The concept of “early extubation” has been initially proposed and implemented in adult cardiac surgery where it has become widely adopted.Reference Hawkes, Dhileepan and Foxcro1 The paediatric cardiac surgical population is quite distinct from the adult cohort concerning not only the age-dependent differences, but also the fact that paediatric cardiac surgery involves different types of haemodynamics and doesn’t always result in the re-establishment of biventricular circulation. This contributes to a widely heterogeneous group of children, where the experience with early extubation after heart surgery is less well described. Many factors have to be considered for the decision of ventilatory discontinuation, amongst them being the heart disease, surgical volume, cardiopulmonary bypass time and aortic cross-clamp time, and their potential deleterious effects, as well as the use of opioids, inotropes, or hypothermia.Reference Durandy, Younes and Mahut2,Reference Jin, Yum and Kim3
Awakening and spontaneous breathing trials are important components of developing an early extubation strategy. Spontaneous breathing trials aim to assess patients’ readiness for extubation. Newth et al (2009)Reference Newth, Venkataraman and Willson4 presented a systematic review, which concluded that the use of a weaning protocol in both children and adults results in shorter ventilator times, improved outcomes, and lower costs.
The International Quality Improvement Collaborative for congenital heart surgery was designed in 2007 to address the lack of quality evaluation of surgical programmes in low/middle-income countries and to identify risk factors contributing to poor surgical outcomes. As part of the IQIC since 2016, National Cardiology Hospital participated in a quality improvement education course, which resulted in the implementation of a daily spontaneous breathing trial protocol as a quality improvement project in our centre. A study was conducted, in which patients were divided into a pre-protocol cohort (n = 35) and a post-protocol cohort (n = 38) and patients’ perioperative, intraoperative characteristics, and outcomes were compared between the two groups. After protocol implementation, abnormal chest radiograms decreased from 28.6 to 5.2% (p = 0.043) and early extubated patients increased from 20 to 30% (p = 0.047). Protocol implementation didn’t lead to a significant decrease in duration of mechanical ventilation, cardiac ICU and hospital length of stay, but resulted in more consistent approach to the process of ventilator weaning in our centre. The findings of the study were presented as an electronic poster during the Pediatric Cardiac Intensive Care Society’s 16th Annual International Meeting.
The goal of this study was to describe our initial experience with a protocol-driven early extubation strategy in paediatric cardiac surgical patients. We sought to identify risk factors associated with failed spontaneous breathing trials within 12 hours of ICU admission.
Materials and methods
Setting and population
The study was conducted in National Cardiology Hospital, located in Sofia, Bulgaria. It is the only centre in the country involved in the surgical treatment of congenital heart defects. The paediatric cardiac ICU consists of 8 beds, while 230 paediatric cardiac surgeries are annually performed.
Children up to 18 years of age, undergoing paediatric cardiac surgical procedures, with or without the use of cardiopulmonary bypass were investigated. Exclusion criteria from the study were patients less than 1 month of age, preoperative mechanical ventilation, atrial septal defect, persistent ductus arteriosus surgery, delayed sternal closure, death within 12 hours after surgery in mechanically ventilated patients. Patients younger than 1 month of age were not included as early extubation in this population was scarce. Patients after atrial septal defect and patent ductus arteriosus surgery were excluded because all of them were extubated in the first 12 hours after surgery, which could skew the data. Data were collected during a 1-year period from June, 2018 to May, 2019 on the patients that met the inclusion criteria (129 of 213). The study protocol was approved by the Ethics Committee in our institution and the need for patient consent was waived due to the study’s retrospective nature. A protocol-driven early extubation strategy within 12 hours after surgery was pursued (Fig 1).
