Approximately 25% of children born with CHD have a critical form of the disease, requiring surgical intervention in the first year of life. Reference Hoffman and Kaplan1 These children are often subjected to long hospital stays, frequent readmissions, and life-threatening complications. Long term, children with critical CHD are at high risk for neurodevelopmental impairments including problems regulating emotions and behaviours, Reference Marino, Lipkin and Nideewburger2 which can impact school performance, social functioning, and quality of life. To improve outcomes for this growing population, modifiable risk factors for neurodevelopmental impairment that can be targeted for prevention and intervention should be identified.
Parents of children with critical CHD are exposed to potentially traumatic medical events related to their child’s disease (e.g., witnessing cardiac arrest/resuscitation, life-threatening complications, painful procedures). In turn, up to 80% of parents report clinically significant post-traumatic stress symptoms including intrusive re-experiencing of traumatic events, avoidance of trauma reminders, negative thoughts and feelings, and heightened physiological reactivity. Reference Woolf-King, Anger and Arnold3 Up to 30% meet the full criteria for post-traumatic stress disorder. Reference Woolf-King, Anger and Arnold3 While post-traumatic stress symptoms resolve over time for some parents of children with CHD, these symptoms persist for a substantial portion. Over 20% of mothers and over 13% of fathers of children with heart disease aged 8–18 who were an average of roughly 9 years out from surgeries reported moderate-to-severe post-traumatic stress symptoms, with even higher rates amongst parents of children with single-ventricle physiology. Reference Wray, Cassedy and Ernst4 Parental post-traumatic stress symptoms are associated with worse psychosocial functioning and quality of life in children with CHD Reference DeMaso, Labella and Taylor5,Reference Ernst, Marino and Cassedy6 and may be a modifiable risk factor for poor child outcomes.
Although the mechanisms underlying the relationship between parental post-traumatic stress symptoms and child psychosocial functioning are not well understood, parenting may play a role. The few published studies on the relationship between post-traumatic stress symptoms and parenting have mixed results. Reference Christie, Hamilton-Giachritsis and Alves-Costa7 However, the Parent Stress and Resilience in CHD model, which provides a theoretical basis for understanding the impact of parental stress on the family, suggests that parental stress responses to CHD, including post-traumatic stress symptoms, will likely impact parenting and child psychosocial functioning. Reference Lisanti8 Parents of children with CHD report high levels of parenting vigilance, and compared to parents of healthy children, perceive their child to be more vulnerable. Reference Meakins, Ray and Hegadoren9,Reference Vrijmoet-Wiersma, Ottenkamp and van Roozendaal10 Parents describe struggling to balance the need to protect with the need to let their child with CHD be a “normal kid. Reference Rempel and Harrison11 ” These findings suggest the potential for overprotective parenting, defined as “excessive parental regulation of children’s activities and routines, encouragement of children’s dependence on parents, and instruction to children on how to think or feel [ Reference McLeod, Wood and Weisz12 p. 156].” Overprotective parenting may increase the risk for mental health issues amongst offspring. For example, overprotective parenting is related to separation anxiety in preschool children. Reference Orgilés, Penosa and Morales13 Overprotective parenting of extremely low birth weight infants increased the risk for anxiety disorders and substance use disorders in adulthood. Reference Day, Dobson and Schmidt14 However, prior studies have not directly assessed the relationships between parental post-traumatic stress symptoms, overprotective parenting, and child outcomes and not in a population of parents of children with CHD.
Whereas parental post-traumatic stress symptoms may increase the risk for poor child psychosocial outcomes, parental post-traumatic growth may serve as a protective factor. Post-traumatic growth is defined as positive changes resulting from the struggle with life-changing events. Reference Tedeschi and Calhoun15 Through positive reframing of traumatic events, post-traumatic growth may provide parents with greater psychological resources to handle the stressors of parenting a medically complex child. Some studies have documented a positive association between parental and child post-traumatic growth amongst families exposed to traumatic events, Reference Hafstad, Gil-Rivas and Kilmer16 whereas others have shown no association between these constructs. Reference Bernstein and Pfefferbaum17 To our knowledge, no studies have examined the relationships between parental post-traumatic growth, parenting, and child psychosocial outcomes.
