Introduction
The temporal bone is one of the most complicated structures in the human body. Cochlear implantation, used to rehabilitate patients with severe sensorineural hearing loss, involves electrode insertion. Generally, three anatomical entrances (or ‘gates’) must be created during implantation. The surgical procedures required include cortical mastoidectomy, posterior tympanotomy and cochleostomy (or the round window approach).
Here, we describe these gate-creating surgical procedures, and emphasise that pre-operative temporal bone three-dimensional (3D) computed tomography (CT) is invaluable for ensuring patient safety by identifying surgical landmarks.
Materials and methods
Pre- and post-operative temporal bone CT images were analysed. Cochlear implantation was performed using the transmastoid and facial recess approaches. Electrode insertion into the scala tympani was achieved using either cochleostomy or the round window approach. High-resolution axial 3D-CT data were reconstructed using V-works software (version 4.0; CyberMed, Seoul, Korea). This was used to optimise the approach to the cochlea. All procedures complied with national and institutional guidelines for human experimentation (UC12RISE0064) and the Helsinki Declaration of 1975, as revised in 2008.
Results
Electrode insertion
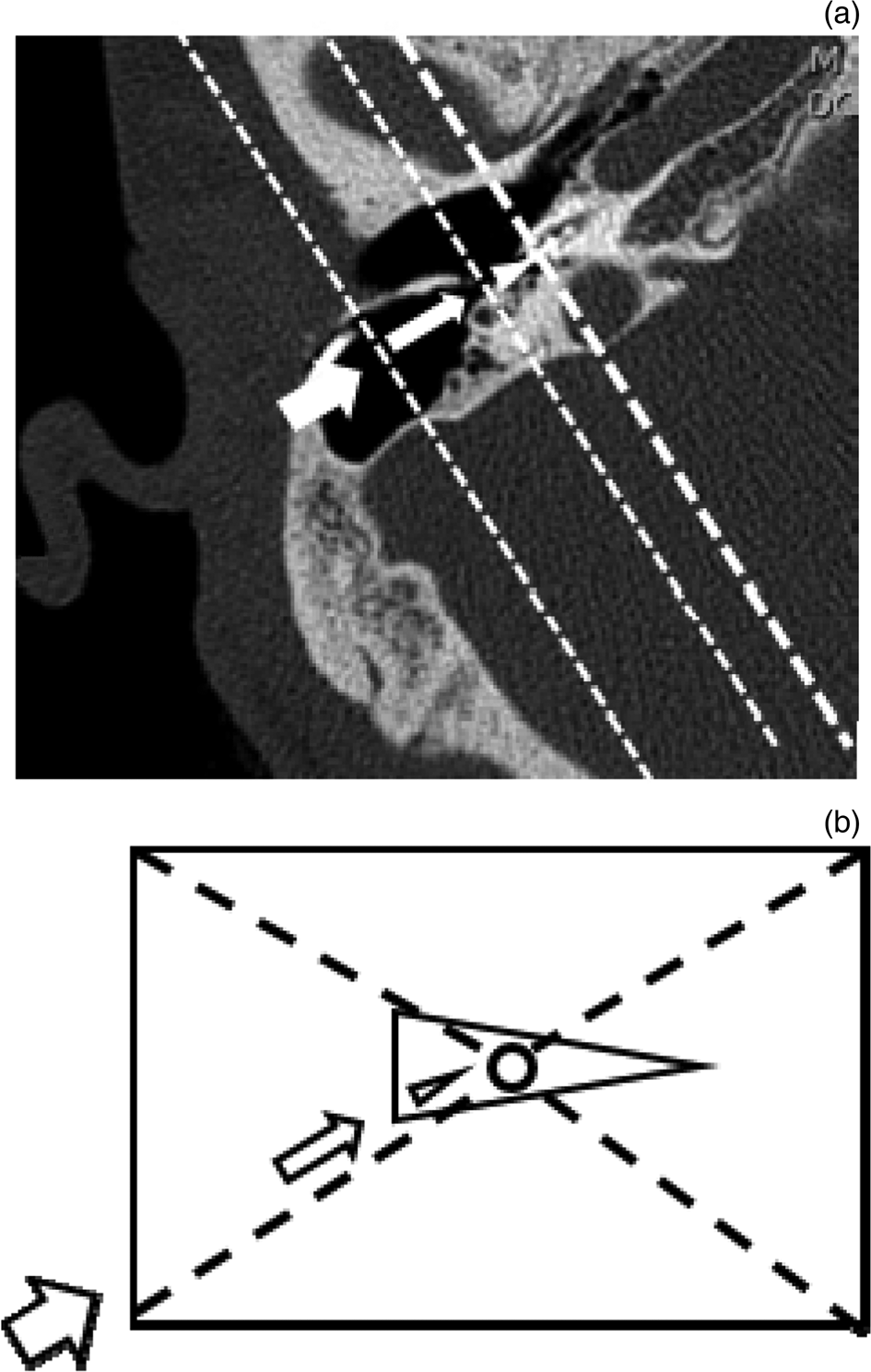
For electrode insertion into the cochlea, the electrode must pass through the mastoid cortex and the facial recess; portals are created via posterior tympanotomy and cochleostomy (or the round window approach). The inner structures are small and the field of view is obscured by intermediate structures. Good visibility is essential to ensure surgical success and avoid complications. Each gate should be sufficiently large to conform to the contour of the next gate (Figure 1).

