Interrupted aortic arch is a rare congenital cardiac lession.Reference Burbano-Vera, Zaleski, Latham and Nasr1 The incidence of the pathology is 3 per million live births and accounts for 1–1, 5% of all CHDs.Reference Garcia, Rey, Lopez, Lamelas and Orozco-Sevilla2 The patients with interrupted aortic arch present with poor perfusion in the distal part of the aorta and pulmonary over circulation in the early neonatal period.Reference Burbano-Vera, Zaleski, Latham and Nasr1
The pathology may be divided into three subtypes based on the location of the interruption such as Types A, B or C as the interruption distal to the left subclavian artery, the interruption distal to the origin of the left carotid artery and proximal to the origin of the left carotid artery, respectively.Reference Javadzadegan, Porhomayon, Sadighi, Yavarikia and Nader3 The most common type is Type B with an incidence of 53% among cases followed by Type A (43%) and Type C (4%).Reference Garcia, Rey, Lopez, Lamelas and Orozco-Sevilla2
The most common presentation of the patients is severe congestive heart failure in the neonatal period,Reference Singh and Singh4 and without treatment, the pathology may end up with mortality in 90% of patients at a median age of 4 days.Reference Javadzadegan, Porhomayon, Sadighi, Yavarikia and Nader3,Reference Firouzi, Mohebbi and Shafiei5 Surgery is the main treatment option for the patients with interrupted aortic arch. Various techniques were defined in the literature such as direct end-to-end anastomosis, use of an anterior patch at the anastomosis site and extensive mobilisation of the descending aorta or prosthetic graft interposition, with pros and cons related with each technique.Reference Dodge-Khatami6
In this report, we present our experiences with autologous pericard roll bypass for the treatment of critically ill infants with interrupted aortic arch.
Patients and methods
The technique was applied in nine infants in severe congestive heart failure and/or organ malperfusion symptoms between July 2011 and December 2019. The patients were retrospectively reviewed, and data regarding the patients were obtained from the records of the hospitals. All the patients were diagnosed with interrupted aortic arch with or without associated congenital cardiac anomalies. Operations were performed by the same team with the same surgical technique. Patients were diagnosed with echocardiography (Fig 1, Suppl. 1). CT angiography was not hesitated when needed (Fig 2). As soon as the patients were diagnosed, patients were transferred to the cardiovascular surgery or new born ICU. Prostaglandin E1 infusion was initiated at appropriate doses to keep the ductus open. All the patients were in critical situations secondary to congestive heart failure and/or symptoms secondary to ischaemia, malperfusion and infection. The surgical treatments had to be performed in certain emergency conditions without optimising the conditions of the patients despite meticulous care and medical treatment, and considering the high mortality and morbidity risks, and not being able to perform the ideal surgical treatment; hence, the procedures were usually bailout interventions. The parents of the babies were informed about the status of the patients and risks and benefits of surgical treatment, and then surgeries were planned following their consent.

Figure 1. Echocardiographic appearance of interrupted aortic arch.
