Introduction
In adults, otitis media with effusion (OME) is less common than in children but is not without considerable morbidity.Reference Mills and Hathorn1 Otitis media with effusion in adults can be associated with sinonasal disease, reflux, Eustachian tube dysfunction and malignancy in the post-nasal space.Reference Mills and Hathorn1 Incidence of malignancy in patients with OME as the sole presentation varies greatly between countries where nasopharyngeal carcinoma (NPC) is endemic (5.5 per cent)Reference Sheu, Ho, Kuo and Juan2 and non-endemic like the UK (0.4–1.4 per cent).Reference Dempster and Simpson3,Reference Gaze, Keay, Smith and Hardcastle4
Aural symptoms (e.g. tinnitus, impaired hearing) are present in 62.2 per cent of patients with NPC. The correlation of OME with NPC has led to examination of the post-nasal space being recommended as part of investigations of adults with OME.Reference Gaze, Keay, Smith and Hardcastle4 However, this recommendation has been questioned by other authors from non-endemic areas.Reference Dempster and Simpson3,Reference Abu-Ghanem, Neiderman, Horowitz, Yehuda, Leshno and Abu-Ghanem5–Reference Glynn, Keogh, Ali, Timon and Donnelly7 Given this controversy, we conducted a systematic literature review to identify alternative investigative modalities for adult patients with OME that we could implement in a new management protocol.
Data on outcomes in adults with OME are not as established as in children, who generally have a favourable outcome. This is especially the case in adults with NPC who have been shown to have worse prognosis in terms of complications.Reference Yung and Arasaratnam8 The same authors reported on the outcome of ventilation tubes in adults without NPC and with OME in the 15–18 months after insertion. Persistent discharge was present in 4 out of 53 patients (7.5 per cent), and there was recurrence of OME in 19 out of 53 patients (35.8 per cent).Reference Yung and Arasaratnam8 Another study investigated the outcome of ventilation tubes in those aged over 15 years compared to younger patients. Otitis media with effusion was bilateral in 30 per cent of the younger group, whereas it was 8 per cent in the adult group. The younger group was also 20 times more likely to recover spontaneously (40 per cent, compared to 2 per cent).Reference Ogawa9
This paper presents the rate of complications, and describes our experience in terms of surgical outcomes of examination under anaesthesia of the post-nasal space and grommet insertion in adults presenting solely with OME.
Materials and methods
Ethical considerations
This study received approval from the local clinical research and audit committee. Patients’ data were anonymised and stored securely.
Literature review
A systematic review of PubMed literature was performed on 14 of November 2020 using a combination of the two search terms: ‘nasopharyngeal carcinoma otitis media with effusion’ and ‘adults unilateral otitis media with effusion’. Non-English language articles, articles on patients aged less than 19 years, those published before 1980, review articles, case reports and animal studies were excluded. The search of the first term returned 64 articles and the search of the second term returned 62 articles. The results are presented in a modified Preferred Reporting Items for Systematic Reviews and Meta-Analyses (‘PRISMA’) flow diagram (Figure 1).Reference Moher, Liberati, Tetzlaff and Altman10

Fig. 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (‘PRISMA’) flow diagram of the literature review. NPC = nasopharyngeal carcinoma
Subjects
This retrospective cohort study was conducted using a local database of adult patients who underwent examination under anaesthesia of the post-nasal space with unilateral or bilateral grommets, between January 2014 and January 2016, for otitis media with effusion. Patients who underwent grommet insertion for Ménière's disease or for recurrent acute otitis media were excluded.
Data collected
The data collected included patients’ demographics, presenting complaints, any subsequent head and neck radiological studies, outcome and complications of grommet insertion, and outcome of the examination under anaesthesia of the post-nasal space.
We also compared the number of examinations under anaesthesia of the post-nasal space recorded nationally11 compared to our local data.
Results
Patient demographics
A total of 103 consecutive adult otitis media with effusion (OME) patients were scheduled for examination under anaesthesia of the post-nasal space and ventilation tube insertion between January 2014 and January 2016. Follow-up duration ranged from 39 to 63 months. Two patients were excluded as they had T-tubes instead of grommets. Three further patients were excluded because of missing data, which prevented meaningful analysis. The following analysis was conducted on the remaining 98 patients.
Table 1 highlights patient demographics and presenting symptoms.
