Introduction
Contraceptive use is of continuing scientific interest for its contribution to reducing fertility and improving maternal and child health in India. Contraceptive prevalence and demand for family planning remain highly diverse among the Indian states (New et al., Reference New, Cahill, Stover, Gupta and Alkema2017), despite the implementation of various family planning programmes since the 1950s aimed at increasing contraceptive use (Srikantan & Balasubramanian, Reference Srikantan and Balasubramanian1983; Santhya, Reference Santhya2003). The enactment of the Reproductive and Child Health Programme in 1996 and the National Population Policy of 2000 affirmed the Indian government’s promises on the delivery of quality services, information and counselling, and expanding the contraceptive method ‘basket’ to enable people to make voluntary and informed contraceptive choices (Santhya, Reference Santhya2003). India’s Vision FP2020 document recommends focusing on ensuring the quality of services to achieve its target of reaching 48 million additional women with modern contraceptive methods by 2020 (Government of India, 2014). However, the quality of family planning services has often been reported to be far from satisfactory (Mavalankar & Sharma, Reference Mavalankar, Sharma, Koenig and Khan1999; Srinivasan, Reference Srinivasan2006), and has been questioned for failing to address the ethical issues associated with the programme at large (Pradhan & Ram, Reference Pradhan and Ram2009). Women have the right to receive complete information on family planning and to make their own decisions, and informed choice is considered a fundamental human right (Huezo & Diaz, Reference Huezo and Diaz1993). Informed choice increases women’s confidence and commitment to contraceptive use. Moreover, counselling women appropriately with instructions they can understand ensures their right to information and reproductive self-determination (Hardee et al., Reference Hardee, Kumar, Newman, Bakamjian, Harris, Rodriguez and Brown2014).
Young Indian women and, more specifically, those socioeconomically weak, usually have little autonomy within and outside the household and have limited control over their own reproductive and contraceptive choices (Jejeebhoy, Reference Jejeebhoy1995; Moursund & Kravdal, Reference Moursund and Kravdal2003; Ravindran & Balasubramanian, Reference Ravindran and Balasubramanian2004). Prevalent norms on childbearing, particularly son preference, further compel young married women to surrender to the expectations of their husbands and in-laws, irrespective of economic status (Clark, Reference Clark2000; Pande & Malhotra, Reference Pande and Malhotra2006). Hence, assessing informed choice in specific modern contraceptive method acceptance among young married women is pertinent in the broader context of individual freedom and reproductive rights. Although prone to measurement error, and perhaps differing from the provider’s perspective (Petersen, Reference Petersen1988), the client’s perspective is useful for service providers and programmers to understand user’s perception of service quality (Andaleeb, Reference Andaleeb2001).
The Method Information Index (MII) has been adopted as a core indicator of informed choice by the Family Planning 2020 (FP2020) initiative, and is increasingly used as an indicator to address the concepts of counselling, informed choice and process quality (Jain, Reference Jain2017; Chang et al., Reference Chang, Mukanu, Bellows, Hameed, Kalamar and Grépin2019). This study asked: (a) whether young Indian married women’s acceptance of modern contraceptive methods are informed choices, and (b) what the enablers and barriers to informed choice are among young married women in India.
Methods
Study sample
The study used data from the fourth round of the Indian National Family Health Survey (NFHS-4) 2015–16. Currently married women aged 15–24 using any modern contraception at the time of the survey were included in the study sample (N = 20,752). The NFHS is a nationally representative household survey that provides data for a wide range of monitoring and impact evaluation indicators in the areas of population and health. It is a stratified two-stage sample with an overall response rate of 98%. Only those respondents who voluntarily consented to participate in the survey were included.