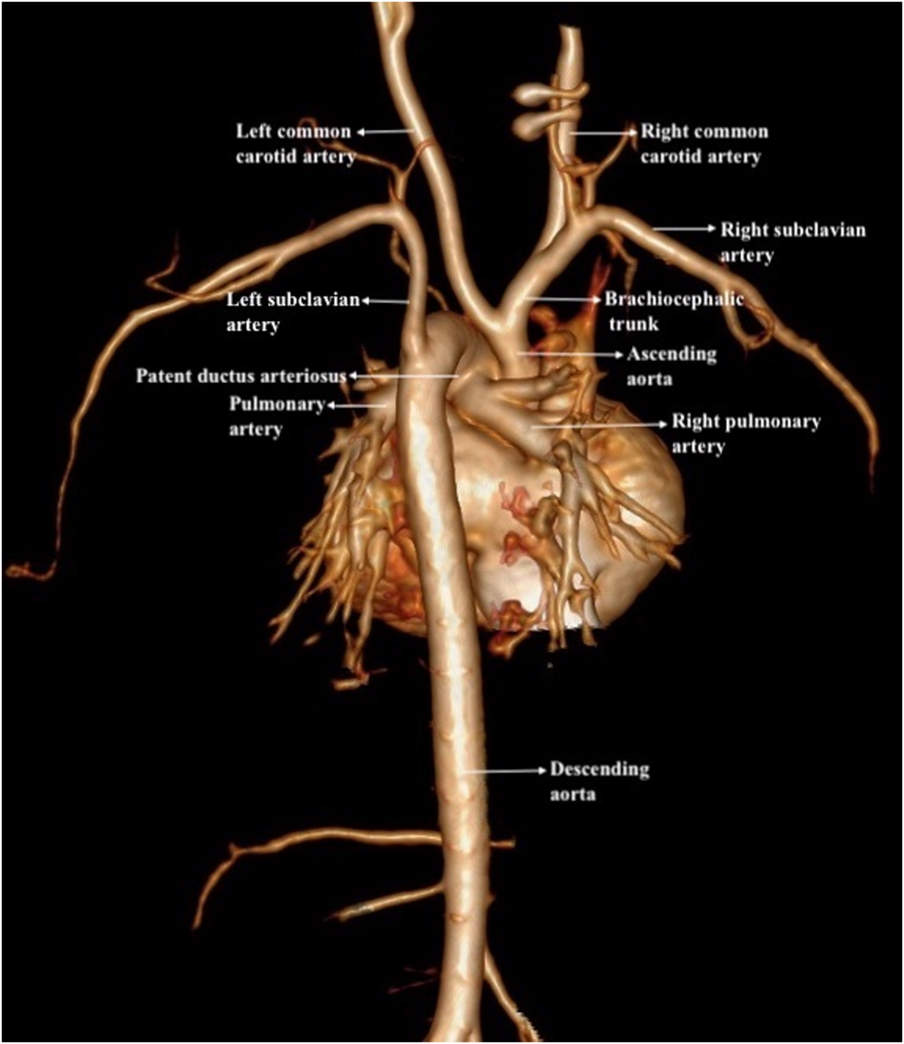
Figure 2. CT angiography of the interrupted aortic arch.
In all patients, the co-morbidity factors were determined depending on haemodynamic status, intubation requirement, ischaemia symptoms, routine blood gas analysis, complete blood cell count, biochemical tests including liver, kidney and gastrointestinal enzymes, necrotising enterocolitis status, preoperative blood, blood product and/or albumin transfusion requirements, alimentation and derangement of symptoms despite meticulous care.
Surgical technique
All the patients were already intubated at the ICU. Two arterial lines, one from the right radial arterial artery and another from the femoral artery, and a central venous line from the right jugular vein were inserted preferably by ultrasonographic guidance. Cerebral near-infrared spectroscopy probes attached to the forehead were not hesitated. Following median sternotomy, the thymus was partially resected. The pericardium was opened. The ascending aorta, brachiocephalic trunk, left carotid artery, ductus arteriosus, aortic arch, left subclavian artery and the descending aorta as far as it can be reached were dissected-free and looped with tapes. The length between the descending aorta and the ascending aorta was simply measured and appropriate length of the pericardial roll bypass graft determined. The required amount of pericardium was excised. The pericardial rolls were created by rolling the pericardium around Hegar dilators (usually 7–8 mm) and double-line suturing with 7.0 polypropylene material.
Pericardium was used fresh pericardium in two cases. Pericardial rolls were soaked in 0.6% gluteraldehyde solution for 3 minutes in four patients. In the remaining three cases, pericardia were excised, soaked in 0.6% gluteraldehyde solution for 3 minutes and then the rolls were created.
