Introduction
Tonsillectomy is one of the commonest surgical procedures performed in the UK, with over 45 000 performed in England in 2018–2019.1 The procedure accounts for 17 per cent of the total elective surgical workload of ENT departments across the UK and almost 8 per cent of their total budgets.Reference Marshall2
Indications for tonsillectomy include recurrent acute tonsillitis, obstructive sleep apnoea (OSA), peritonsillar abscess and diagnostic purposes. Post-operative complications include infection, pain and bleeding and can often necessitate readmission to hospital. The recent Getting It Right First Time review of tonsil surgery in the UK found that up to 18.4 per cent of all adult and 9.4 per cent of all paediatric tonsillectomy patients were readmitted to hospital based on Health Episode Statistic data.Reference Marshall2 Haemorrhage was the commonest reason for readmission in both adults (13.0 per cent) and children (5.7 per cent), and infection, pain, nausea and vomiting accounted for readmission in 2.2 per cent of adults and 1.6 per cent of children. Based on these results, the Getting It Right First Time review recommended that hospitals adopt standard patient information that provides clear post-operative information on expected recovery and instructions for managing early signs of complications in an effort to reduce readmission rates.
The advice given to patients post-tonsillectomy is known to vary between countries, hospitals and surgeons, especially with regards to diet.Reference Setabutr, Adil, Adil and Carr3 Many surgeons have favoured recommending soft and cold foods post-operatively in order to maximise good oral intake and patient satisfaction, whereas others have favoured dry foods such as toast, which has anecdotally been thought to enhance the healing of the operative site.Reference Millington, Gaunt and Phillips4 These differing opinions are partially because of the lack of high-quality studies on the subject and a subsequent over-reliance on expert opinion. A cohesive, national approach to reducing readmissions following tonsillectomy is required; as such, an awareness and critical examination of the current practice of UK hospitals in providing advice to patients following tonsillectomy is necessary.
In this paper, the first of its kind in the UK, we analysed the advice sheets given to patients from 110 National Health Service (NHS) trusts across the UK and compared the advice being given with that of published evidence on the subject. Based on this, we also aimed to make suggestions as to what information should be included in a ‘gold standard’ post-tonsillectomy advice sheet based on available published evidence.
Materials and methods
Freedom of information requests were submitted to 148 UK NHS trusts and equivalent organisations (referred to as ‘hospitals’ in this paper) between December 2019 and March 2020 enquiring as to whether they routinely performed tonsillectomy on adults or children (Appendix 1). A total of 129 hospitals responded, of which 110 were regularly performing tonsillectomy procedures. Copies of tonsillectomy patient advice sheets provided by these hospitals were requested. As most hospitals provided separate advice sheets for adult and paediatric patients, a total of 143 unique advice sheets were received from 110 hospitals.
Each advice sheet from each hospital was analysed separately. The collated advice sheets were then grouped into advice given to adults and advice given to children. If a hospital provided more than one advice sheet to adults or children, the advice within both was combined, even if the advice was opposing, to create a unique ‘advice profile’ for adults and children for each hospital. Advice was thematically categorised under four headings: ‘post-operative diet and fluid intake’, ‘general post-operative management’, ‘general post-operative risks’ and ‘bleeding’. Once all the thematic categories of advice had been established and filled, the leaflets were re-analysed to ensure no pertinent information was missed.
Limitations of this study
Trusts who did not initially respond were recontacted on two occasions over the course of six months. Because of the limitations of freedom of information requests, only generic advice sheets were obtained, and we acknowledge that clinicians may have informed the patients about tonsillectomy procedures through other means, such as consultations and the consent process.