Outcome variables
The outcome variables included in the analysis were: (1) told about other available family planning methods before adopting any of the selected modern methods (female sterilization, oral contraceptive pill or intrauterine device (IUD)) by any person, including health/family planning worker; (2) informed about the side-effects when starting using the modern method; and (3) told about the procedure to manage side-effects when starting using the modern method by any person, including health/family planning worker. The analysis excluded condom use because information about its side-effects and side-effect management was not available in the survey. Moreover, the condom has few side-effects for women and is known to be procured commercially with hardly any scope for counselling. A detailed analysis of the injectable was not carried out because of the very small number of users. Furthermore, the MII was calculated and used separately for female sterilization, the oral contraceptive pill and IUD, and a combined MII also calculated that included female sterilization, the oral contraceptive pill, IUD and injectables. The MII was calculated from the percentage of users who responded ‘yes’ to all three questions about: whether they were informed about methods other than the one they received, were told about method-specific side-effects and were advised what to do if they experienced side-effects.
Predictor variables
The predictor variables used in the analysis were source of method (government/private sector), women’s age (15–19/20–24), years of schooling (no schooling, <10 years, 10+ years), number of living child (none, at least one), exposure to family planning messages (TV/radio/newspapers/wall paintings) (no, yes), religion(Hindu, other), social group (scheduled caste (SC), scheduled tribe (ST), other backward class (OBC), other), number of household members (<5, 5+), wealth quintile (poorest, poorer, middle, richer, richest), type of place of residence (urban, rural), and region (North, Central, East/ North-East, West, South). Number of living children as a predictor variable was not included in the analysis for female sterilization as there were only five sterilized women without any children. The source of method as a predictor variable was not included in the analysis for the oral contraceptive pill because a substantial proportion of pill users had obtained their last supply from a commercial outlet with little scope for counselling. Additionally, the survey has no information about the initial supply for oral contraceptive pill users. Previous literature supports all the predictor variables included in the analyses as key determinants of contraceptive use in the Indian setting (Balaiah et al., Reference Balaiah, Naik, Ghule and Tapase2005; Stephenson, Reference Stephenson2006; Sharma et al., Reference Sharma, Mohan, Das and Awasthi2012; Ram et al., Reference Ram, Shekhar and Chowdhury2014; Pandey & Singh, Reference Pandey and Singh2015; Thulaseedharan, Reference Thulaseedharan2018).
Statistical analysis
Descriptive statistics and bivariate analyses were carried out to understand the socioeconomic and demographic differentials in women 1) being informed about contraceptive methods other than the one they received, 2) being told about method-specific side-effects and 3) being advised about possible side-effects management. Binary logistic regression was carried out to examine the adjusted effect of factors associated with the MIIs for female sterilization, oral contraceptive pill and IUD, and the combined MII. Sample weights were used to adjust for non-response. STATA Version 15 was used for analyses, and a level of significance of p < 0.05 applied.
Results
Levels of modern contraceptive use among young women
Twenty-one per cent of the sample women were using a form of modern contraceptive method (Fig. 1): 8% for limiting and 13% for spacing. Of these, 36% were sterilized, 30% used condoms, 25% used the oral contraceptive pill, 7% the IUD and the rest used another method (Fig. 2).

Figure 1. Contraceptive methods used by currently married women aged 15–24, India, 2015–16.
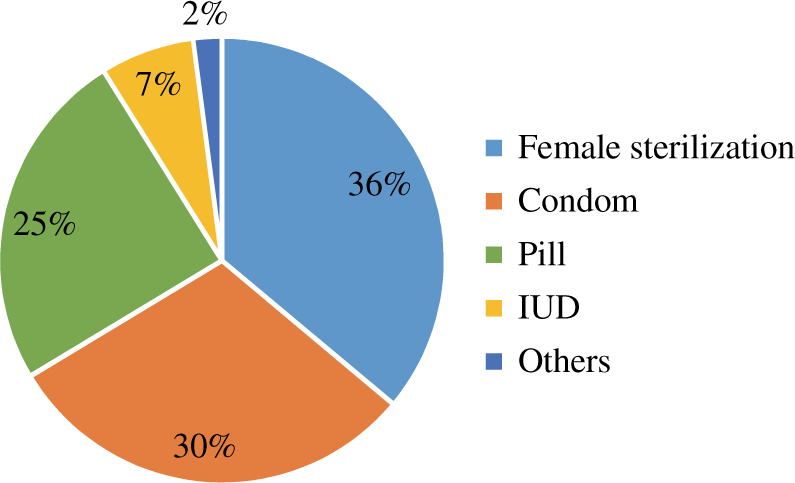
Figure 2. Percentage distribution of modern contraceptive method use by currently married women age 15–24, India, 2015–16.