After systemic injection of 50–100 units/kg heparin, the ductus arteriosus was ligated and divided. The descending aorta was clamped distally. The pericardial roll was anastomosed end to end to the descending aorta beyond the ductal tissue-free segment with a 7.0 polypropylene suture. The proximal end of the pericardial roll was anastomosed end to end to the aortic arch or end to side to the appropriate region of the ascending aorta or the aortic arch with a 7.0 polypropylene suture with a side-biting clamp. During proximal clamp, the compromise in cerebral blood flow was checked with right radial arterial pressure and/or right and left near-infrared spectroscopy values. Clamps were removed following air evacuation following the anastomosis. The blood pressure decrease after removal of the clamps was managed with infusion of volume. Inotropic support or infusion of NaHCO3 infusion was not hesitated when needed. The gradient between femoral and radial artery pressures was measured after stabilisation of the patients perioperatively. Heparin was not neutralised with protamine.
Additional procedures such as pulmonary bands were performed in selected patients.
Results
Preoperative
Nine patients with unstable haemodynamics as well as certain ischaemic symptoms in critical conditions were emergently operated. There were four girls and five boys. The mean age of the patients was 7.5 ± 2.4 (range: 3–11 days, median: 8 days). One patient was premature, and four patients had low weight. Weights of the patients ranged between 2430 and 3450 g (mean: 3030 ± 366, median: 3200 g). The interruption types of the patients were Type B in six cases and Type A in the remaining three babies. Additional cardiovascular anomalies were ventricular septal defect in all (seven isolated and two in conjunction with single-ventricle pathologies), atrial septal defect or patent foramen ovale in all, single-ventricle pathologies in two and bicuspid aortic valve in three. All the patients had various degrees of patent arterial duct and received prostaglandin E1 infusion. The demographic features of the patients are summarised in Table 1.
Table 1. The demographic and preoperative features of the patients

ASD=atrial septal defect; PFO=patent foramen ovale; VSD=ventricular septal defect.
The co-morbidity factors included congestive heart failure, ischaemic symptoms and infection. A certain degree of gastric intolerance was present in eight of the patients, and alimentation was stopped except the premature baby. Seven of the patients received inotropic support such as milrinone alone or combined with additional agents including adrenalin, noradrenalin and/or dopamine. Various degrees of necrotising enterocolitis were present in all patients such as Type 1 A in one, Type 1 B in one, Type 2 A in five, Type 2B in one and Type 3 A in one. All the patients received anti-biotherapy and total parenteral nutrition. Blood and blood products or human albumin were not hesitated for maximum supportive therapy. Serial blood gas analysis was performed in all patients, and acidity status of the blood, NaHCO3, lactate, bilirubin and base excess levels were closely checked. Complete blood cell count, kidney and liver functions were tested on daily basis and managed accordingly. The co-morbidity features of the patients are presented in Table 2.
Table 2. Co-morbidity features

H=High; N=Normal.
Perioperative
The mean duration of surgery was 180 ± 34.8 (range:120–240 minutes, median: 180 minutes) minutes. Perioperative ventricular fibrillation occurred in one patient, and sinus rhythm was obtained with defibrillation. Carefully placed small, thin and gentle side-biting clamps were used to partially clamp of the ascending aorta or the aortic arch, and the clamps did not compromise the cerebral blood blow in any of the patients. Together with the release of the clamps and distal perfusion, a rapid decline in blood pressure was observed and it was managed with intravenous fluid infusion. The blood gas analysis indicated increase in lactate levels as high as 18 mmol/L (difference from the time of operation: 4–11; mean 8.2 ± 3.9 mmol/L, median: 7 mmol/L). In seven patients, we observed minimal gradient (between 3 and 7 mmg), in one patient no gradient between the right radial and femoral artery. In one case, the femoral artery pressure was measured 2 mmHg higher than the radial artery pressure. In six patients, pulmonary artery banding was added to the interruption repair and bands were adjusted to reveal oxygen saturation above 85% with 60% FiO2. In patients with muscular or small ventricular septal defects with high probability of spontaneous closure, pulmonary bands were not performed. In all cases, the sternums were closed no matter it compressed the heart.