Results
Of the 110 hospitals that performed tonsillectomy procedures, 104 performed adult tonsillectomy procedures and 106 performed paediatric tonsillectomy procedures. Of those performing paediatric tonsillectomy procedures, 88 hospitals (83 per cent) provided separate advice sheets for children. In total, 143 distinct post-tonsillectomy advice sheets were analysed. Sixty hospitals provided one or more of their own leaflets on tonsillectomy procedures (total number n = 139), 41 hospitals provided leaflets from ENT UK only5 and 18 hospitals provided leaflets from EIDO Healthcare only.6 On average, each hospital provided 2 patient information leaflets (range, 1–8). Nineteen hospitals provided patients with a combination of their own hospital leaflets plus ENT UK (16 hospitals) or EIDO healthcare (4 hospitals) leaflets.
Post-operative diet and fluid intake
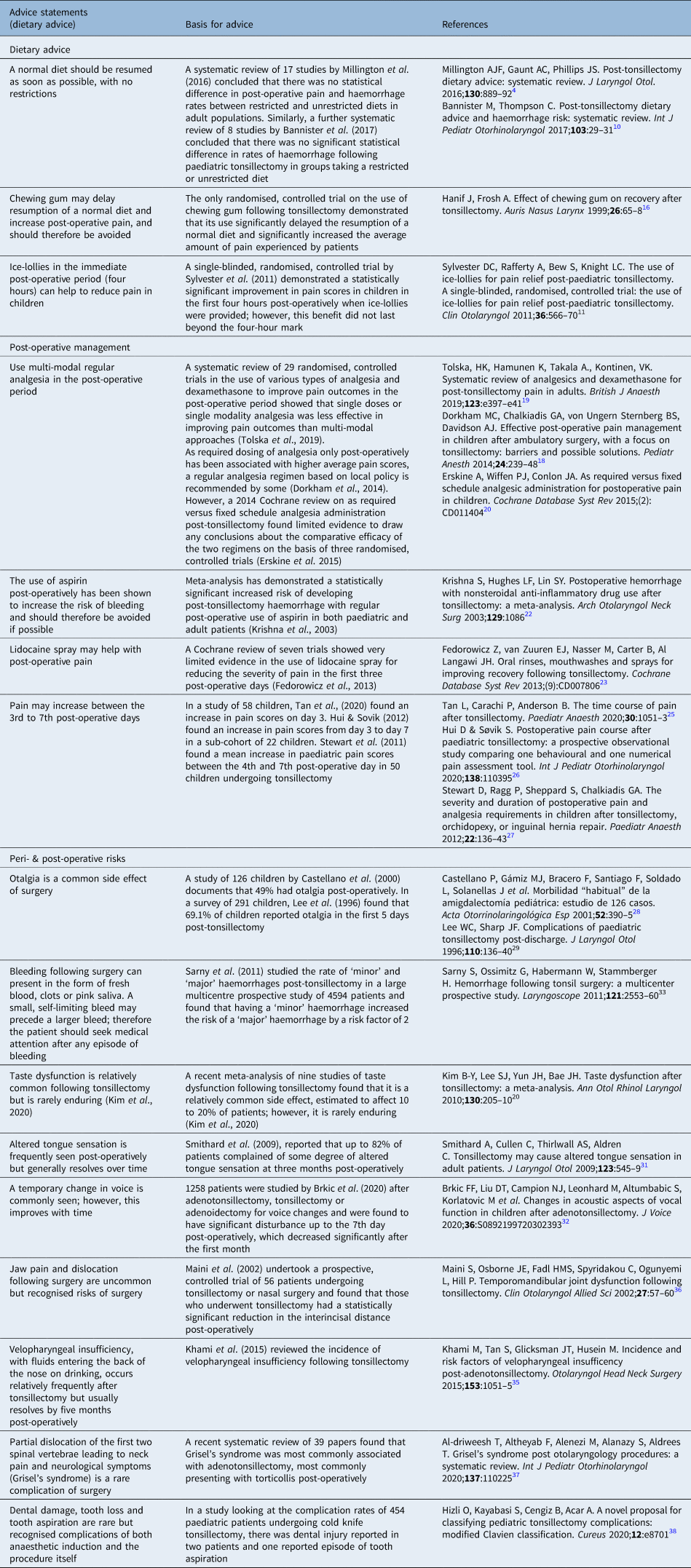
Within the 143 distinct advice sheets analysed, dietary intake was the most commonly mentioned topic of advice (95 per cent). Six discrete and differing advice statements on post-operative diet and four on fluid intake were identified (Figure 1). Eighty-five per cent of hospitals recommended regularly eating and drinking a normal diet to both adults and children. Twenty-six per cent of hospitals recommended eating ‘hard’ foods and 8 per cent recommended that ‘soft’ foods should preferentially be consumed. Nearly 52 per cent of hospitals recommended using chewing gum to adults post-operatively and 39 per cent to children. Many hospitals recommended that adults drink ‘plenty’ of fluids (75 per cent), but comparatively this advice was relatively lacking in the advice sheets for children (25 per cent). Many hospitals also recommended that adults should ‘avoid fizzy drinks’ (21 per cent) and ‘citrus or fruit juices’ (9 per cent) in the post-operative period without any explanation for this advice.