Fig. 1. Post-operative axial computed tomography scan of the right temporal bone (a) shows the electrode inserted through entrances in the mastoid (thick arrow) and facial recess (thin arrow), and a portal created via cochleostomy (arrowhead). The entrances narrow with increasing distance from the operator. The cortical mastoidectomy (rectangle), posterior tympanotomy (triangle) and cochleostomy (round window; circle) portals are shown (b).
Mastoidectomy
Mastoidectomy does not need to be extensive; the aim is not to eliminate pathological lesions of mastoid air cells (such as in otitis media), but rather to create a good field of vision for posterior tympanotomy. If the mastoid cavity is sclerotic, a gate can be extended through the middle fossa dura superiorly, the jugular bulb inferiorly, the external auditory canal anteriorly and the sigmoid sinus posteriorly (by reference to the lateral head position) (Figure 2).

Fig. 2. Three-dimensional reconstruction of the lateral surface of the temporal bone (a) and virtual cortical mastoidectomy (b). Critical temporal bone structures include the facial and chorda tympani nerves (yellow), the sigmoid sinus (blue), the labyrinth (green), the ossicles (white) and the cochlea (red).
Drilling of the mastoid cortex margin or a bony remnant of air cells helps to fix the electrode array in place. Most patients requiring a cochlear implant exhibit a well-pneumatised temporal bone and no history of otitis media. However, care should be taken when drilling a sclerotic mastoid cavity, a low-lying middle fossa dura, an anteriorly displaced sigmoid sinus or a high jugular bulb (Figure 3).

Fig. 3. Axial computed tomography scan of the right temporal bone (a) shows a sclerotic (arrow) and anteriorly displaced (arrowhead) sigmoid sinus. Care should be taken to avoid damaging the sinus (arrowhead) during mastoid drilling (b).
If the mastoid cavity is sclerotic, it is difficult to locate the mastoid antrum and short process of the incus. The lack of surgical landmarks may result in an iatrogenic lateral semicircular canal fistula or facial nerve injury during mastoid drilling. Damage to the middle fossa dura can cause cerebrospinal fluid leakage, while damage to the sigmoid sinus or high jugular bulb can trigger massive bleeding.
Posterior tympanotomy
The size of the gate created via posterior tympanotomy is limited by the fossa incudis superiorly, facial nerve posteriorly and chorda branch anteriorly (relative to the lateral head position) (Figure 4).

Fig. 4. The gate size in posterior tympanotomy is limited by the fossa incudis superiorly (arrow), facial nerve inferiorly (arrowhead) and chorda branch anteriorly (thin arrow) (relative to the lateral head position). Three-dimensional reconstructed image (yellow = facial and chorda tympani nerves, blue = sigmoid sinus, green = labyrinth, white = ossicles, red = cochlear) (a), microscopic view (b) and superimposition (c). The round window niche (thin arrowhead) is apparent through the facial recess.
The hard bone of the facial nerve fallopian canal can be located by removing mastoid cavity air cells lying posterior to the external auditory canal. The mastoid antrum, the short process of the incus and the bony contour of the lateral semicircular canal serve as surgical landmarks when seeking to locate the mastoid segment of the facial nerve, which should be preserved after identification. The safety of posterior tympanotomy is enhanced by locating the chorda tympani branch. If this is not identified, dissection may proceed in the wrong direction (i.e. through the posterior wall of the ear canal and not the middle-ear cavity) (Figure 5).