Post-operative
Early post-operative
Post-operative early mortality occurred in one patient with severe mitral regurgitation on the third day due to multi-organ failure secondary to cardio-septic shock. Mortality did not occur in any of the other patients. Erythrocyte suspension and/or fresh frozen plasma suspensions were transfused in eight patients. In one patient, cryoprecipitate was additionally used. The femoral pulses were palpable in all patients. Inotropic support with milrinone was routinely applied, and when the milrinone dose reached 0.75 mcg/kg/minute, additional inotropes including dopamine, adrenaline and/or noradreline were infused. Mean inotrope scores of the patients were calculated 37.2 ± 14.8 (median: 35). The antibiotheraphy was maintained with pre-operatively initiated agents and adjusted according to the acute-phase reactants including white blood cell and thrombocyte counts, C-reactive protein levels, body temperature and appearance of the lungs on the chest X-rays. All the patients could be weaned off the ventilator in 4 days (mean: 39 ± 25.44 hours, median: 24 hours). Neurologic morbidity did not occur in any patients. Echocardiography revealed successful procedure in all patients, post-operatively. Mean duration of ICU stay was 6 ± 2.9 (range: 3–11 days, median: 5 days) days. Dialysis was required in one patient with severe mitral regurgitation and peritoneal dialysis was attempted; however, this patient was lost. The creatinine and liver enzyme levels mildly increased in the post-operative period in the living patients who did not require intervention; but the doses and the types of the antibiotics were adjusted accordingly. Duration of hospital stay after the surgery ranged between 8 and 16 days (mean: 10.1 ± 3.3 days, median: 8.5 days). Early post-operative data of the patients are presented in Table 3.
Table 3. Operative and early post-operative features of the patients

Late post-operative
The patients are followed a mean of 49.5 ± 28.1 (range: 18–106 months, median: 40 months) months at the outpatient clinics periodically, and additional procedures are planned in at least 2 years, unless emergent. One patient who had single-ventricle pathology and required anti-congestive therapy with digoxin, furosemide and captopril during the follow-up underwent bidirectional Glenn procedure and required high doses of inotropic support and received furosemide infusion at the post-operative period. Extubation was attempted 3 times, however, could not be successful due to respiratory acidosis leading to myocardial depression in two attempts and convulsion in the last attempt. He was lost on the post-operative 26th day due to multi-organ failure secondary to sepsis. The other patient with single-ventricle pathology underwent an uneventful bidirectional Glenn procedure.
The two patients who received pericadial roll bypass with fresh pericardial tissues presented to the clinic with dilatation of the pericardial roll 18 and 24 months after the operations. They both had ventricular septal defects initially, and the defects were found to be closed spontaneously in one patient and were apical and insignificant in the other. They were periodically followed with serial echocardiographies for the increase in the dilatation of the rolls. The size of the pericardial roll reached to 3.8 cm in diameter with echocardiography in one case, confirmed with CT revealing 4 cm in diameter (submitted elsewhere) with stenosis at the proximal ascending aortic anastomosis region of the pericardial roll. The patient underwent surgical restoration of the dilated pericardial roll by resection of the anterior enlarged segment and reconstruction including the ascending aorta with a xenograft patch with our on-pump beating-heart full-body perfusion technique,Reference Ugurlucan, Yildiz and Ulukan7 uneventfully. The stenosis at the proximal anastomosis might have contributed to the aneurysm formation (i.e. post-stenotic dilatation) in addition to the fresh material use. When the aneurysm was opened, there was thickened endothelial lining without any thrombus formation in the sac. The other patient did not require any interventions, so far.