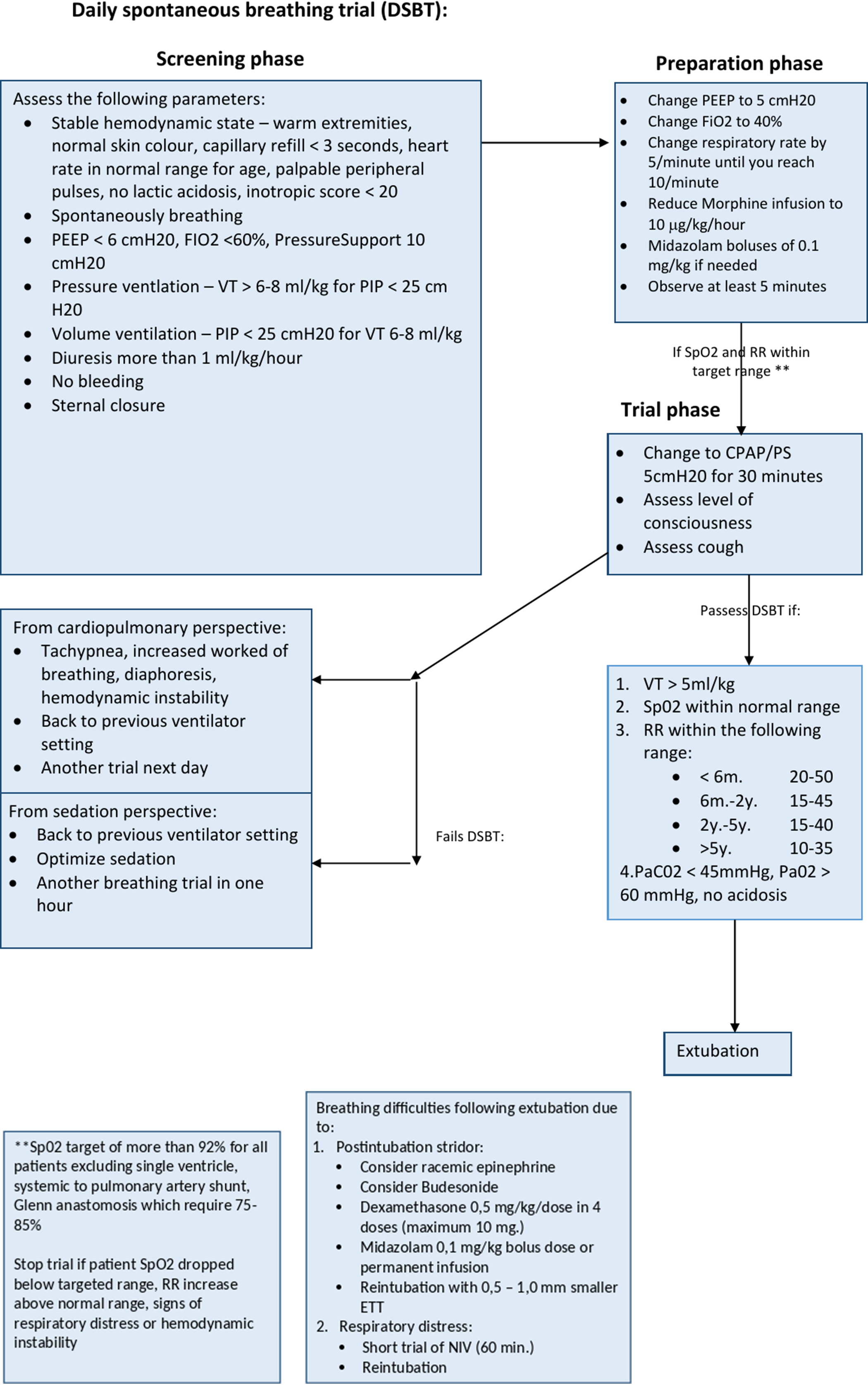
Figure 1. Daily spontaneous breathing trial protocol. PEEP = Positive end-expiratory pressure; PS = pressure support; FiO2 = Fraction of inspired oxygen; VT = Tidal volume; PIP = Peak inspiratory pressure; RR = respiratory
The study population (n = 129) was stratified into two age groups: infants (patients aged 1 from month to 1 year, n = 84) and children (from 1 year to 18 years, n = 45). Patient groups were further stratified into two subgroups according to extubation status based upon the daily spontaneous breathing trial protocol assessment – successfully passed a daily spontaneous breathing trial with subsequent early extubation (ventilation time less than 12 h after surgery, n = 86) and failed daily spontaneous breathing trial with deferred extubation (ventilation time more than 12 h after surgery, n = 43). The process of the study is presented in Fig 2.