Fig. 5. The chorda tympani is an important landmark when searching for the facial nerve (arrow) and facial recess. An inappropriate drilling direction may lead to destruction of the posterior part of the external auditory canal. Post-operative axial computed tomography reveals thinning of the bone posterior to the external auditory canal (arrowhead) caused by misidentification of the chorda tympani landmark.
It is desirable to preserve the chorda tympani nerve; damage may cause changes in taste perception. The posterior tympanotomy should be sufficiently large to allow identification of the round window niche and membrane. Pre-operative 3D-CT can be used to confirm that the round window is visible, via rotation of the reconstructed image after virtual mastoidectomy and posterior tympanotomy (Figure 6).

Fig. 6. Reconstructed three-dimensional images (lateral to anterior) (a–c). The round window niche is not evident (a). The anterior portion of the round window niche is shown (b). The entire contour of the round window is apparent (c). Yellow = facial and chorda tympani nerves, blue = sigmoid sinus, green = labyrinth, white = ossicles, red = cochlear
Confirming the round window contour
The round window of the middle-ear canal is found by first identifying the oval window of the stapes, which lies anterior and superior to the round window. A round window reflex confirms the presence of a round window membrane; perilymph moves from the oval to the round window when the ossicles are touched.
If a round window pseudo-membrane lies external to the real membrane, the reflex is absent. The round window membrane is sometimes obscured by protruding bone of the high jugular bulb or mucosal thickening of the middle-ear cavity (Figure 7).

Fig. 7. Pre-operative axial (a) and post-operative coronal (b) temporal bone computed tomography images. When inserting the electrode through the round window membrane or a cochleostomy portal, it is essential to identify the contour of the round window niche. The contour may be obscured by mucosal thickening of the middle-ear promontory (arrow) (a) or protrusion of the bony structure of the high jugular bulb (arrowhead) (b).
Cochleostomy or round window opening
The two principal approaches to electrode insertion are cochleostomy and the round window approach. The former approach creates a cochlear portal anteroinferior to the round window membrane, while the latter uses the round window itself to advance the electrode (Figure 8).

Fig. 8. When inserting the electrode via the round window approach, drilling out the round window niche improves visibility of the round window membrane (arrow) (a). Prior to insertion, the size of the round window entrance is measured (b) and the electrode is then inserted (c). Post-operative three-dimensional computed tomography image showing the electrode inserted into the cochlea (yellow = facial and chorda tympani nerves, red = electrode arrays of cochlear implant) (d).
Recently, non-invasive (‘soft’) cochlear implantation has been recommended, to preserve the inner cochlear structure and residual hearing. The round window approach is thus preferred. However, it can be difficult to observe the entire contour of the window through the orifice created by posterior tympanotomy if the window lies posteromedial to the fallopian canal of the facial nerve.
Therefore, when using the round window approach, posterior tympanotomy may be wider than required for cochleostomy. The electrode tip may damage the osseous spiral lamina if an orthogonal approach is taken to the round window membrane (Figure 9).

Fig. 9. Reconstructed three-dimensional images (at different angles) after cochlear implantation using cochleostomy (a & b) and the round window approach (c & d). The direction of insertion is more central (arrow) for the round window approach than for cochleostomy (arrowhead). The round window is shown in green (thin arrow).
Cochleostomy involves the creation of a hole anterior or inferior to the round window. If the facial nerve sheath is exposed, care must be taken to ensure that the burr shaft does not damage it during drilling. The electrode can be inserted with confidence after identifying the scala tympani, the basilar membrane superiorly and the modiolus medially. However, the heat and vibration associated with drilling may damage cochlear hair cells, thus compromising residual hearing.
Electrode insertion
The electrode insertion method varies slightly according to the type of electrode placed. Insertion should be slow; if resistance is felt, it is prudent to retract the electrode and try again. When inserting an electrode through the round window, it may fold if the tip is buckled by the cochlear hook. If the tip slides posterior to the modiolus, it may be inserted incorrectly. It is important to ensure that the tip lies anterior to the modiolus of the scala tympani. Cochlear anomalies, ossification and small dimensions (Figure 10) will be evident on pre-operative CT.