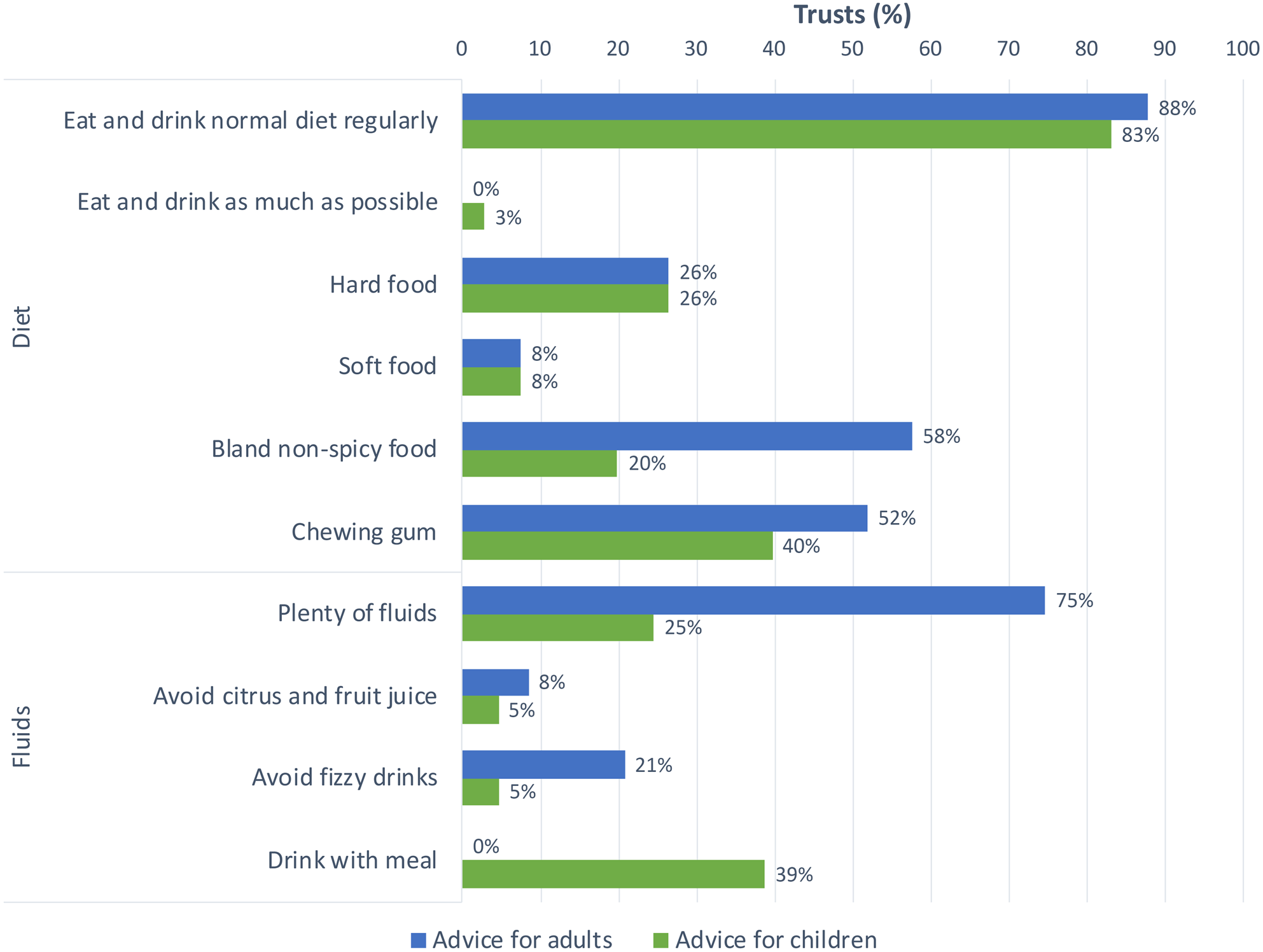
Fig. 1. Frequency of post-operative dietary and fluid-intake advice given by hospitals.
General post-operative management
Any advice that did not pertain to diet, fluid intake or specific risks within the first two weeks of the post-operative period was grouped under the heading of ‘general post-operative advice’ (Figure 2). Most hospitals recommended taking oral painkillers regularly in the post-operative period (87 per cent for adults and 81 per cent for children), whereas only 7 per cent of hospitals recommended using topical analgesic sprays such as DifflamTM. Specific advice regarding which analgesics to use (i.e. ‘regular paracetamol and ibuprofen’) and to avoid (i.e. ‘avoid aspirin’) was given to children by 39 per cent and 51 per cent of hospitals, respectively, whereas no hospital provided such advice to adults (0 per cent). Most hospitals also recommended that adults (79 per cent) and children (84 per cent) should take two weeks off work or school following the operation, although the specific reasoning behind this advice was not explained.

Fig. 2. Non-dietary post-operative management advice.
General post-operative risks
Post-operative risks and complications mentioned in leaflets could be broadly grouped into three categories: pain, visual and sensory changes, and bleeding (Figure 3). Referred otalgia was mentioned as a risk to adults and children by 74 per cent and 63 per cent of hospitals, respectively. By contrast, relatively few hospitals mentioned the fact that pain could be expected to worsen over the first post-operative week (21 per cent for adults, 15 