Table 1. Patients’ demographics and presenting symptoms

Surgical outcomes and grommet complications
Table 2 details complications of the grommets, which were present in 36 out of 98 patients (36.73 per cent). Six patients of the thirteen with persisting hearing loss were fitted with hearing aids with no further problems.
Table 2. Complications of grommets

CSOM = chronic suppurative otitis media; GA = general anaesthesia; OME = otitis media with effusion
Of the 27 patients who had recurrence of OME after grommet extrusion during the follow-up period, 15 (55.56 per cent) were re-scheduled for further ventilation tube insertion, with some of them having T-tubes. Of these 15 patients, 7 (46.67 per cent) had further complications; 1 patient had infections followed by blockage, and the other 6 had either infections (3 out of 15) or blockage (3 out of 15). For the remaining 12 patients who re-presented with OME and did not have further ventilation tubes, 4 were referred for hearing aids, another 4 had no documented action, 2 agreed on no further action, 1 was scheduled for further grommet insertion but did not attend and in 1 patient the OME resolved spontaneously.
Examination under anaesthesia outcomes
Findings of the examination under anaesthesia of the post-nasal space in OME adult patients were documented as abnormal in three patients: ‘enlarged adenoids’ in the first patient, ‘oedematous tissues’ in the second and ‘bulky tissues look inflammatory’ in the third. Biopsies were taken from these three patients and from one patient with normal post-nasal space (by random sampling of apparently normal tissue).
No patients re-presented to ENT at a later date with post-nasal space pathology during the follow-up period of this study.
Flexible nasoendoscopy was documented as performed in clinic in 50 out of 98 patients (51.02 per cent). The flexible nasoendoscopy findings were abnormal in only four patients: the first patient had fullness in the superior aspect of the post-nasal space, the second had adenoid remnants, the third had post-nasal space erythema and rhinitis, and the fourth had laryngeal Reinke's oedema.
In England, in the year 2018–19, examination under anaesthesia of the post-nasal space was performed in 1979 adults (aged 18 years and older). Fewer than a quarter of these were carried out as day-case procedures.11 There are 126 ENT units in England, meaning that an average of 15 examinations under anaesthesia of the post-nasal space took place in each unit in one year. In our unit, it stands at 50 procedures per year.