Uneventful, de-banding, patch reconstruction of the pulmonary artery and surgical ventricular septal defect closure were performed in two patients 2 years after the interruption repair.
Major complications did not occur at the following surgical procedures neither during re-do sternotomy nor dissection of the mediastinal structures and major vessels. The pericardial rolls were relatively devoid of severe adhesions to the surrounding structures. It was relatively easy to dissect even the dilated pericardial roll in aneurysm case.
Spontaneous ventricular septal defect closure was observed in one patient, and this patient received balloon dilatation of the pulmonary artery. In the remaining patients, successful percutaneous balloon dilatation of the pulmonary artery and device closure of the ventricular septal defect were performed.
Except one early and one late death, the remaining patients are asymptomatic, active and within normal limits of body and mental growth. The patient with single-ventricle pathology who underwent bidirectional Glenn is followed with oxygen saturation above 93% and a Fontan procedure is not planned with current haemodynamics and saturation values. Control CT angiography images of one of the patients with pericardial roll bypass and pulmonary artery band are presented in Fig 3 and Cine of the tomography (Suppl. 2). The late post-operative data of the patients are presented in Table 4.

Figure 3. Control CT angiography of a patient who received pericardial roll bypass between the ascending aorta and the descending aorta, and pulmonary banding procedure.
Table 4. Late post-operative features of the patients

VSD=ventricular septal defect.
Discussion
Interrupted aortic arch is a life-threatening congenital cardiovascular malformation with an incidence of 3 per million live birthsReference Garcia, Rey, Lopez, Lamelas and Orozco-Sevilla2 and rarely occurs as an isolated lesion.Reference Firouzi, Mohebbi and Shafiei5,Reference Chen, Li and Pu8 Ventricular septal defect is the most common concomitant anomaly in these patients that is seen in 73% of the cases. The patent ductus arteriosus has to continue as descending aorta otherwise lower body perfusion is compromised.Reference Javadzadegan, Porhomayon, Sadighi, Yavarikia and Nader3,Reference Varghese, Saheed, Omoregbee, Ninan, Pavithran and Kothandam9 Bicuspid aortic valve and right subclavian artery abnormalities may also be seen in these patients.Reference Burbano-Vera, Zaleski, Latham and Nasr1 Other associated rare cardiovascular anomalies include truncus arteriosus, single-ventricle pathologies, atrioventricular canal defects and transposition of great arteries.Reference Jonas10 Various single-ventricle pathologies may be seen in 11% of patient with interrupted aortic arch.Reference LaPar and Baird11 An atrial septal defect or usually a patent foramen ovale is almost always present in all cases.Reference Jonas10 The subaortic stenosis based on subaortic fibrous membrane is not common in these patients; however, a subaortic membrane may occur in patients who receive neonatal interrupted aortic arch repair in 1 to 2 years.Reference LaPar and Baird11 Especially in the Type B interrupted aortic arch, genetic testing is suggested due to high association with DiGeorge Syndrome.Reference Javadzadegan, Porhomayon, Sadighi, Yavarikia and Nader3
The affected patients rarely reach adulthood without surgical treatment. In these patients, the main factor of the survival is the extensive collateral vessels that provide distal blood flow.Reference Chen, Li and Pu8 In the neonatal period, the pathology is associated with severe congestive heart failure or lower body hypoperfusion, severe metabolic acidosis and multi-organ failure with the ductal closure.Reference Burbano-Vera, Zaleski, Latham and Nasr1,Reference Javadzadegan, Porhomayon, Sadighi, Yavarikia and Nader3 The mortality in the first days of life is generally due to the closure of the patent ductus arteriosus; and without treatment, 90% of the patients die at a median age of 4 days.Reference Javadzadegan, Porhomayon, Sadighi, Yavarikia and Nader3,Reference Firouzi, Mohebbi and Shafiei5