Level of informed choice of modern contraceptive users
Female sterilization acceptors
Nearly half (49%) of female sterilization acceptors were told about other possible methods of contraception; about two-fifths (41%) were told about its side-effects, and of these, 87% were told about side-effect management (Table 1). Only 29% of sterilized women had information about all three of the above indicators, and level of communication varied considerably by women’s socioeconomic and demographic characteristics. Better education status increased the chances of receiving method information. For example, women with any schooling (OR: 1.25, CI 1.08–1.45) and 10 or more years of schooling (OR: 1.42, CI 1.19–1.69) had higher odds of receiving method information compared with those without any schooling. Economic status was also found to be an enabler, with women in the richer (OR: 1.24, CI 1.01–1.53) and richest quintiles (OR: 1.59, CI 1.21–2.09) having higher chances of method information as against their counterparts in the poorest quintile. Women with exposure to FP messages (OR: 1.30, CI 1.09–1.55) were more likely to be informed about the method compared with those without any exposure. Women from households with five or more members (OR:0.85, CI 0.76–0.94), those of non-Hindu religions (OR:0.78, CI 0.66–0.92) and those residing in rural areas (OR:0.73 CI 0.64–0.83) were significantly less likely to be informed about the method than their respective counterparts. Sterilized women from the West (OR: 0.49, CI 0.39–0.63), South (OR: 0.76, CI 0.63–0.93) and Central regions (OR: 0.82, CI 0.65–1.03) had lower chances of being informed about the method than their northern counterparts. Women availing sterilization from a private health facility were less likely to be informed about the method compared with those who underwent the procedure in a public health facility (OR: 0.86, CI 0.75–0.98).
Table 1. Percentage of female sterilization acceptors told about other methods, side-effects and side-effect management, and Method Information Index (MII), India, 2015–16

*p < 0.10; **p < 0.05; ***p < 0.01.
Oral contraceptive pill acceptors
Of the oral contraceptive pill users, 65% were told about other possible methods of contraception; 54% were told about its side-effects, and of these, 86% were told about side-effect management (Table 2). Forty-two per cent of oral contraceptive pill users were informed about all three of the above indicators. Women with exposure to FP messages (OR: 1.31, CI 1.11–1.55), those of non-Hindu religions (OR:1.40, CI 1.22–1.61) and those in the richest quintile households (OR: 1.36, CI 0.99–1.87) were significantly more likely to be informed about the method as against their respective counterparts. The likelihood of receiving method information was higher among those in the SC (OR: 1.93, CI 1.65–2.27), ST (OR: 1.65, CI 1.33–2.04) and OBC (OR: 1.68, CI 1.44–1.97) categories than those from the ‘other’ category. Users from the East region (OR: 1.38, CI 1.06–1.80) and the South region (OR: 2.52, CI 1.46–4.35) had higher chances of receiving method information compared with their counterparts from the North.
Table 2. Percentage of oral contraceptive pill acceptors told about other methods, side-effects and side-effect management, and Method Information Index (MII), India, 2015–16

*p < 0.10; **p < 0.05; ***p < 0.01.
IUD acceptors
Half of IUD users were informed about other available methods of contraception, possible side-effects and side-effect management (Table 3). Separately, 71% were told about other available methods of contraception; 66% were told about IUD side-effects, and of those, 87% were informed about side-effect management. IUD users exposed to FP messages were two times more likely to be informed about the method than those without exposure to such messages (OR: 2.08, CI 1.36–3.15). Users aged 20–24 had higher chances of receiving method information than those aged 15–19 years (OR: 1.50, CI 0.95–2.36). The chances of IUD users being informed about the method were higher among acceptors following non-Hindu religions (OR: 1.32, CI 0.98–1.77) and those residing in rural areas (OR: 1.67, CI 1.30–2.13). Users from the West region (OR: 0.46, CI 0.31–0.68) and the North-eastern region had lower chances (OR: 0.59, CI 0.34–1.07) of being informed about the method than their counterparts from the North. However, IUD acceptors from the southern region had higher odds (OR: 1.37; CI 0.96–1.96) of being informed about the method compared with acceptors from the North region.