per cent for children). Other advice commonly mentioned to both adults and children included the post-operative risk of ‘bad breath’ (40 per cent for adults, 50 per cent for children) and a ‘white appearance of the throat’ (59 per cent for adults, 53 per cent for children). The risk of post-operative nausea was more likely to be mentioned in advice for children (48 per cent) than adults (5 per cent), although conversely the risk of voice change was mentioned more frequently to adults (21 per cent) than children (3 per cent).

Fig. 3. Post-operative risks mentioned in patient information leaflets.
Bleeding
The majority of hospitals recommended that patients should seek medical attention if they experienced any bleeding (71 per cent for adults, 71 per cent for children). However, some hospitals qualified this statement by advising that only ‘continued’ bleeding should necessitate medical review (17 per cent for adults, 17 per cent for children). Some went further and suggested that ‘bleeding of up to a spoonful’ is normal and should not prompt the patient to seek medical attention (11 per cent for adults, 12 per cent for children).
Discussion
The overall picture of post-tonsillectomy advice being given to patients around the UK is mixed. Although there is much consensus, there are also many areas of contrasting and conflicting guidance. We reviewed the published literature pertaining to our four identified thematic domains and compared this to the advice contained within analysed information leaflets. Following on from this, we were able to synthesise evidence-based patient information leaflet statements (Appendix 2).