The current study aimed to test the associations amongst parental post-traumatic stress symptoms, post-traumatic growth, overprotective parenting, and child emotional/behavioural problems in families of young children with critical CHD. It was hypothesised that (1) parental post-traumatic stress symptom severity would be positively associated with overprotective parenting and child emotional/behavioural problems; (2) overprotective parenting would be positively associated with child emotional/behavioural problems; and (3) overprotective parenting would mediate the relationship between parental post-traumatic stress symptom severity and child emotional/behavioural problems. Given the lack of prior research on post-traumatic growth in parents of children with critical CHD and inconsistent findings regarding its relationship with child outcomes in other populations, analyses involving parental post-traumatic growth were exploratory.
Methods
Participants and procedures
Participants were 60 parents of young children (aged 1–6) who had previously undergone cardiac surgery for critical CHD within the first year of life. They were recruited from an existing online sample (n = 108) of parents of children with critical CHD from across the United States of America that was formed as part of a larger qualitative study examining parent perspectives on family-based psychosocial care for CHD. Reference Hoffman, Karpyn and Christofferson18–Reference Gramszlo, Karpyn and Christofferson20 This larger study used a maximum variation purposive sampling strategy to maximise diversity across demographic and clinical characteristics. Reference Palinkas, Horwitz and Green21
All 108 parents in the larger study, which included several bereaved parents, were emailed an announcement about the current study, which linked directly to an electronic consent form and online questionnaires in Research Electronic Data Capture (REDCap). Reference Harris, Taylor and Thielke22 The questionnaires could be completed within 20–25 minutes via computer, tablet, or smartphone. The decision to include bereaved parents was based on prior research indicating that post-traumatic stress and post-traumatic growth are salient in this population. Reference Albuquerque, Narciso and Pereira23,Reference Suttle, Hall and Pollack24 Participants were paid $15 upon completion of the questionnaires and were given the option to receive written feedback on parental post-traumatic stress symptoms, and for parents of surviving children with CHD, feedback on child emotional/behavioural problems (i.e., no concerns/at-risk/clinically significant) along with a list of related clinical resources. This study was approved by the Institutional Review Board, with a waiver of written documentation of informed consent to allow for an electronic consent process. A stakeholder advisory council consisting of four parents of a child with CHD and six medical and mental health providers advised on study methodology.
Measures
Demographic and medical information
Parents reported demographic and medical information via a REDCap survey upon initial enrollment in the larger study of family-based psychosocial care, including parent gender, race, ethnicity, and education level, family income and geographic area (i.e., urban, suburban, rural); and parent-reported child age, CHD diagnoses, genetic diagnoses, treatment history, and history of medical complications and developmental delay.
Parental post-traumatic stress symptoms
Parents responded to a modified introductory question (i.e., “Before we get started, it would be helpful for us to know the most upsetting or traumatic events you experienced related to your child’s CHD. Please list or briefly describe the events.”) from the Posttraumatic Stress Disorders Checklist for Diagnostic and Statistical Manual of Mental Disorder – Fifth Edition. Reference Weathers, Litz and Keane25 They then rated 20 questions based on how much they have been bothered by symptoms spanning the 4 post-traumatic stress disorder symptom clusters (i.e., intrusion, avoidance of trauma reminders, negative alterations in thoughts/feelings, altered physiological arousal/reactivity) 26 in the past month on a scale of 0 (Not at all) to 4 (Extremely). Responses yield a total symptom severity score ranging from 0 to 80, with higher scores indicate greater post-traumatic stress symptom severity. Further, to determine whether respondents reported a constellation of symptoms consistent with a diagnosis of post-traumatic stress disorder, 26 each item response was categorised as endorsed if rated “moderate” or higher, as per scoring guidelines. Reference Weathers, Litz and Keane25 Respondents endorsing at least one symptom of intrusion, one symptom of avoidance, two symptoms of negative alterations in thoughts/feelings, and two symptoms of arousal were considered to have fulfilled the criteria. This measure has previously demonstrated good test–retest reliability and adequate convergent, discriminative, and construct validity. Reference Blevins, Weathers and Davis27 Within the current sample, this instrument demonstrated high internal consistency for the total symptom severity score (α = .94), and acceptable to good internal consistency for each of the symptom clusters, intrusion (α = .85), avoidance (α = .74), negative thoughts/feelings (α = .87), and arousal/reactivity (α = .85).