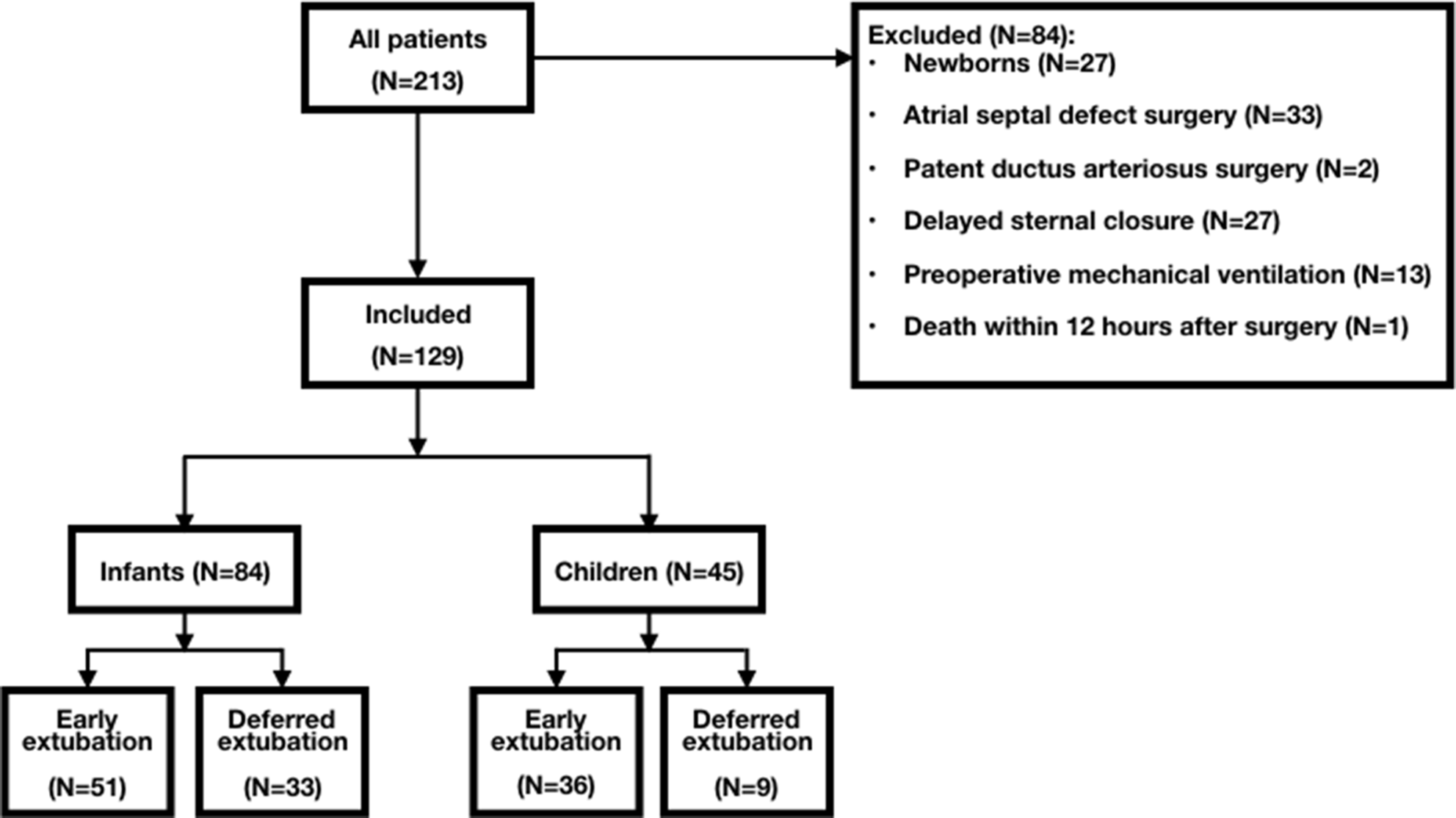
Figure 2. Flowchart of the study population process.
Anaesthesia
Induction of anaesthesia included 0.3 mg/kg of midazolam and 3–5 μg/kg of fentanyl. Tracheal intubation was facilitated by 2 mg/kg of suxamethonium chloride. After induction of anaesthesia, an intra-arterial line was used to monitor arterial pressure and blood gas analysis, and a double lumen central venous catheter was inserted to measure central venous pressure, deliver vasoactive drugs, and repeatedly monitor venous oxygen saturations. Anaesthesia was maintained with isoflurane and additional fentanyl boluses of 3–5 μg/kg. Catecholamine and volume management intraoperatively was guided by the haemodynamic status of the patient and the judgement of the attending anaesthesiologist. Post-operative analgesia was achieved through continuous morphine infusion of 10–20 μg/kg/hour and paracetamol of 10–15 mg/kg up to a maximum of four doses in 24 hours.