Dietary Advice
The majority of hospitals recommended returning to a normal diet in the post-operative period (88 per cent for adults, 83 per cent for children); however, 26 per cent also suggested preferentially eating hard foods (such as dry toast) and 8 per cent suggested soft foods. The reasoning behind this advice was explained in some of the leaflets: hard, dry foods were said to ‘keep the healing area where the tonsils were clean’ by ‘removing dead tissue’. Similarly, cold and soft foods were said to ‘reduce pain, increase dietary intake and reduce the risk of post-operative bleeding’.7 This advice was unreferenced within the information sheets.
• Many UK hospitals provide varying advice on post-tonsillectomy care, but much of this advice is anecdotal
• Restricted diets are not shown to have benefit in post-tonsillectomy, and early resumption of a normal diet is recommended
• Use of multi-modal analgesia post-operatively has been shown to have the greatest benefit in terms of pain management
• Risks such as otalgia and change in taste should be mentioned more in leaflets
• Minor haemorrhages can lead to larger bleeds post-operatively, and this should be made clear
• Evidence-based post-tonsillectomy advice has been summarised in a patient advice sheet for dissemination
This differing of opinion on preferential or restricted diets is reflected within the published literature. Setabutr et al. (2011) questioned 793 US otolaryngologists on the post-operative dietary advice they routinely gave; 59 per cent of respondents recommended a soft diet and 35 per cent an unrestricted diet.Reference Setabutr, Adil, Adil and Carr3 It is known that children will preferentially choose a soft or liquid diet in the post-tonsillectomy period when given the choice; however, further than this, most post-tonsillectomy dietary advice seems to be based on historical anecdotes.Reference Thomas, Moore and Reilly8,Reference Idvall, Holm and Runeson9 A systematic review of 17 studies by Millington et al. (2016) concluded that there was no statistical difference in post-operative pain or haemorrhage rates between restricted and unrestricted diets in adult populations.Reference Millington, Gaunt and Phillips4 Similar conclusions were drawn in a systematic review of eight studies by Bannister and Thompson (2017) in paediatric groups.Reference Bannister and Thompson10 However, it is important to note, as recognised by Millington et al. (2016), that most of the included studies in these reviews were generally of poor quality, with small sample sizes and inappropriately powered and non-randomised studies, meaning drawing conclusions was difficult.
Although restricted diets do not appear to confer any benefit, there is some evidence that additives to diets can reduce post-operative morbidity. A small-scale study by Sylvester et al. (2011) demonstrated statistically significant improved pain scores in children in the first four hours post-operatively when ice-lollies were provided; however, this benefit did not appear to last beyond the four-hour mark.Reference Sylvester, Rafferty, Bew and Knight11
Dietary supplements
The addition of honey to the post-operative diet has been suggested as beneficial in reducing pain and analgesia use. A 2014 meta-analysis concluded that its use following tonsillectomy may have such positive effects, but it was on the basis of four small-scale heterogeneous studies only.Reference Hwang, Song, Jeong, Lee and Kang12 However, a more recent Cochrane review on the effects of honey on wound healing has concluded that the ‘evidence for differences in the effects of honey and its comparators is of low or very low quality and does not form a robust basis for decision making’.Reference Jull, Cullum, Dumville, Westby, Deshpande and Walker13
The use of chewing gum post-operatively was widely recommended to both adults (52 per cent of hospitals) and children (40 per cent of hospitals) in the leaflets analysed. However, this recommendation appears to be largely based on historical anecdotal observations. In 1982, Maurice Schiff commented on the beneficial use of bubble gum in reducing post-operative pain: the ‘increased deglutition effort’ being said to ‘permit the milking out of lymphatics even better than chewing gum’.Reference Shiff14 The only published study with a positive finding was that of an observational audit in 1997 that demonstrated a moderate reduction in the number of general practitioner consultations by patients following tonsillectomy after the use of chewing gum was encouraged and added to post-operative instructions.Reference Jones, Temple, Morar, Roland and Rogers15 However, the observational nature and lack of any objective patient morbidity or adherence scores make it impossible to draw any meaningful conclusions from this study in isolation. The only prospective randomised, controlled trial on the use of chewing gum following tonsillectomy demonstrated that its use significantly delayed the resumption of a normal diet and significantly increased the average amount of pain experienced by patients.Reference Hanif and Frosh16 On the basis of this study alone, the use of chewing gum should be discouraged in the immediate post-operative period.