Parental post-traumatic growth
Parental post-traumatic growth was assessed through the 10-item Post-Traumatic Growth Inventory – Short Form. Reference Cann, Calhoun and Tedeschi28 Participants were instructed to indicate the degree to which they experienced positive changes (e.g., “I have a greater sense of closeness with others” and “I discovered that I am stronger than I thought I was”) as a result of their upsetting or traumatic CHD experiences on a Likert-type scale ranging from 0 (Not at all) to 5 (A very great degree). Possible scores ranged from 0 to 50, with higher scores indicating greater post-traumatic growth. This adaptation of the original 21-item Post-Traumatic Growth Inventory has been found to have the same factor structure as the original and good convergent validity. Reference Cann, Calhoun and Tedeschi28 The Post-Traumatic Growth Inventory – Short Form demonstrated good internal consistency for the total score in the current sample (α = .80).
Overprotective parenting
Parents of a surviving child with CHD aged 4 years and older completed the 10-item Overprotective Parenting Subscale of the Comprehensive General Parenting Questionnaire. Reference Sleddens, O’Connor and Watson29 Items on this subscale (e.g., “I always help my child with everything he/she does”) are rated on a 5-point Likert type scale ranging from 1 (Strongly disagree) to 5 (Strongly agree), for a total score range of 10–50. Parents of a surviving child with CHD less than 4 years of age completed the 7-item Overprotective Parenting Subscale from the toddler version of the Comprehensive General Parenting Questionnaire, with possible total scores ranging from 7 to 35. Reference van der Horst and Sleddens30 Higher scores on both measures indicate more overprotective parenting. Total scores were divided by the number of items to produce comparable scales across age ranges. These measures showed adequate internal consistency in this sample (α = 76 for aged 4 and over and α = .71 for the toddler version).
Child emotional and behavioural problems
Parents of a surviving child with CHD completed the first 17 items of the Pediatric Emotional Distress Scale, Reference Saylor, Swenson and Stokes Reynolds31 designed to capture emotional and behavioural problems in young children exposed to trauma. This measure, standardised on children aged 2–10, produces a total score and three subscales with established clinical cut-offs: Anxious/Withdrawn, Acting Out, and Fearful. Parents rated their child’s experience of problems on a 4-point Likert-type scale ranging from 1 (Almost Never) to 4 (Very Often). This measure has satisfactory test–retest reliability and inter-rater reliability. Reference Saylor, Swenson and Stokes Reynolds31 Internal consistency for the total scale was good in the current sample (α = .85), and individual subscales demonstrated adequate internal consistency (Anxious α = .71, Fearful α = .68, Acting Out α = .77).
Analysis
All analyses were conducted using the Statistical Package for the Social Sciences Version 24. 32 The first author categorised the most upsetting or traumatic CHD experiences reported by parents on the Post-Traumatic Stress Disorder Checklist for the Diagnostic and Statistical Manual of Mental Disorder – Fifth Edition into broad themes and the proportion of parents reporting each theme were calculated. Four parents with children 4 years and older did not respond to one item on the overprotective parenting measure, and two of those did not respond to another item on that scale, both pertaining to their child having play dates. Since they answered the remaining items on the measure, the subscale means for existing data were used to replace the participants’ missing data on these two questions. Descriptive statistics were computed for scale score totals and demographic variables. Pearson correlational analyses were used to examine hypothesis 1 (i.e., parental post-traumatic stress symptom severity would be positively associated with overprotective parenting and child emotional/behavioural problems) and hypothesis 2 (i.e., overprotective parenting would be positively associated with child emotional/behavioural problems). Additional exploratory Pearson correlational analyses and t-tests were completed to examine patterns of relationships between post-traumatic growth, parent and child demographic variables, and the primary variables of interest. Hypothesis 3 (i.e., overprotective parenting would mediate the relationship between parental post-traumatic stress symptom severity and child emotional/behavioural problems) was examined through mediation analysis with ordinary least squares path analysis with bootstrapping using Process Macro Reference Hayes and Little33 in the Statistical Package for the Social Sciences. Mean-centred scores were used in the mediation model, and 10,000 bootstrap samples were used to calculate 95% confidence intervals for direct and indirect effects.