Table 3. Percentage of IUD acceptors told about other methods, side-effects and side-effect management, and Method Information Index (MII), India, 2015–16
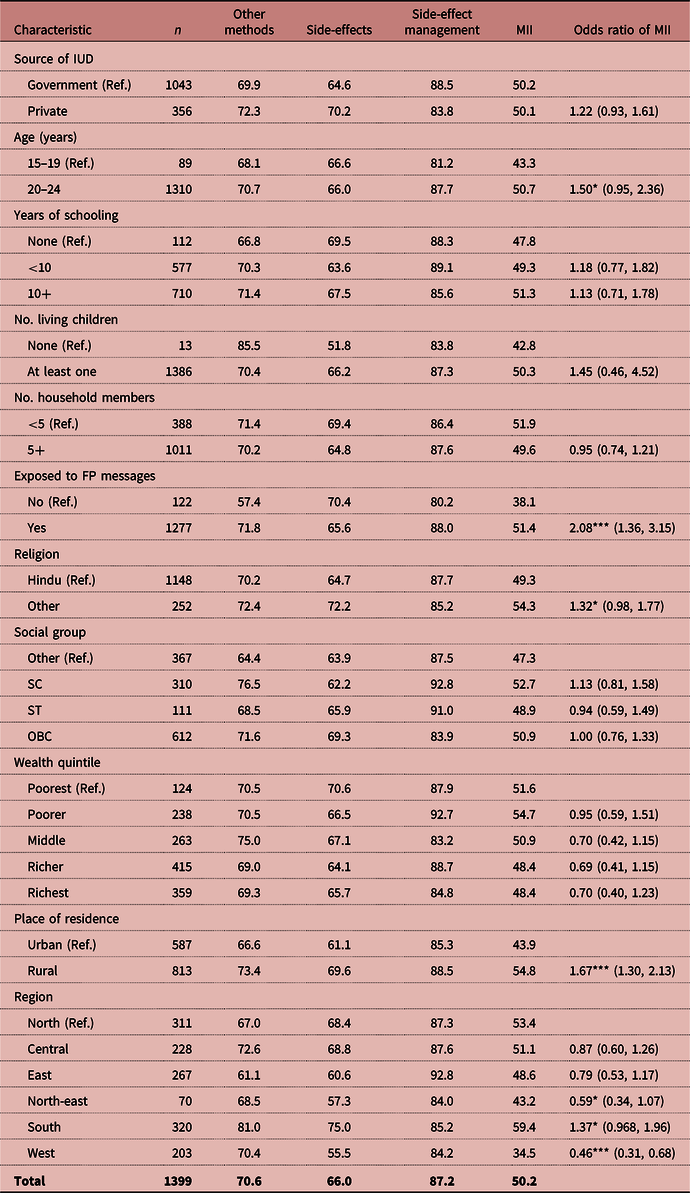
*p < 0.10; **p < 0.05; ***p < 0.01.
Method Information Index
Of the modern method users, only 36% were informed about other available methods of contraception, possible side-effects and side-effect management before their acceptance (Table 4). After controlling the effects of the socio-demographic characteristics of users, the likelihood of being informed about the methods was significantly higher among those using the oral contraceptive pill (OR: 1.75 CI 1.58–1.94), IUD (OR: 2.23, CI 1.97–2.52) and injectables (OR: 1.37, CI 0.97–1.94) compared with sterilized women. The chances of being informed about the methods were significantly higher among method users: exposed to FP messages (OR: 1.34, CI 1.19–1.50), those with 10 or more years of schooling (OR: 1.21, CI 1.06–1.37) and users from the richest wealth quintile (OR: 1.31, CI 1.09–1.57) than their respective counterparts. The likelihood of receiving method information was higher among users in SC (OR: 1.45, CI 1.31–1.61), ST (OR: 1.17, CI 1.02–1.35) and OBC (OR: 1.25, CI 1.14–1.38) categories than among those from the ‘other’ category. Users from rural areas (OR: 0.92, CI 0.84–1.00) and of households with five or more members (OR: 0.90, CI 0.84–0.97) were less likely to be informed about the methods. Users from the West region (OR: 0.60, CI 0.51–0.71) had lower chances of receiving method information compared with their counterparts from the North.