General post-operative management
Following tonsillectomy, 79 per cent of hospitals suggested 2 weeks off work for adults, and 84 per cent suggested 2 weeks off school for children (Figure 2). Many of the leaflets suggested that being around others at work or at school in the post-operative period resulted in an increased risk of infection. The Getting It Right First Time analysis found that 1.1 per cent of adults and children were re-admitted to hospital post-tonsillectomy with ‘infection’Reference Marshall2; however, the underlying risk factors for developing such a post-operative infection have not been well categorised in the literature. More research in this domain could be valuable, as 14 days off work or school can represent a significant drawback to undergoing tonsillectomy for patients who find it difficult to take the required time off work or off school during term-time.
Post-operative analgesia
Most hospitals recommended the use of ‘regular painkillers’ to both adults (87 per cent) and children (81 per cent). Although there is no strong evidence for any one particular regimen of medication over another in the literature, many studies report better post-operative pain control with a multi-modal analgesic approach in both adults and children.Reference Aldamluji, Burgess, Pogatzki-Zahn, Raeder and Beloeil17–Reference Tolska19 As required dosing of analgesia post-operatively has been associated with higher average pain scores, a regular analgesia regimen based on local policy is recommended by some.Reference Dorkham, Chalkiadis, von Ungern Sternberg and Davidson18 However, these conclusions are drawn from relatively small scale studies, which suffer from a lack of randomisation. A 2015 Cochrane review on as required versus fixed schedule analgesia administration post-tonsillectomy found limited evidence to draw any conclusions about the comparative efficacy of the two regimens on the basis of three randomised, controlled trials.Reference Erskine, Wiffen and Conlon20
Avoiding the use of aspirin was mentioned in 51 per cent of advice leaflets for children but not in any for adults. The British National Formulary for Children states that the use of aspirin in the UK is not licensed for children under the age of 16 years with certain exceptions because of the risk of Reye's syndrome occurring in the paediatric population.21 Meta-analysis has demonstrated a statistically significant increased risk of developing post-tonsillectomy haemorrhage with regular post-operative use of aspirin in both paediatric and adult patients.Reference Krishna, Hughes and Lin22 Counselling patients who regularly take aspirin regarding this increased risk should therefore be undertaken routinely and included in post-operative information leaflets.
Mouthwash and throat sprays
Seven per cent of advice sheets for adults recommended the regular use of mouthwashes and throat sprays post-operatively. A 2013 Cochrane review of seven trials on the use of oral rinses, mouthwashes and sprays concluded that poor reporting quality, high risk of bias and inadequate data did not permit comprehensive and reliable conclusions to be made regarding their efficacy in aiding post-operative recovery.Reference Fedorowicz, van Zuuren, Nasser, Carter and Al Langawi23 Limited results suggested that lidocaine spray appeared to be more effective than saline spray at reducing the severity of pain until the third post-operative day, and although a small number of participants experienced a burning or stinging sensation with benzydamine spray, it was generally not sufficient enough to cause discontinuation of its usage.Reference Fedorowicz, van Zuuren, Nasser, Carter and Al Langawi23 Further prospective, double-blind, large-scale, randomised, controlled trials on the use of such adjuncts are required in order to draw more reliable conclusions.