A protocol for investigating patients with OME as the sole presentation was suggested as a result of this study, and was approved for use in our hospital (Figure 2).
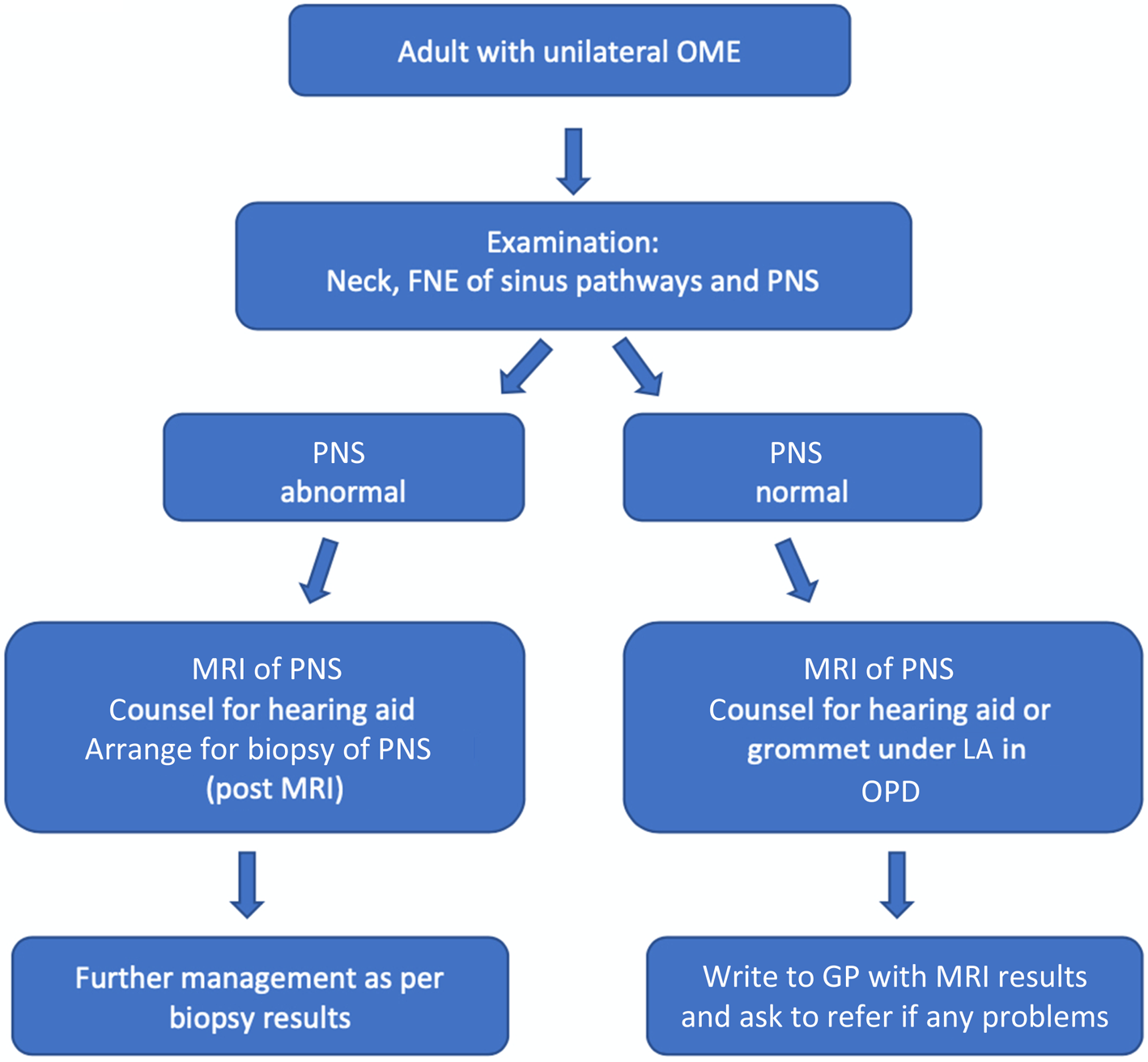
Fig. 2. A protocol for management of adult patients with unilateral otitis media with effusion (OME). (Written by H Mohammed (supervising consultant: P Yates); date February 2020, review date February 2021.) FNE = flexible nasoendoscopy; PNS = post-nasal space; LA = local anaesthesia; MRI = magnetic resonance imaging; OPD = out-patient department; GP = general practitioner
Discussion
Literature review
Seven studies were included in the final analysis.Reference Sheu, Ho, Kuo and Juan2–Reference Gaze, Keay, Smith and Hardcastle4,Reference Glynn, Keogh, Ali, Timon and Donnelly7,Reference Shilo, Abu-Ghanem, Yehuda, Weinger, Fliss and Abergel12–Reference Leonetti14 Glynn et al. recommend the need for close follow up with serial flexible nasoendoscopy in those with a normal post-nasal space.Reference Glynn, Keogh, Ali, Timon and Donnelly7 Abu-Ghanem et al. recommend magnetic resonance imaging (MRI) even in patients with an apparently normal post-nasal space, given the risk of cancer with submucosal spread.Reference Abu-Ghanem, Neiderman, Horowitz, Yehuda, Leshno and Abu-Ghanem5 The same group suggested that the MRI scan could offer a cost-effective alternative to biopsy of the post-nasal space.Reference Shilo, Abu-Ghanem, Yehuda, Weinger, Fliss and Abergel12
Other authors recommend radiological investigations in adults with otitis media with effusion (OME) lasting more than two months, although the type of radiological investigation is not universally agreed.Reference Ramakrishnan, Sparks and Berryhill15 This is supported by studies from non-endemic areas on adult patients with unilateral OME and a normal post-nasal space, but with abnormal cross-sectional radiological evaluation findings.Reference Lee, Weiner and Campbell13,Reference Leonetti14
Grommet complications in adults
Our study demonstrates the relatively high complication rates associated with grommets in adult patients with isolated OME. Moreover, it shows that OME in this cohort appears to have a different natural history, with considerably less spontaneous resolution,Reference Ogawa9 and with a different spectrum of complications than in children.Reference Yung and Arasaratnam8,Reference Gates, Avery, Prihoda and Holt16 The complication rate is even higher in patients who underwent grommet insertion to treat recurrence of OME after the extrusion of a previously inserted grommet. In this subgroup of patients, other solutions may be better, such as hearing aids or balloon dilation Eustachian tuboplasty.