Results
Parent participant and child characteristics
Of 108 invited parents, 73 (68%) read the study description and completed at least one field of the REDCap survey (e.g., indicated an interest in reviewing the electronic consent form), 68 (63%) provided electronic consent, and 60 (56%) (45 mothers, 15 fathers) participated in the study (see Table 1). Children of participating parents ranged from 1 to 6 years old (M = 3.79 SD = 1.43), and most had open-heart surgery in the first month of life (75%; Table 2). Over half of these children had parent-reported developmental delays (55%) and experienced medical complications (55%) including cardiac arrest/need for CPR (30.0%), extracorporeal membrane oxygenation (20%), stroke (13.3%), and requiring a feeding tube at discharge (48.3%). Participating parents were more likely to be college educated (81.7% versus 56.3%, χ 2(1) = 8.26, p < .01) and more likely to have received a prenatal CHD diagnosis (55.0% versus 34.3%, χ 2(1) = 6.92, p < .01) than were non-participant. There were no other significant differences between those who did and did not participate.
Table 1. Parent characteristics

N = 108 for larger study. N = 60 for current study. aN = 58. Parent age ranged from 22 to 47 (larger study) and 22 to 44 years (current study).
Table 2. Child characteristics

N = 108 for original study. N = 60 for current study. Child age ranged from 1 to 6 years.
Traumatic events
On average, participants listed roughly three different “most upsetting or traumatic events” related to their child’s CHD (Mean = 2.93, Median = 2, SD = 2.78, Range = 1–16; see Table 3). The most frequently listed events were initial diagnosis (n = 21, 35%); child arresting and requiring resuscitation (n = 17; 28%); medical complications (n = 15; 25%); difficult procedures such as extracorporeal membrane oxygenation, intubation, and multiple needle sticks (n = 10; 17%); and hospital/intensive care admissions that were lengthy, unexpected, or frequent (n = 9; 15%).
Table 3. Most upsetting/traumatic CHD-related events

N = 60. CHD = congenital heart disease. Themes endorsed by more than one parent were included.
Rates of parental post-traumatic stress symptoms, post-traumatic growth, and child emotional/behavioural problems
Many parents reported post-traumatic stress symptoms related to their CHD experiences, with 70% (n = 42) meeting clinical criteria for the symptom cluster of intrusion. For each of the other three symptom clusters, 42% (n = 25) met the clinical criteria. Eighteen per cent of parents (n = 11) met the full criteria for post-traumatic stress disorder (see Table 4). On average, parents reported experiencing post-traumatic growth between a moderate and great degree related to their CHD experiences (M = 31.71, SD = 8.81, Range = 5–48). Mothers (M = 33.18, SD = 7.98) reported higher rates of post-traumatic growth than did fathers (M = 27.4, SD = 9.96) (t(57) = −2.27, p = .03). Bereaved parents and parents of living children did not differ on post-traumatic stress nor post-traumatic growth. Parents reported considerable child emotional and behavioural problems, with roughly half endorsing clinically significant problems with child Acting Out (n = 25, 48%), Anxious/Withdrawn behaviour (n = 33, 63%), and Fearfulness (n = 28, 54%). Overall, more than three quarters (n = 42, 81%) of parents reported clinically significant emotional/behavioural concerns in their children (i.e., Pediatric Emotional Distress Scale total score).
Table 4. Questionnaire data
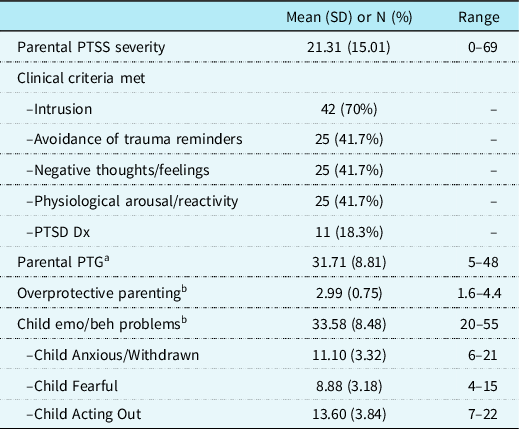
N = 60. aN = 59. bN = 52. Parental PTSS severity = PTSD checklist for DSM-5 (PCL-5) total score. Clinical Criteria Met = each symptom cluster met the criteria based on the PCL-5 scoring guidelines. PTSD Dx = met the clinical criteria for post-traumatic stress disorder based on the PCL-5 scoring guidelines. Parental PTG = Post-Traumatic Growth Inventory – Short Form total score. Overprotective Parenting = combined mean score (5-point Likert scale) from age-appropriate version of the overprotective subscale on the Comprehensive General Parenting Questionnaire. Child emo/beh problems = Pediatric Emotional Distress Scale total score and subscale total scores (clinical cut-offs: Anxious/Withdrawn >9.5; Fearful >8.5; Acting Out >13.5; Total>27.5).