General post-operative risks
The most frequently mentioned post-operative risks in the leaflets analysed were increasing post-operative pain (18 per cent), bleeding (71 per cent), infection (74 per cent), otalgia (68 per cent) and need for a repeat procedure (65 per cent; Figure 3). It is well known that many post-operative patients will attend their general practitioner surgery with fears that increasing throat pain and otalgia over the first post-operative week indicates evolving or worrisome pathology.Reference Cooper24 Only 21 per cent of adult leaflets and 15 per cent of paediatric leaflets made mention of increasing pain being normal during the first week, while many more mentioned the risk of otalgia (74 per cent for adults, 63 per cent for children). Many studies have documented increased pain scores between 3 and 7 days post-operatively,Reference Tan, Carachi and Anderson25–Reference Stewart, Ragg, Sheppard and Chalkiadis27 and otalgia is also a well-documented risk and seen in up to 69 per cent of children post-tonsillectomy.Reference Castellano, Gámiz, Bracero, Santiago, Soldado and Solanellas28,Reference Lee and Sharp29 Increasing awareness of these common side effects of tonsillectomy could help assuage patient and parent worries in the post-operative period and help reduce the incidence of post-operative general practitioner and hospital attendances.
A recent meta-analysis of nine studies of taste dysfunction following tonsillectomy found that it is a relatively common side effect, estimated to affect 10–20 per cent of patients; however, it is rarely enduring.Reference Kim, Lee, Yun and Bae30 Altered tongue sensation is also frequently seen and can be longer lasting, reported by up to 82 per cent of patients at 3 months post-operatively in one study.Reference Smithard, Cullen, Thirlwall and Aldren31 These risks were mentioned in 60 per cent of leaflets for adults but only in 2 per cent of the leaflets for children; while these are important risks to mention pre-operatively, post-operative written advice reassuring the patient that these symptoms will pass with time should also be considered.
Dysphonia post-tonsillectomy is also relatively common and can be significant; however, it generally resolves over time. In a retrospective study of 1258 patients by Brkic et al. (2020),Reference Brkic, Liu, Campion, Leonhard, Altumbabic and Korlatovic32 patients undergoing adenotonsillectomy, tonsillectomy or adenoidectomy were found to have significant post-operative voice disturbance up to the seventh day, but rates decreased significantly after the first month. This was only mentioned in 21 per cent of leaflets for adults and 2 per cent of leaflets for children. Reassurance that these symptoms will improve could help prevent social and work-related frustrations around these symptoms and should therefore be included in post-operative advice sheets.
Bleeding
Post-operative bleeding represents the most concerning common complication of tonsillectomy. Much research has gone into stratifying the risk of bleeding with different surgical techniques, yet advice around the significance of any bleeding given to patients in the post-operative period appears to vary. The majority of hospitals recommended that any post-operative bleeding should necessitate medical attention (71 per cent adults and children). However, a smaller percentage of hospitals stated that ‘bleeding up to a spoonful is normal’ (12 per cent) or that only ‘continued bleeding’ should prompt medical attention (17 per cent). In a large, multicentre prospective study of 4594 patients, Sarny et al. (2011) calculated that 12 per cent of patients experienced a ‘minor bleed’ (requiring conservative or medical management only) post-tonsillectomy, with 5 per cent experiencing a major bleed (requiring surgical intervention, a blood transfusion or resulting in death).Reference Sarny, Ossimitz, Habermann and Stammberger33 These ‘minor’ bleeds can often be a precursor to a more major bleed, a so called ‘herald’ bleed. Indeed, in the same study, 10 per cent of patients who experienced a minor bleed later went on to have a major bleeding episode (an increase in the risk of a major bleed by a factor of 2 above the overall risk). Forty-one per cent of these second major episodes of bleeding occurred the day after the minor bleed.Reference Sarny, Ossimitz, Habermann and Stammberger33 As such, it seems prudent to recommend to a patient that any episode of bleeding should necessitate medical attention given the risk of subsequent larger bleeds and the potential need for medical therapy to prevent this.