The physical examination may reveal differential cyanosis and the gradient between lower and upper peripheral pulses in neonatesReference Javadzadegan, Porhomayon, Sadighi, Yavarikia and Nader3,Reference Singh and Singh4 which are clues for either aortic interruption or coarctation which may be confirmed with transthoracic echocardiography, initially.Reference Chen, Li and Pu8 CT angiography and MRI may also be used in challenging cases to confirm the exact pathology regarding the aortic arch and differential diagnosis between aortic coarctation, interrupted aortic arch and the exact type location of the stenosis/interruption at the aortic arch.Reference Chen, Li and Pu8
Although in the preoperative period, prostaglandin E1 infusion is vital for the survival to provide ductal patency,Reference Burbano-Vera, Zaleski, Latham and Nasr1 early surgical therapy is the main treatment option for the babies with interrupted aortic arch.Reference Javadzadegan, Porhomayon, Sadighi, Yavarikia and Nader3,Reference Chen, Li and Pu8 Endovascular treatment may be considered when two parts of the aorta are very close or only separated with a membrane,Reference Firouzi, Mohebbi and Shafiei5,Reference Celebi, Sarıtaş, Demir, Akdeniz and Erdem12 treatment methods include end-to-end or end-to-side direct anastomosis, graft interpositionReference Chen, Li and Pu8 and extra-anatomic bypass using a graft.Reference Garcia, Rey, Lopez, Lamelas and Orozco-Sevilla2 End-to-end direct anastomosis or extended aortic arch anastomosis are the most common and relatively the most anatomical surgical techniques; however, direct anastomosis may cause stenosis and/or bronchial compression. The technique also requires extensive mobilisation of the descending aorta.Reference Nishioka, Fuchigami and Akashige13,Reference Cr, Aggarwal, Joshi and Joshi14 Thus, an anterior patch may be utilised at the anastomosis site to provide reduced anastomotic tension which may also decrease the risk of stenosis and tracheobronchial compression after the operation and in the long run.Reference Dodge-Khatami6 Pericardial materials or arterial allografts may also be used in reconstruction of the aorta.Reference LaPar and Baird11 Bechtold et al.Reference Bechtold, Purbojo and Schwitulla15 used various patch materials including autologous pericardium treated with 0.6% glutaraldehyde for 20 minutes, bovine pericardium and homograft patches. In their series, re-coarctation occurs in certain cases especially who received autologous pericardium during initial arch repair.Reference Bechtold, Purbojo and Schwitulla15 Bernabei et al.Reference Bernabei, Margaryan, Arcieri, Bianchi, Pak and Murzi16 used gluteraldehyde-treated autologous pericardium in their cases for aortic arch repair, and they faced with re-stenosis in some of their cases. Their attempt was to balloon dilate the stenosed arches primarily; however, unsuccessful cases were surgically treated. They detected an overgrowth of neo-intima to be responsible for the progressive lumen narrowing.Reference Bernabei, Margaryan, Arcieri, Bianchi, Pak and Murzi16 In our series, fresh or short-duration gluteraldehyde-treated autologous pericardial materials were used for the treatment of aortic interruption. We faced with pericardial roll dilatation in patients who received fresh tissues both of which presumed to result due to decreased strength of the material at the aortic position as well as additional proximal anastomosis stenosis in one (submitted elsewhere) who was further operated.Reference Ugurlucan, Yildiz and Ulukan7 The remaining living patients are followed uneventful in good conditions devoid of significant stenosis of the used materials.