Correlates of parental post-traumatic stress symptoms, overprotective parenting, and child emotional/behavioural problems
Consistent with our hypotheses, parental post-traumatic stress symptom severity was associated with overprotective parenting (r = .37, p = .008) and child emotional/behavioural problems (r = .29, p = .037; see Table 5); and overprotective parenting was associated with child emotional/behavioural problems (r = .45, p = .001) and with child age (r = .33, p = .018). Child age was correlated with child emotional/behavioural problems (r = .31, p = .024) and was included as a covariate in the mediation testing. Overprotective parenting and child emotional/behavioural problems were not associated with prenatal diagnosis or parent-reported child medical complications or developmental delay. Parental post-traumatic stress symptom severity was negatively correlated with income (r = −.27, p = .041), but not with either medical complications or developmental delays. Exploratory analyses revealed significant associations between parental post-traumatic growth and the post-traumatic stress symptoms symptom cluster of intrusion (r = .32, p = .013). There were no associations between parental post-traumatic growth and any other parent or child characteristics, including overprotective parenting and child emotional/behavioural problems. Therefore, parental post-traumatic growth was not included in further analyses.
Table 5. Correlations amongst variables of interest and covariates

N = 51–60 with pairwise deletion. **p < .01. *p < .05. Child emo/beh problems = Pediatric Emotional Distress Scale mean score. Parental PTSS = PTSD checklist for DSM-5 mean score. Parental PTG = Post-Traumatic Growth Inventory – Short Form mean score. Overprotective Parenting = combined mean score (5-point Likert scale) from age-appropriate version of the overprotective subscale on the Comprehensive General Parenting Questionnaire.
Overprotective parenting as a mediator between parental post-traumatic stress symptoms and child emotional/behavioural problems
Mediation analysis using ordinary least squares path analysis, controlling for child age, revealed that overprotective parenting significantly mediated the relationship between parental post-traumatic stress symptoms and child emotional/behavioural problems (See Table 6 and Fig 1). The total effect of parental post-traumatic stress symptoms on child emotional/behavioural problems was significant (b c = .18; p = .03). Path a, the relationship between parental post-traumatic stress symptoms and overprotective parenting, was likewise statistically significant (b a = .34, p = .006). Path b, the relationship between overprotective parenting and child emotional/behavioural problems when controlling for parental post-traumatic stress symptoms, was also significant (b b = .21; p = .03). The indirect effect of parental post-traumatic stress symptoms on child emotional/behavioural problems through the pathway mediated by overprotective parenting was statistically significant (b ab = .11; 95% CI = .01 – .25). Finally, there was no significant direct effect of parental post-traumatic stress symptoms on child emotional/behavioural problems when overprotective parenting was in the model (b c’ = .11; p = .22), suggesting full mediation. In other words, controlling for child age, the relationship between parental post-traumatic stress symptoms and child emotional/behavioural problems was fully accounted for by overprotective parenting.
Table 6. Multiple regression analysis testing mediation of overprotective parenting on relationship between parental PTSS and child emotional/behavioural problems

N = 52. *p < .05. **p < .01. Coefficient = unstandardised beta weight for scale means. Parental PTSS = PTSD checklist for DSM-5 total score. Child emo/beh problems = Pediatric Emotional Distress Scale total score. Overprotective parenting = Overprotective composite from the toddler and original items from the Comprehensive General Parenting Questionnaire mean scores.

Figure 1. Mediation of overprotective parenting on the relationship between parental PTSS and child emotional/behavioural problems.
N = 52. *p < .05. **p < .01. PTSS = post-traumatic stress symptoms. Child age was included as a covariate in the model. a = total effect of parental PTSS on overprotective parenting. b = total effect of overprotective parenting on child emotional/behavioural problems, controlling for parental PTSS. ab = completely standardised indirect effect of parental PTSS on child emotional/behavioural problems. c = total effect of parental PTSS on child emotional/behavioural problems (sum of direct and indirect effects). c’ = direct effect of parental PTSS on child emotional/behavioural problems.
