However, future studies might take the group structure into account when conducting such analyses.
Our analyses demonstrated that participants who dropped out tended to have higher depression and anxiety at baseline. It is possible that psychological variables associated with poorer mental health, such as low self-efficacy and feelings of hopelessness, might have deterred participants from completing the group. It is also possible that people who dropped out might have had a significant trauma history that might have worsened their mental health. Participants with higher anxiety at baseline were less likely to complete follow-up measures; this may reflect a similar process whereby those with more severe mental health problems might engage less with the group and with the evaluation. This suggests that the group may be most effective for those with mild to moderate concerns regarding self-esteem, while those presenting with more severe and enduring difficulties might benefit from more intensive interventions.
It is also worth mentioning that several participants fell into the optimal self-esteem group at the beginning of the intervention. This might suggest that these participants were referred to this group in error, or that these participants tended towards optimism in their self-assessments. It may have been useful to conduct analyses with this subgroup excluded, given the intervention was not targeted towards these participants. However, these participants also seemed to benefit from the group in terms of their self-esteem, suggesting that their improvements were on par with those experienced by the rest of the sample.
Conclusion
The results of this study demonstrate that improvements in self-esteem, depression, and anxiety following a group intervention based on Fennell’s ‘Overcoming Low Self-Esteem’ protocol can persist after the intervention has finished. This suggests that a CBT-based intervention can be helpful for self-esteem as well as other common mental health problems. However, further research from randomised controlled trials would help to provide causal evidence for improvements.
Acknowledgements
Thanks to Tara Graham for her research governance support.
Financial support
No financial support was required for this project.
Conflicts of interest
The authors have no conflicts of interest with respect to this publication.
Ethical statements
While conducting this evaluation, all authors abided by the Ethical Principles of Psychologists and Code of Conduct as set out by the BABCP and BPS. Ethical approval was granted from the University of Edinburgh Clinical Psychology Research Ethics team, reference number CLIN633.
Data availability
The data that support the findings of this study are considered confidential according to National Health Service policy and therefore are not shared publicly. Anyone interested in accessing the data should contact the corresponding author (S.S.).






Comments
No Comments have been published for this article.