Management in the pediatric cardiac ICU
None of the patients were extubated in the operating room. Upon arrival in the paediatric cardiac ICU, a daily spontaneous breathing trial protocol was used to assess patients’ readiness for extubation, adapted from the protocol proposed by Abu-Sultaneh et al (2017).Reference Abu-Sultaneh, Hole and Tori5 Chlophazoline for infants and propofol for older children were used as sedatives. The daily spontaneous breathing trial protocol has three phases: (1) screening phase; (2) preparation phase; and (3) pressure support/continuous positive airway pressure trial phase (Fig 1). The attending physician is responsible for the assessment for all screening criteria. The timing of extubation was decided by the attending paediatric cardiologist, and is informed by the results of the spontaneous breathing trial protocol.
Primary and secondary outcome definitions
Patients’ charts were reviewed for patient characteristics and primary outcomes of interest were defined: early extubation, defined as eligible patients who have successfully passed a daily spontaneous breathing trial protocol and were extubated within 12 hours after arrival in the paediatric cardiac ICU. Secondary outcomes were ventilation time (cumulative duration of mechanical ventilation during the entire ICU stay), early extubation failure (need of re-intubation within 24 hours after early tracheal extubation), respiratory morbidity (presence of pulmonary infiltrate, atelectasis on chest radiogram), ICU and hospital length of stay. Weaning failure is defined as a failure to pass a spontaneous breathing trial within 12 hours after arrival in the paediatric cardiac ICU. Procedures were classified according to the Risk Adjustment for Congenital Heart Surgery category.Reference Jenkins6 Nutritional status was defined as malnourished when the weight-for-age z score was <−2.7
Statistics
Descriptive statistics were used to provide frequencies and percentages for categorical variables and means, medians, and standard deviations for continuous variables. We used the Mann–Whitney U-test to compare the distribution of continuous variables between early extubated and deferred extubated patients. A two-sided p-value <0.05 was considered statistically significant. A binomial logistic regression model was performed to ascertain the effects of age, weight, nutritional status, aortic cross–clamp, and cardiopulmonary bypass times on the likelihood that patients successfully pass a spontaneous breathing trial within 12 hours after surgery. Linearity of the continuous variables with respect to the logit of the dependent variable was assessed via the Box–Tidwell procedure. A Bonferroni correction was applied using all 10 terms in the model resulting in statistical significance being accepted when p < 0.0055. Based on this assessment, all continuous independent variables were found to be linearly related to the logit of the dependent variable. Analyses were performed using SPSS statistics 24.0 software.
Results
Comparisons of preoperative and intraoperative patients’ characteristics by age group stratification are described in Table 1 and patients’ outcomes are shown in Table 2. Infants who were younger, malnourished had lower weight, longer cardiopulmonary bypass and aortic cross-clamp time were less likely to successfully pass a daily spontaneous breathing trial and undergo early extubation. These patients exhibited significantly longer ICU and hospital length of stays (Figs 2 and 3), mortality, and re-intubation rates.
Table 1. Comparison of early and deferred extubated patients’ perioperative and intraoperative characteristics by age group

AoX = Aortic Cross-Clamp; CPB = Cardiopulmonary bypass; ICU = Intensive care unit; LOS = Length of stay; RACHS = Risk Adjustment for Congenital Heart Surgery.
Table 2. Comparison of early and deferred extubated patients’ outcomes of patients by age group

ICU = Intensive care unit; LOS = Length of stay; Ro = Roentgenography.

Figure 3. A comparison of the ICU length of stay between early extubated and deferred extubated patients. (a) All patients and (b) Patients up to 1 year of age. Boxes represent median, the low and high quartile, and the whiskers indicate the minimum and maximum values. A comparison of the Hospital length of stay between early extubated and deferred extubated patients. (c) All patients and (d) Patients up to 1 year of age. Boxes represent median, the low and high quartile, and the whiskers indicate the minimum and maximum values.
Children who failed to pass a daily spontaneous breathing trial and deferred extubation had experienced significantly longer CBP and aortic cross-clamp time, but showed no statistical significance in the studied outcomes. More children (80%) successfully passed a daily spontaneous breathing trial and achieved early extubation than the infants (61%). Reintubation occurred in 4.7% (n = 4) of the early extubated patients: three patients due to respiratory reasons; one patient due to haemodynamic instability from moderate aortic regurgitation after ventricular septal defect surgery.
