Introduction
In recent years, there has been increased concern about occupational stress. Problems associated with occupational stress are considered to be the most important health threat affecting the workforce, with at least 22% of workers being affected.Reference Harter, Schmidt and Keyes 1 Researchers have tried to develop different theoretical models to improve the understanding of all the variables which affect occupational mental health. Regarding this issue, Karasek’s job strain model, which supports the most widely used self-administered workplace questionnaires,Reference Karasek, Brisson, Kawakami, Houtman, Bongers and Amick 2 has been examined in relation to several different health outcomes and it has been used in several important studies, such as the Whitehall II Study.Reference Marmot, Bosma, Hemingway, Brunner and Stansfeld 3
Most studies on the clinical effects of occupational stress are focused on workplace harassment since it is characterized by a powerful psycho-traumatic effect. 4–7 This allows a better evaluation of the causal relationship between work experiences and symptoms. 8–11 Such prolonged social stress affects emotional wellbeing, likely through changes in neuroendocrine, autonomic, and immune system function.Reference Verkuil, Atasayi and Molendijk 9 , Reference Buselli, Veltri and Baldanzi 12 Several studies concluded that workers who experience unfavorable psychosocial working conditions had an increased risk of developing mental disorders associated with sleep, depression, anxiety, and post-traumatic stress. 13–16 In 2002, the European Commission (EC) estimated that the annual cost of job-related unemployment due to work-related mental disorders in 15 EU countries was on average 3% to 4% of Gross Domestic Product (GDP, about 265 billion euros). 17
For these reasons, work-related mental disorders represent an important public health challenge to be considered not only from a therapeutic point of view but also with respect to prevention.
Preventive medicine public health teams must comply with legal requirements through “vigilance and supervision” policies in order to try to reduce the incidence of these phenomena.
In addition to EC laws, Italy has created a list of occupational diseases with mandatory reporting which is referred to as “mental and psychosomatic disorders related to work organization dysfunction.” This includes post-traumatic stress disorder (PTSD) and adjustment disorder (AD).Reference Kostev, Rex, Waehlert, Hog and Heilmaier 11 , Reference Tonini, Lanfranco and Dellabianca 18
Although the debate and the difficulty in establishing the most occurred psychopathological disorder following a traumatic event is still ongoing, the main manifestations shared to many psychiatric disorders include sleep difficulties, concentration problems, avoidance, anhedonia, isolation and detachment from others, and sense of guilt.Reference Byllesby, Elhai and Tamburrino 19 , Reference Carmassi, Corsi and Bertelloni 20 The key differentiation for PTSD is that these symptoms are compulsorily secondary to a traumatic event but in the case of repeated traumas, as happens with occupational stress, it is difficult to determine the timing of symptoms onset.Reference Flory and Yehuda 21
Even though it has been demonstrated that serious traumatic events are associated with a higher incidence of PTSD and poor outcomes, many authors in recent studies have underlined the importance of minor events. This is especially significant when minor traumatic acts are repeated. This has paved the way for a more holistic approach to trauma, and the emerging concept of trauma dosing leading to post-traumatic reaction.Reference Carmassi, Corsi and Bertelloni 20 , Reference Carmassi, Akiskal and Yong 22 , Reference Carmassi, Corsi and Bertelloni 23
In light of the growing quantity of literature on dimensional approaches to PTSD and recent attention of the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) to trauma-related disorders, a specific questionnaire called "Trauma and Loss Spectrum Self-Report” (TALS-SR) was developed to explore PTSD spectrum symptoms related not only to the core manifestations of PTSD, but also to the attenuated and atypical symptoms. This includes the personality traits and the behavioral manifestations that may be associated with PTSD but which may also be present in subthreshold or partial forms.Reference Dell’Osso, Katherine and Carmassi 24 , Reference Dell’Osso, Carmassi and Rucci 25
In occupational medicine is important to capture symptoms associated with post-traumatic stress in order to prevent critical situations and to be able to accurately diagnose mental disorders and report them to the appropriate responsible institutions.
In the literature, there does not seem to be direct epidemiological data about the impact of PTSD on work-related stress victims. There are some conflicting data about the prevalence of PTSD among harassment victims. An American survey of more than 1000 victims determined that 26% of them had developed PTSD. A Swedish study of 64 victims determined that 92% of them had developed PTSD.Reference Bonafons, Jehel and Coroller-Béquet 26 Other recent studies have evidenced a new pathway of research highlighting high prevalence of PTSD in “burn-out” victims. 27–29
The present cross-sectional investigation fits into this context with the aim of better understanding the impact of post-traumatic stress symptomatology, using a specific self-assessment questionnaire, in a cohort of subjects experiencing occupational stress. The rationale is to start looking at the variegated symptoms expressed by this particular population in a post-traumatic dimensional perspective.
Methods
Participants and procedures
Between September and December 2018, the authors conducted a cross-sectional collection of data by means of a retrospective analysis of both medical records and self-assessment questionnaires of subjects at the Occupational Health Department operating in a university hospital in central Italy between 2016 and 2018. The Occupational Health Department included a multidisciplinary team comprised of occupational physicians, psychiatrists, and psychologists. Both clinical and self-report tools based on the transactional model of stress and the workers’ subjective perception of psychosocial risks were utilized in order to assess the degree of work stress and the presence or absence of occupational diseases, PTSD, and AD.