Table 4. Odds ratio of Method Information Index (MII) by women’s socio-demographic and economic characteristics, India, 2015–16

*p < 0.10; **p < 0.05; ***p < 0.01.
Discussion
The study found poor informed choice among young married women in India, although a sizable mumber of them reported using some form of modern method of contraception. The indicator of informed choice, the MII, was very low among young contracptive users and varied by specific methods, regions and socioeconomic profiles. This user’s perspective on the quality of counselling is useful for service providers and programmers to understand the client’s perception of service quality, although it has inherent problems of measurement error and might differ from the perspective of providers.
Although the most adopted method by young women in India, the study found an inadequate level of informed choice among sterilized women, along with wide variation in the provision of information; users in rural areas, the poorest households, from larger households, the non-educated and those without any exposure to FP messages were least informed. The counselling quality for sterilization was lower than that for pills, the IUD and injectables. An earlier study in India also found that health workers provide limited information about possible method side-effects and their management, and poor quality of care during and following sterilization (Koenig et al., Reference Koenig, Foo and Joshi2000). Sterilization acceptors usually undergo the procedure at a pre-fixed date and place and would have taken the decision to accept the method before arrival, and hence health providers might not have counselled them about alternative methods. Sterilization acceptance at a young age without informed choice is associated with post-sterilization health problems (Pradhan & Ram, Reference Pradhan and Ram2009) and regret, especially for the women without a son and in the case of child loss (Singh et al., Reference Singh, Ogollah, Ram and Pallikadavath2012). Female sterilization at an early age may also lead to low condom use, which is crucial for the prevention of RTI/STI as well as HIV/AIDS, particularly among those young women who are more vulnerable in traditional settings like India. Once a couple has undergone sterilization it is rather difficult to motivate/convince them to use condoms, which can protect them from acquiring HIV/AIDS, as most couples in India view family planning primarily as a means of spacing/regulating fertility and not as a way to protect against diseases/infections (Pandey et al., Reference Pandey, Sahu, Bakkali, Reddy, Venkatesh and Kant2012). The results suggest the need for better counselling of potential sterilization acceptors and re-emphasis on spacing methods to ensure informed decision-making and to avoid possible post-use health problems as well as regret. An earlier study evaluating informed contraceptive choices among 8077 potential clients who were told about all available contraceptive methods in the Indian national programme, found the majority opted for spacing methods (Baveja et al., Reference Baveja, Buckshee, Das, Das, Hazra and Gopalan2000). Lack of information or misinformation regarding spacing methods and less opportunity to adopt modern spacing methods due to poor affordability and accessibility have been shown to affect young women’s choice of female sterilization (Pandey et al., Reference Pandey, Sahu, Bakkali, Reddy, Venkatesh and Kant2012).
Informed choice in acceptance of the oral contraceptive pill and IUD was also found to be inadequate among these young Indian women. The finding is in concurrence with a past study (Koenig et al., Reference Koenig, Foo and Joshi2000), which revealed a limited choice of methods and insufficient information provided to women as a significant weakness of the family planning programme in India. It is worth mentioning that, unlike IUD users, most of whom have undergone the procedure in a health facility, sizeable percentages of pill users had obtained their most recent supply from a shop/pharmacy. These commercial outlets are also likely to be the initial supply source for many pill users and have a little scope for any form of counselling. Nevertheless, some modern spacing methods have side-effects: oral contraceptive pill users have reported changes in bleeding patterns, headaches, dizziness, nausea and mood changes (WHO, 2018), and the IUD can cause increased uterine bleeding and pain (Hubacher et al., Reference Hubacher, Chen and Park2009). Method-related reasons have been reported to be the principal factors for contraceptive discontinuation and switching (Blanc et al., Reference Blanc, Curtis and Croft2002; Ali et al., Reference Ali, Cleland and Shah2012; Sharma et al., Reference Sharma, Joshi, Nagar and Sharma2014).