Risk factors for failed spontaneous breathing trial within 12 hours after surgery
A binomial logistic regression model was performed on the infant group to assess the risk for failed spontaneous breathing trial within 12 hours after surgery. Of the five predictor variables, only cardiopulmonary bypass CPB time and malnourished patients were significantly associated with an increased likelihood to fail ventilator weaning (Table 3).
Table 3. Logistic regression predicting the likelihood of failure to pass a spontaneous breathing trial within 12 hours after surgery in infants based on age, weight, malnourished patients, CPB, and AoX times

AoX = Aortic Cross-Clamp; CPB = Cardiopulmonary bypass.
Note: Age was assessed in years, weight was measured in kilograms, cardiopulmonary bypass, and aortic cross-clamp time were analysed per minute.
Discussion
Our research suggests that early extubation through a protocol-driven approach is reasonable in the majority of patients following paediatric cardiac surgery. In the present study, we have shown that infants who have successfully passed a spontaneous breathing trial with subsequent early extubation have lower re-intubation rates, lower early mortality, shorter ICU and hospital length of stays compared to infants who failed a spontaneous breathing trial and deferred extubation. The performed binomial logistic regression in the infant group showed that increasing cardiopulmonary bypass times and malnourished patients had an increased likelihood of failure to pass a spontaneous breathing trial within 12 hours after surgery.
Many centres have adopted early extubation programmes after paediatric cardiac surgery. Although a few randomised prospective studies on this issue are present,Reference Preisman, Lembersky and Yusim8,Reference Alam, Shalini, Hedge, Mazahir and Jain9 it is accepted that early tracheal extubation is associated with better post-operative outcomes.Reference Preisman, Lembersky and Yusim8–Reference Barash, Lescovich, Katz, Talner and Stansel11 There is considerable variation across studies in defining “early extubation”. Extubation can be accomplished in the operating room or during the early course in the ICU stay, ranging from 3 hours up to 24 hours.Reference Alghamdi, Singh and Hamilton12
Protocol implementation is another aspect of an early extubation strategy in order to facilitate the process. Spontaneous breathing trials aim to assess patients’ readiness for extubation. It is a useful tool for assessing patient’s spontaneous breathing using a continuous positive airway pressure trial. As a result, a protocol-driven approach safely reduces the duration of mechanical ventilation,Reference Abu-Sultaneh, Hole and Tori5 which leads to weaning of sedation and inotropes, faster initiation of enteral feeding, and decreased incidence of pulmonary infections.
Several authorsReference Preisman, Lembersky and Yusim8–Reference Neirotti, Jones, Hackbarth and Paxson Fosse10,Reference Vricella, Dearani, Gundry, Razzouk, Brauer and Bailey13,Reference Heinle, Diaz and Fox14 reported reduced ICU and hospital length of stay in early extubated patients. Our study confirms this finding in the infants, while no statistically significant difference was observed in the children. We hypothesise that the lack of statistical significance in the children can be explained by the fact that the majority of patients were early extubated, leaving only nine patients in the group with a ventilation time of more than 12 hours.
Overall mortality in the present study was similar to that reported by other authors.Reference Neirotti, Jones, Hackbarth and Paxson Fosse10,Reference Barash, Lescovich, Katz, Talner and Stansel11,Reference Vricella, Dearani, Gundry, Razzouk, Brauer and Bailey13,Reference Shinkawa, Tang and Gossett15 Mortality of early extubated patients varied from 0 to 5%Reference Jenkins6–Reference Preisman, Lembersky and Yusim8,Reference Barash, Lescovich, Katz, Talner and Stansel11–Reference Vricella, Dearani, Gundry, Razzouk, Brauer and Bailey13 whereas in our centre, none of the early extubated patients died.