Fig. 10. A space-occupying structure (arrow) in the basal cochlear turn is evident on pre-operative axial temporal bone computed tomography (CT) (a). On post-operative axial CT, electrode array insertion was not complete; one ball electrode (arrowhead) lay outside the cochleostomy site (b).
Discussion
Prior to cortical mastoidectomy, it is important to determine whether or not the bone is well-pneumatised. Sclerotic cases involve a narrow mastoid space surrounded by dura, the sigmoid sinus and the posterior wall of the external auditory canal. It is important to avoid damaging these boundary landmarks. Well-aerated cases with thin air cell septa may have thin facial bony canals. Careful drilling is essential to avoid canal damage. During mastoidectomy, it is important to locate the aditus ad antrum, which ensures the absence of iatrogenic trauma. However, a sclerotic mastoid, as well as granulation tissue in the middle ear and mastoid, may hinder identification of the aditus ad antrum.Reference Long, Athar, Mahmud and Saim1
Iatrogenic trauma of the facial nerve principally affects the second genu of the fallopian canal. This may occur when drilling the mastoid toward the aditus. The surgeon may inappropriately drill more inferiorly than the aditus. As the second genu of the facial nerve lies inferior and medial to the aditus, this is the most likely site of injury.Reference Long, Athar, Mahmud and Saim1 The semicircular canals may also be accidentally injured when drilling toward the aditus. Injury to the labyrinth can cause sensorineural hearing loss and serious suppurative intracranial infection.Reference Long, Athar, Mahmud and Saim1
Anterior displacement of the sigmoid sinus may lead to damage during mastoid drilling. An anteriorly located sigmoid sinus often narrows the mastoidectomy boundary, preventing the surgeon from reaching the antrum because of the limited field of view.Reference Çam and Karataş2 When creating the second gate via posterior tympanotomy, it is essential to identify the facial canal (to avoid damaging the facial sheath) and the chorda tympani. The latter structure can be located via soft drilling with a large diamond burr under irrigation.
Paralysis of the facial or chorda tympani nerve is a potential complication of the facial recess approach; such complications are rare but serious, and their likelihood can be minimised by obtaining a full understanding of facial recess anatomy. The facial recess length and width, and the angle between the facial and chorda tympani nerves, are larger in pneumatised temporal bones than in sclerotic and diploic bones. Facial recess length varies greatly by the type of pneumatisation. Variations in the origin of the chorda tympani branch and pneumatisation pattern affect the size of the facial recess.Reference Jain, Deshmukh, Lakhotia, Kalambe, Chandravanshi and Khatri3 The round window niche is not always fully exposed by posterior tympanotomy. Öztürk et al. found that complete round window exposure through the facial recess was possible for most temporal bones (79.2 per cent).Reference Öztürk, Göde, Çelik, Orhan, Bilge and Bilgen4
For the third gate (created via cochleostomy or the round window approach), pre-operative CT evaluation of round window shape and position, cochlear ossification, and any small dimensions or narrow turns, is very useful.Reference Karkas, Champfluer, Uziel, Mondain, Puel and Venail5 Thinning of the posterior external auditory canal wall may improve round window visibility. The round window varies markedly in size and shape.
The role of the round window as a portal for electrode implantation is well supported by the fact that it is the safest landmark for identifying the scala tympani. Hamamoto et al. used a pin gauge to classify the topographical relationship between the facial and chorda tympani nerves and posterior wall of the external acoustic canal into five types.Reference Hamamoto, Murakami and Kataura6 It can be difficult to find the round window if the middle-ear mucosa is thickened by chronic otitis media, anatomically changed by prior surgery or obstructed with a pseudo-membrane; gentle dissection using micro-instruments may be required.