Post-operative risks not mentioned
In light of the landmark Montgomery versus Lanarkshire case of March 2015,34 it has become a legal requirement to include details of ‘material risks’ in the surgical consenting process in order to attain fully informed consent from patients. Material risks should be tailored to the individual patient and as such it may be important to remember and discuss rare and uncommon, but associated, risks that were not frequently mentioned in advice sheets. Such risks include temporomandibular joint dislocation and dysfunction secondary to the surgical technique,Reference Khami, Tan, Glicksman and Husein35 velopharygeal insufficiencyReference Maini, Osborne, Fadl, Spyridakou, Ogunyemi and Hill36 and rotatory subluxation of the atlantoaxial joint, also known as Grisel's syndrome, which can lead to neck deformity and serious neurological complications.Reference Al-driweesh, Altheyab, Alenezi, Alanazy and Aldrees37
Conclusion
Although many hospitals published varying and disparate advice in their individual leaflets, the vast majority agreed on the core principles of returning to a normal diet in the post-operative period, good use of analgesia and safety-netting risks such as post-tonsillectomy haemorrhage. Because of the relative lack of robust, prospective, large-scale randomised, controlled trials on diet in the post-operative period, there is an over-reliance on the use of anecdotal, historical and non-evidence based recommendations on restricted diets and other interventions such as chewing gum.
A thorough review of the literature demonstrated that the overall weight of evidence does not lie in favour of supporting such advice; however, further prospective trials need to be undertaken in this area. Post-operative information leaflets will not substitute appropriate oral pre- and post-operative advice from the operating surgeon; however, they can be a helpful reference tool for patients and parents alike during the recovery period. As such, and in line with the Getting It Right First Time recommendations, these information leaflets should aim to be more comprehensive and evidence-based. We suggest that individual trusts, as well organisations such as British Association for Paediatric Otolaryngology, EIDO Healthcare and ENT UK rapidly and effectively review their advice sheets for adults and children undergoing tonsillectomy. Our summary of the best evidence-based advice to include in hospital leaflets could help hospitals and ENT departments to this end, with the ultimate aim of reducing post-operative morbidity and readmission rates (Appendix 2).
Acknowledgements
The authors thank the freedom of information departments throughout the UK for their help in collecting data.
Competing interests
None declared
Appendix 1. Freedom of information (FOI) request
1 Does your trust / hospital(s) offer tonsillectomy surgery which is undertaken in the trust?
If the answer is no, the FOI request ends here. Please just notify me that your trust / hospital(s) does not undertake this surgery.
If yes, please answer the following questions:
2a Do surgeons in your trust / hospital(s) perform tonsillectomy surgery on children (under 16 years of age)?
2b If the answer to 2a is ‘yes’, do they provide patients / parents of patients in this age group with an information sheet relating to their operation?
2c If the answer to 2b is ‘yes’ please, as well as completing these questions, also send me a copy of the information sheet that is provided, even if it is only sometimes given to patients/parents.
3a Do surgeons in your trust / hospital(s) perform tonsillectomy surgery on young adults and adults (16 years and over)?
3b If the answer to 3a is ‘yes’, do they provide patients in this age group with an information sheet relating to their operation?
3c If the answer to 3b is ‘yes’ please, as well as completing these questions, also send me a copy of the information sheet that is provided, even if it is only sometimes given to patients (unless the same sheet is given to both children/parents and to adult patients in which case please make that clear in your answer and just provide that sheet)
4 What advice is usually given to a) children and b) young adults / adults regarding diet immediately after tonsillectomy (i.e. for approximately the first week or so post-surgery)
Please provide the information requested in the form of PDF leaflets, or scanned images of information sheets.
Appendix 2. ‘Gold standard’ evidence-based advice