There is considerable variation in early extubation failure across centres, varying from 1 to 11%.Reference Preisman, Lembersky and Yusim8–Reference Barash, Lescovich, Katz, Talner and Stansel11,Reference Vricella, Dearani, Gundry, Razzouk, Brauer and Bailey13,Reference Heinle, Diaz and Fox14,Reference Gupta, Rettiganti and Gossett16,Reference Benneyworth, Mastropietro and Graham18 Some authors decided not to include neonates and infants less than 6 months of age in their research because of anatomical or physiological reasons, thus lowering the surgical complexity in the studied groups. Early extubation failure in our study was 4.7%. Neonates were excluded from the study, but infants over 1 month of age were included. Our strategy wasn’t limited just to RACHS-1 risk categories 1 and 2. Patients with higher RACHS-1 were also extubated within 12 hours after arrival in our paediatric cardiac ICU, which means that patients undergoing more complex surgical procedures can be extubated early. The rate of re-intubation in the current study differed between the early and deferred extubation groups in infants with the early extubated patients having lower re-intubation rates. There was a difference in the children group when comparing early and deferred extubation, but it was not statistically significant. An explanation to the reported re-intubation rates could be that patients are not extubated rapidly enough, however, we believe that a protocol-driven approach using a spontaneous breathing trial results in a slower, but safer process with less re-intubation rates in early extubated patients.
Our work has demonstrated overall respiratory morbidity of 15%, which included atelectasis and pulmonary infiltrates. This is significantly lower than the values reported by Preisman et al (2009),Reference Preisman, Lembersky and Yusim8 and higher than the ones reported by Barash et al (1980).Reference Barash, Lescovich, Katz, Talner and Stansel11 We found the rate of respiratory complications in both infants and children differed between early and deferred extubation groups, but were not statistically significant.
The authors sought to investigate the odds of failure to pass a spontaneous breathing trial within 12 hours after surgery, since patients from this group exhibited longer ICU and hospital length of stay, increased early mortality, and re-intubation rate. The reported findings extend those of Gupta et al(2010)Reference Gupta, Rettiganti and Gossett16 and Székely et al(2006),Reference Székely, Sápi, Király, Szatmári and Dinya17 confirming that malnourished patients and longer cardiopulmonary bypass times were independent risk factors for weaning failure. In our institution, we have accepted that patients with cardiopulmonary bypass time above 140 mi and aortic cross-clamp time of more than 90 mi should be considered for spontaneous breathing trial 24 hours after the surgical correction as a result of this study. The rationale behind this institutional decision is the potential deleterious effects of prolonged cardiopulmonary bypass and aortic cross-clamp times. Patients with partial and total cavopulmonary connection are an exception, with a goal towards early extubation despite cardiopulmonary bypass and aortic cross-clamp times. During the past 12 months, a total of 13 patients from the infant group had CPB times more than 140 min and AoX times more than 90 min. An interesting finding is that four of the patients with similar haemodynamics (three patients after tetralogy of Fallot repair and one patient after VSD closure and debanding of the pulmonary artery) were extubated early without subsequent re-intubation. This finding could be explained by the fact that spontaneous ventilation has a positive impact on right ventricular function, thus, it could be beneficial for patients after tetralogy of Fallot repair. Future work should include criteria revision with a possibility of considering patients with cardiopulmonary bypass and aortic cross-clamp times of more than 140 and 90 min for early extubation.
However, some important limitations are worth mentioning. The single-centre, retrospective, non-randomised design of the study is a limitation itself. Patient heterogeneity between the studied populations is significant, despite the strict exclusion criteria used in the study. Other studies similar to ours have also compared groups of patients with significant differences in age and nutritional status, which is in favour of the statement that early extubated patients are older and with a better nutritional status. Lack of an anaesthetic protocol concerning limiting the amount of intravenous opioids and sedatives intraoperatively is a barrier for the establishment of an early extubation strategy. Subjective aspects of the clinician’s decision to initiate ventilator weaning were not accounted for in our study. Our work lacked data in certain key patient variables, such as non-cardiac structural anomalies, which might impact extubation success and outcomes.
In conclusion, children after congenital heart surgery undergoing a spontaneous breathing trial with subsequent early extubation had lower ICU and hospital length of stays in infants, without an increase in morbidity or mortality. The majority of the children achieved early extubation utilising a protocol-based approach. Malnourishment and cardiopulmonary bypass times were independent risk factors for failed spontaneous breathing trial.
Acknowledgements
The authors would like to thank the International Quality Improvement Collaborative (IQIC) for organising a quality improvement education course, which provided the necessary tools to design and implement a quality improvement project in our workplace.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflict of interests
None.
Ethical standards
The study protocol was reviewed and approved by the Ethical Committee of National Cardiology Hospital in Sofia, Bulgaria.