Discussion
Parental post-traumatic stress symptoms are associated with greater emotional and behavioural problems in children with critical CHD, and this association appears to be mediated by overprotective parenting. There were high rates of concern regarding child emotional and behavioural problems amongst parents in this sample, with the mean score above the clinical cut-off for all three subscales and the total score. Critical CHD places children at risk for multiple medical and neurodevelopmental challenges. In addition, they face roughly seven times the risk for anxiety and/or depression compared to children without CHD. Reference Gonzalez, Kimbro and Cutitta34 Parental post-traumatic stress and overprotective parenting may contribute to this increased risk. While emerging research highlights the high prevalence of post-traumatic stress symptoms amongst parents of children with CHD Reference Woolf-King, Anger and Arnold3 and its negative associations with child psychosocial functioning and quality of life, Reference DeMaso, Labella and Taylor5,Reference Ernst, Marino and Cassedy6 potential mechanisms underlying these relationships have not been previously identified. These findings build upon research suggesting that parents of children with CHD may perceive their child to be more vulnerable than parents of healthy children Reference Vrijmoet-Wiersma, Ottenkamp and van Roozendaal10 and may exhibit greater parenting vigilance. Reference Meakins, Ray and Hegadoren9,Reference Rempel and Harrison11
Both parental post-traumatic stress symptoms and overprotective parenting are modifiable risk factors for poor child outcomes. Family-based psychosocial prevention and intervention strategies for parents of children experiencing other medical condition, including cancer and preterm birth, have been shown to reduce parental post-traumatic stress symptoms. Reference Kazak, Alderfer and Streisand35,Reference Jotzo and Poets36 Within the CHD literature, there is emerging evidence to support parental mental health interventions targeting maternal anxiety, parenting confidence, parenting satisfaction, and parent–infant interaction. Reference Kasparian, Kan and Sood37 However, existing prevention and intervention programmes for parents of children with CHD have not specifically targeted parental post-traumatic stress symptoms or overprotective parenting. Parents of children with CHD sometimes receive conflicting advice from medical professionals (e.g., “Treat her like a normal kid,” and “She might be back in the hospital if she gets a cold”) and are not often provided with formal support in navigating the challenges of parenting a medically complex child. Such supports could include parenting classes or individual meetings with an expert on child development and parenting, addressing parents’ fears for their child’s health while encouraging appropriate independence, and formalised peer-to-peer support from parents who have experienced challenges in parenting children with CHD firsthand. Routine screening for beliefs related to child vulnerability, overprotective parenting, and parent post-traumatic stress symptoms may also be helpful in identifying families in need of more formal parenting or psychosocial supports.
Parents in this study reported high rates of clinically significant post-traumatic stress symptoms, with mothers reporting more symptoms than fathers, consistent with other literature. Reference Wray, Cassedy and Ernst4 This level of continuing distress suggests that without treatment, these symptoms persist well beyond the initial surgeries. In fact, the rates of post-traumatic stress disorder (18%) amongst this sample were similar to that of parents 4 months after discharge from surgical admissions. Reference Medoff-Cooper, Marino and Fleck38 Although post-traumatic stress symptoms and post-traumatic stress disorder require just one criterion event, parents reported numerous traumatic events related to their child’s CHD, consistent with a pattern of prolonged, repeated experience of paediatric medical trauma that is known to increase parents’ symptom complexity and vulnerability to further traumatisation. Reference Boman, Kjällander and Eksborg39 The experience of receiving the initial diagnosis was perceived as traumatic by 35% of parents, suggesting that trauma and parental post-traumatic stress symptoms may begin even before the child’s birth. The fear that their child would die was reported as one of the most traumatic CHD events for 15% of parents. This fear is more predictive of parental post-traumatic stress symptoms than objective measures of disease severity and life threat. Reference Nelson and Gold40 In our sample, there were no associations with the type of medical or developmental complication and post-traumatic stress symptoms. Whereas other paediatric illnesses may be diagnosed after the parent–child relationship has been well established, for families of a child with critical CHD, the parent–child relationship and parenting practices may develop within the context of ongoing paediatric medical trauma beginning at or before birth. Trauma experienced during a level 2 ultrasound with an obstetrician, prior to initial contact with the paediatric cardiac team, may not be immediately recognised by cardiac social workers, psychologists, or other psychosocial team members who are likely to focus on traumas occurring later within the hospital setting. Therefore, this important experience of trauma may go unnoticed, representing a missed opportunity to provide parents with psychosocial support to prevent or reduce post-traumatic stress symptoms.