Literature includes reports in which the main pulmonary artery was used for the reconstruction of the aortic arch as an autograft tube regarding growth potential of the graft.Reference Lee, Lee and Lee17 Additional procedures for the concomitant cardiac pathologies or for remote operations such as pulmonary bands should also be added to the aortic interruption repair. A modification of Norwood arch reconstruction in aortic arch repair was introduced by Urencio and associates for a tension-free repair in patients with interrupted aortic arch. The technique is called ascending aorta slide technique and uses the ascending aortic flap as a posterior bridge of the connection between proximal and distal parts of the interruption.Reference Urencio, Dodge-Khatami, Greenleaf, Aru and Salazar18 The small ascending aorta and bleeding risk as a result of long suture line are some of the disadvantages of the technique.Reference Takeuchi19
All of these techniques require cardiopulmonary bypass. Following cardiopulmonary bypass, myocardial oedema and reduced cardiac output may occur in the post-operative period. Care of the critically ill patients during or after cardiopulmonary bypass may be highly complicated due to the side effects of the extracorporeal circulation.Reference Burbano-Vera, Zaleski, Latham and Nasr1 Additionally, the extensive mobilisation of the aortic arch may cause recurrent laryngeal and phrenic nerve injuries.Reference Burbano-Vera, Zaleski, Latham and Nasr1 The residual aortic arch obstruction is not an uncommon pathology and ends up with requirement of the re-intervention in approximately 20% to 40% of the patients who receive aortic interruption repair.Reference Burbano-Vera, Zaleski, Latham and Nasr1 Angioplasty may be considered in case of re-stenosisReference Dodge-Khatami6,Reference Bechtold, Purbojo and Schwitulla15,Reference Bernabei, Margaryan, Arcieri, Bianchi, Pak and Murzi16 ; however, the results in the literature reveal that the technique did not reduce the need for surgical reoperation.Reference Burbano-Vera, Zaleski, Latham and Nasr1
Respiratory complications are the other major complications most probably occur secondary to the external compression of the airways especially the left main bronchus most probably due to inadequate mobilisation of the descending aorta and aortic stretch afterwards.Reference Dodge-Khatami6,Reference Maddali, Kandachar, Mohsen, Arora and Lacour-Gayet20 A prosthetic interposition graft may also be utilised for the treatment but due to the inability of growth potential of the graft material re-intervention becomes mandatory in the growing patients. To overcome the re-interventions for the graft incompatibility, the native tissues are frequently preferred, such as subclavian rotational flap, but this technique sacrifices a major artery to the upper extremity.Reference Dodge-Khatami6
Our technique with an autologous pericardial roll bypass eliminates the need for cardiopulmonary bypass; hence, the patients are protected against the negative effects of cardiopulmonary bypass and do not suffer from many post-operative complications during the myocardial recovery process; being vitally important especially in critically ill infants. The duration of the operation may be relatively shorter as it includes only two anastomosis and devoid of cardiopulmonary bypass. The pulmonary dysfunction both secondary to cardiopulmonary bypass and bronchial compression due to descending aortic proximal anastomosis may be prevented providing a less complicated pulmonary course and easier and faster extubation. During the growth period, depending on the use of a native tissue, re-intervention may not be required. However, use of fresh materials revealed graft dilatation in our two cases and gluteraldehyde-fixed materials have been relatively protected with certain degree of graft growth.
Limitations
The major limitations of the study are the small number of patients and relatively short duration of follow-up. Additionally, it is a non-comparative study and manuscript is devoid of comparison results of the technique with conventional methods. However, the technique was a bailout procedure in critically ill newborns with the diagnosis of interrupted aortic arch who otherwise may be lost secondary to the side effects of cardiopulmonary bypass such as dissemination of sepsis, revealing oedema, myocardial depression or pulmonary complications. Another limitation of the study is the retrospective nature of the research.
Conclusions
Treatment of interrupted aortic arch with a bypass with an autologous pericardial roll without cardiopulmonary bypass seems a safe and reliable technique for the treatment of critically ill infants. Short duration of low-concentration gluteraldehyde fixation of the autologous tissue provides long-term event-free survival with adequate growth of the neo-arch in the growing child. Although fresh use of the pericardium does not change the early outcome, it carries risk of dilatation which may further require intervention.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951120001687
Acknowledgements
None.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of Interest
None.