Factors that influence the optimal trajectory for atraumatic electrode insertion include the orientation and size of the cochlear basal turn, and the anatomy of the hook region that lies immediately behind the round window membrane.Reference Luers, Hüttenbrink and Beutner7 Several aspects of round window anatomy are relevant to its use as a portal for electrode insertion. Certain anatomical features in fact suggest that the round window is not the ideal portal for cochlear implantation. An electrode inserted straight through the round window will be aimed directly at the modiolus.Reference Roland, Wright and Isaacson8 If the posterior-superior overhang of the niche is not drilled away, it is almost impossible to insert an electrode into the scala tympani alone; instead, it will be directed toward the modiolar wall and spiral ganglion.Reference Roland, Wright and Isaacson8 In one study, cochlear electrodes were more likely to cause osseous spiral lamina trauma when placed in the scala vestibuli via round window implantation rather than via cochleostomy.Reference Zhou, Friedmann, Treaba, Peng and Roland9
The goal of cochleostomy is to enter the scala tympani as near as possible to the centreline or main axis, to avoid the need for drilling of, or application of direct force to, the spiral ligament region of the outer and superior walls.Reference Adunka, Radeloff, Gstoettner, Pillsbury and Buchman10 Thus, an ideal insertion vector minimising the force delivered to, and subsequent damage of, intracochlear structures is required.Reference Meshik, Holden, Chole and Timothy11,Reference Breinbauer and Praetorius12 Electrodes can become displaced even in patients with normal inner-ear anatomy. In particular, an electrode may be inappropriately directed into the superior or lateral semicircular canal through the vestibuleReference Jain, Deshmukh, Lakhotia, Kalambe, Chandravanshi and Khatri3,Reference Breinbauer and Praetorius12 or internal auditory canal, or even the internal carotid artery. Electrode misplacement is usually caused by drilling along an inappropriate axis. A microscope should be used to identify the round window niche and membrane. Computed tomography of a cochlear duct lying under the promontory of the middle-ear cavity is very helpful.
The internal carotid artery and jugular bulb are at risk during cochlear implantation. Therefore, the access route to the cochlear lumen should be chosen before surgery.Reference Sahni, Singla, Gupta, Gupta and Aggarwal13 A high-riding jugular bulb may cover the round window or basal cochlear turn, thereby hindering access to the cochlear lumen via the standard transmastoid approach.Reference Di Lella, Falcioni, Piccinini, Iaccarino, Bacciu and Pasanisi14 Hara et al. found that reconstructed 3D-CT images were useful when surgically planning cochlear implantation in a patient exhibiting an abnormal facial nerve course;Reference Hara, Takahashi and Kanda15 3D images are optimal for assessing temporal bone anatomy, and they show the skull base and any middle- or inner-ear anomalies.Reference Joshi, Navleka, Kishore, Reddy and Kumar16,Reference Nakamura, Dias, Sasaki, Sugimoto, Hatano and Ito17 Breinbauer and PraetoriusReference Breinbauer and Praetorius12 described the optimal spatial orientation of insertion vectors for cochleostomy and the round window approach through 3D reconstruction of the temporal bones of 50 cochlear implant candidates (100 ears).
• The gate-creating surgical procedures required for cochlear implantation include cortical mastoidectomy, posterior tympanotomy and cochleostomy (or round window approach)
• Gates should be sufficiently large to conform to the next gate's contour, and to ensure surgical success and safety
• Pre-operative temporal bone three-dimensional (3D) computed tomography (CT) detects anatomical variations much more effectively than two-dimensional imaging
• Pre-operative temporal bone 3D-CT orients the surgeon spatially and can minimise complications
High-resolution CT is the only imaging modality that can pre-operatively detect abnormalities, thus minimising the risks associated with an abnormally located facial nerve or narrow recess, for example.Reference Karkas, Champfluer, Uziel, Mondain, Puel and Venail5 Two-dimensional imaging lacks the power of 3D-CT. Round window visibility can be assessed by rotating the 3D reconstructed image after virtual mastoidectomy and posterior tympanotomy. Three-dimensional CT also reveals important features of the temporal bone, thus allowing surgeons to identify and address any difficulties expected during implantation.
Conclusion
Ideally, cochlear implant surgery should be free of iatrogenic complications, such as facial paralysis; it should also minimise cochlear damage, to preserve residual hearing. Pre-operative CT is invaluable for obtaining spatial information on neurovascular structures and ensuring the safe passage of electrodes through the gates created for their insertion.
Competing interests
None declared