Parental post-traumatic growth (post-traumatic growth) was positively associated with the report of intrusive symptoms but no other post-traumatic stress symptoms symptom clusters. Parents with greater intrusive symptoms likely engage repeatedly with the trauma, attempting to put it into perspective. These types of psychological struggles are theorised to be necessary for the development of post-traumatic growth, Reference Tedeschi and Calhoun15 with ongoing traumatic distress acting as a precursor and often co-occurring with post-traumatic growth. In this study, parental post-traumatic growth was not associated with overprotective parenting, child emotional/behavioural problems, or any cardiac characteristics or complications. Prior research has indicated that parent and child post-traumatic growth may be related, Reference Bernstein and Pfefferbaum17 but no study to our knowledge has measured the relationship between parental post-traumatic growth and child emotional and behavioural problems. Future studies should more closely examine the relationship between parental post-traumatic growth and parent and child outcomes in the context of paediatric illness and CHD. Mothers reported higher levels of post-traumatic growth than did fathers, consistent with prior research. Reference Boman, Kjällander and Eksborg39,Reference Vishnevsky, Cann and Calhoun41 Men and women likely process and cope with trauma differently, and prevention and intervention strategies should be tailored to the unique needs of CHD mothers and fathers.
The results of this cross-sectional study should be considered within the context of methodological limitations. Parents reported at a single point in time, therefore, causality cannot be confirmed. Furthermore, the current model does not account for pre-existing mental health of the parent, which could influence both post-traumatic stress symptoms and parenting. In addition, parents were recruited as individuals with the potential for inclusion of two parents reporting on their perspectives about the same child. Roughly half of the children with CHD experienced medical complications. It is possible that reported rates of parental post-traumatic stress symptoms or child emotional/behavioural problems may be higher than would be observed in the broader population of families of children with critical CHD.
Reducing the impact of social determinants of health and mental health is a national priority. 42,Reference Garner, Shonkoff and Siegel43 Participants in this study were English-speaking parents with a reliable smartphone or Internet access, and with many holding multiple positions of privilege. These findings may not generalise to a more diverse sample of families who are subjected to oppression and discrimination and the expected consequences, including increased trauma exposure, toxic stress, and poverty [e.g., Reference Kirkinis, Pieterse and Martin44,Reference Malawa, Gaarde and Spellen45 ]. These social determinants of health also increase the risk of poor medical and neurodevelopmental outcomes for children with CHD, Reference Davey, Sinha and Lee46 yet this population is significantly underrepresented in health research. Reference Oh, Galanter and Thakur47
While this study represents an important first step in a highly understudied area of investigation, longitudinal research using multiple methods of measuring constructs is needed to further our understanding of the relationships between parental post-traumatic stress symptoms, post-traumatic growth, parenting, and child neurodevelopmental and psychosocial outcomes amongst all families affected by CHD. Inclusion and retention of underrepresentation groups, including racial/ethnic minorities and low SES families are imperative. Research teams should invest in long term relationships with these communities, partnering with parent collaborators and other key stakeholders from underrepresented communities in every stage of the research process. Reference Bartlett, Chiarello and Hjorngaard48
In conclusion, this study highlights the urgent need for supports to prevent or reduce parental post-traumatic stress symptoms and to promote effective parenting following a child’s diagnosis of CHD. Protective factors that reduce the risk for post-traumatic stress symptoms following a diagnosis of CHD and mitigate the impact of post-traumatic stress symptoms on parenting should be identified and supports to promote these factors should be incorporated into prevention and intervention programmes.
Acknowledgements
The authors would like to thank the parents who participated in this study and shared their experiences with us. We feel honoured to help tell their story.
Financial support
This project was supported by an Institutional Development Award from the National Institute of General Medical Sciences of the National Institutes of Health under grant number U54-GM104941 (PI: Binder-Macleod).
Conflicts of interest
No conflicts of interest were declared.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the United States Federal Policy for the Protection of Human Subjects, 45 CFR part 46 and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by and was conducted in accordance with the regulations of the Institutional Review Board at Nemours/A.I. duPont Hospital for Children.
Informed consent
All participants provided electronic informed consent and had an opportunity to get all questions answered by the research team prior to their participation.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
All co-authors participated in a meaningful way in the preparation of the manuscript (in the design/conceptualisation of the study, interpretation of data, or drafting manuscript). The data analysis was completed by Linda G. McWhorter and Aimee K. Hildenbrand. The initial draft of the manuscript was written by Linda G. McWhorter. All authors commented on previous versions and have read/approved this manuscript. The principal and corresponding authors have full access to the data and the right to publish such data.