The rate of OME recurrence in our study cohort was lower than that reported in the literature.Reference Yung and Arasaratnam8,Reference Wen-Yuan, Chun-Fu and Chang17 However, one of these studies took place in a country where nasopharyngeal carcinoma is endemic, and included a large number of patients with head and neck cancer.Reference Wen-Yuan, Chun-Fu and Chang17 The rate of otorrhoea in our study was higher than that reported in a non-endemic country,Reference Gates, Avery, Prihoda and Holt16 but lower than that reported in an endemic one.Reference Wen-Yuan, Chun-Fu and Chang17
Fifteen patients reported no improvement in their symptoms, mainly hearing loss, following grommet insertion. This could be related to the presence of other causes of conductive hearing loss, such as tympanosclerosis, scarring and erosion of the long process of the incus.
In view of the considerable complication rate, it is important to discuss the risks openly with patients. This study offers quantification of the risks, which can be used as part of the consent process and to inform shared decision-making.
• In adults, otitis media with effusion causes considerable morbidity and has poorly established outcomes
• Over one-third of adults develop complications following grommet insertion for isolated otitis media with effusion (OME), with an increased complication rate with further grommets
• Hearing aids should be considered in OME patients given the relatively high complication rate and recurrence risk
• Examination under anaesthesia of the post-nasal space with biopsy has a very low yield and alternative investigation modalities should be considered
• The evidence-based complication rate helps in informed decision-making
Examination under anaesthesia
Our results support the low yield of examination under anaesthesia of the post-nasal space in patients presenting solely with OME, in accordance with previous studies.Reference Dempster and Simpson3,Reference Abu-Ghanem, Neiderman, Horowitz, Yehuda, Leshno and Abu-Ghanem5–Reference Glynn, Keogh, Ali, Timon and Donnelly7
Moreover, recent studies from endemic countries show that MRI offers significantly higher sensitivity than flexible nasoendoscopy in investigating the post-nasal space, and non-significantly higher sensitivity than endoscopic biopsy of the post-nasal space.Reference King, Vlantis, Bhatia, Zee, Woo and Tse18 Previous case reports have highlighted that post-nasal space malignancy presenting with OME can nevertheless show a normal post-nasal space on flexible nasoendoscopy.Reference Lee, Weiner and Campbell13 Thus, a 2015 study from a non-endemic country advocates using MRI to reveal submucosal cancers in the apparently normal post-nasal space.Reference Abu-Ghanem, Neiderman, Horowitz, Yehuda, Leshno and Abu-Ghanem5
In our unit, the number of examinations under anaesthesia of the post-nasal space is higher than the national average,11 at 50 per year. This could be simply because of the population size, or the tendency to carry out examinations under anaesthesia of the post-nasal space in patients who choose to go down the route of grommets inserted under general anaesthesia (GA) when they present with OME.
In the presence of a relatively inexpensive and high-quality MRI scan, the need for examination under anaesthesia of the post-nasal space is debatable, especially when factoring in coronavirus disease 2019 risks and the inconvenience of GA for patients, including a longer interruption to work and the need for an overnight stay in some cases.
Our new management protocol recommends an MRI scan even in the presence of a normal post-nasal space on flexible nasoendoscopy. This is because of the possibility of deeper lesions, such as submucosal carcinomas and parapharyngeal space lesions, that could be responsible for the OME, and for which MRI has greater sensitivity than examination under anaesthesia of the post-nasal space, as discussed above. The new protocol also recommends requesting the MRI on the first visit rather than following a three month ‘watch and wait’ period, as most patients have already waited three months prior to the appointment.
Limitations
Limitations of this study include the retrospective collection of data. We have also assumed that patients who did not present back to our centre with complications or recurrence were not presenting elsewhere or lost to follow up, meaning that our figures may underestimate the rates of complications and recurrence. Finally, the number of documented flexible nasoendoscopy examinations in clinic is lower than expected, and prevents conclusions being drawn on sensitivity and specificity for post-nasal space malignancy compared with examination under anaesthesia and radiological imaging.
Conclusion
Grommets in adults with otitis media with effusion (OME) as the sole presenting feature carry high complication rates, especially in those with previously inserted grommets.
Awareness of the incidence and nature of grommet complications in adults is important for reaching shared informed decisions when counselling patients for grommet insertion. Further research is needed to evaluate factors that could be responsible for OME recurrence in this group of patients.
If not opting for grommets, there is low yield from examination under anaesthesia of the post-nasal space. We propose that alternatives are considered, such as MRI, which may be superior and more cost-effective.
Competing interests
None declared