Poor informed choice, coupled with side-effects, might lead to higher contraceptive discontinuation. High rates of contraceptive discontinuation, accompanied by too-early pregnancy among women who discontinue use for reasons other than the desire to get pregnant, are serious concerns due to their link to negative reproductive and public health outcomes. Cross-national studies have found that the majority of births resulting from contraceptive discontinuation are unintended (Blanc et al., Reference Blanc, Curtis and Croft1999; Curtis et al., Reference Curtis, Evens and Sambisa2011). Contraceptive discontinuations are also linked with higher unmet need and induced abortions (Casterline et al., Reference Casterline, El-Zanaty and El-Zeini2003; Cleland & Ali, Reference Cleland and Ali2004), adversely affecting women’s health. Increasing client-centred counselling for modern spacing methods could reduce the discontinuation of spacing methods along with informed choice.
The study found a better quality of counselling among the most disadvantaged social groups (SC/ST/OBC). The majority of these women had accepted female sterilization, thus increasing their chance of contact with a health care provider and receiving the subsequent method-related information. The general perception that disadvantaged groups have little or no knowledge about contracptive methods might have prompted health care providers to provide them with better counselling. In contrast, a majority of the women from the privileged group had often obtained their pills from a shop/pharmacy, so reducing their chance of contact with a health care provider and receiving method-related information.
Women exposed to FP messages were found to have received better counselling. An earlier study found that many targeted family planning messages/interventions using print or electronic media encourage women to seek more method-related information, enhancing informed choice in method acceptance (Modugu et al., Reference Modugu, Panda, Liberhan and Bhanot2018). This awareness may also encourage women to enquire more from the service providers before accepting a method.
The study revealed wide regional variation in quality of counselling, with women from the West region being the least counselled. Earlier studies found that women from the West region had less health care autonomy, especially in choice of family planning methods (Singh et al., Reference Singh, Sharma, Vishwakarma, Yadav, Srivastava and Maharana2019), which are primarily decided by the husband (Ghule et al., Reference Ghule, Raj, Palaye, Dasgupta, Nair and Saggurti2018), thus limiting women’s access to quality counselling. Poor quality of counselling in the West region may also be because of misconceptions about modern methods among likely providers (Hogmark et al., Reference Hogmark, Klingberg-Allvin, Gemzell-Danielsson, Ohlsson and Essén2013). The lack of consistent and accurate knowledge about contraception among providers has the potential to affect the quality of counselling (Dehlendorf et al., Reference Dehlendorf, Levy, Ruskin and Steinauer2010).
A strength of this study is that it reveals the ethical aspects of modern contraceptive method acceptance among young married women in India using a large sample size from a nationally representative survey with a robust sampling design. The findings are of use to efforts aimed at increasing contraceptive use, reducing discontinuation rates and and improving maternal and child health in the country. The MII can further be used to track FP programme performance and comparison across countries over time. The cross-sectional design of the survey, however, limited the causal association of any modern contraceptive method use with socioeconomic and demographic factors drawn from this analysis. There may be other factors such as motivation to use, access to emergency contraception and perceived side-effects that influence any specific method use, which were not included in the analysis due to data unavailability. Exposure to family planning messages as a predictor was weak as there was no information on the frequency/duration of exposure in the data. Additionally, inferences on the association between poor counselling and higher discontinuation should be made with caution as the data were obtained from continuing users.
Informed choice in acceptance of modern contraceptive methods was very low and varied by method, region and socioeconomic profile of the user. Inadequately informed choice violates the reproductive rights of women and might result in higher post-use health problems, discontinuation, unmet need, unintended pregnancies, induced abortion and regret, adversely affecting women’s health. Training of health/family planning workers about the importance of reproductive rights is urgently required to enhance informed contraceptive choice and improved health of young married women in India.
Funding
This research received no specific grant from any funding agency, commercial entity, or not-for-profit organization.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Ethical Approval
The survey was approved by the Institutional Review Board of the Institutions involved, and the datasets are available at https://www.dhsprogram.com for broader use in social research. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.