The study was conducted in accordance to Helsinki Declaration and study participants signed informed consent to data acquisition.
In line with Karasek’s demand-control model of job stress, study participants were assessed using the Work Harassment ScaleReference Nagasawa, Nomura and Takenoshita 30 (WHS) and Job Content QuestionnaireReference Karasek, Brisson, Kawakami, Houtman, Bongers and Amick 2 (JCQ) in order to confirm the degree and nature of their occupational stress. The WHS questionnaire includes 24 items exploring negative and harassment actions at the workplace. Items are coded on a 5-point Likert scale denoting the frequency of these actions in the previous 6 months. The five WHS dimensions were “attacks aimed directly to tasks and duties,” “attacks aimed to expressive opportunities and communication,” “personal attacks,” “direct offensive actions,” and “indirect acts such as isolation, spreading rumors etc.” The total score is obtained as the sum of the items, ranging from 24 to 120. Our sample presented a mean total score of 70.49 (SD = 22.85), ranging between 24 and 118.
The JCQ is a widely used self‐administered workplace environment questionnaire designed to measure social and psychological characteristics of jobs.Reference Karasek, Brisson, Kawakami, Houtman, Bongers and Amick 2 The JCQ contains three main subscales: decision latitude, psychological job demands (PJD), and social support. The PJD mean score in our sample was 26 (SD = 5), ranging between 10 and 36.
Subjects with an insufficient comprehension of Italian that prevented completion of self-report questionnaires were excluded from the study.
Collected data consisted of demographic variables: gender, age, education level (low vs high, respectively, with or without an undergraduate degree), family history of mental disorders, personal physical illnesses (cancer, inflammatory diseases, cardiac diseases, and osteoarticular disorders), fibromyalgia (FM) comorbidity (authors decided to single out this particular condition due to the high recurrence of it in the study sample), and mental disorder comorbidity. Additional collected data included work-related variables: public vs private company, big (>200 employees) vs small company, and the field of work: education, healthcare, law enforcement/army, and service.
The TALS-SR is a questionnaire designed to explore post-traumatic stress spectrum symptoms.Reference Dell’Osso, Katherine and Carmassi 24 , Reference Dell’Osso, Carmassi and Rucci 25 The correlation between the self-report (TALS-SR) and the interview format (SCI-TALS) of the TALS have always exceeded the threshold of 0.90, establishing a substantial reliability in all the domains of PTSD criteria.Reference Dell’Osso, Katherine and Carmassi 24
Data from the TALS-SR were collected and analyzed by psychiatrists who were trained and certified in the use of the TALS-SR.
In accordance to the aims of the present study, data from the TALS-SR were analyzed to assess DSM-5 PTSD criteria related to occupational distress. Due to the sample characteristics, criterion A was considered to be satisfied.
The presence of PTSD was determined by means of the presence of items corresponding to DSM-5 criteria for PTSD. We utilized the following matching between symptom criteria and TALS-SR items: criterion B “intrusion symptoms” (B1 = 80, B2 = 77, B3 = 79, B4 = 78, and B5 = 81), criterion C “avoidance” (C1 = 86, C2 = 87 and/or 88 and/or 89), criterion D “negative alterations in cognitions and mood” (D1 = 90, D2 = 95, D3 = 85, D4 = 96, D5 = 91, D6 = 93, and D7 = 92), criterion E “alterations in arousal and reactivity” (E1 = 108, E2 = 99 and/or 100 and/or 102 and/or 103 and/or 104, E3 = 106, E4 = 107, E5 = 105, and E6 = 109).Reference Carmassi, Akiskal and Bessonov 31 The TALS-SR cannot be considered a substitute of the Structured Clinical Interview for psychiatric disorders according to DSM-5 (SCID), and cannot be used to make a diagnosis without investigating the duration and severity of the symptoms.
Measures: Instruments and assessment
The TALS-SR was developed by some of the authors, who comprise an international (Italian–American) collaboration research project called “Spectrum Project” (http://www.spectrum-project.org/), established to develop and test instruments for the assessment of the spectrum of clinical features associated with the current version of the DSM psychiatric disorders. The spectrum model highlights the significance of isolated symptoms and subthreshold symptom clusters that accompany each disorder classified in the DSM. These isolated and subthreshold symptoms may follow, or be manifested in concurrence with, the main disorder.Reference Cassano, Dell’Osso and Frank 32 The TALS-SR includes 116 items exploring the lifetime experience of a range of loss and/or traumatic events and lifetime symptoms, behaviors, and personal characteristics that can represent manifestations and/or risk factors for the development of a stress response syndrome. The instrument is organized into nine domains. Item responses are coded in a dichotomous manner (yes/no), and domain scores are obtained by counting the number of positive answers. The nine domains are: loss events, grief reactions, traumas, emotional, physical, and cognitive responses to loss and/or traumatic events, re-experiencing, avoidance and numbing, maladaptive coping, arousal, and personality traits/risk factors.
Data analysis
In descriptive statistics of categoric variables, the authors determined the absolute and relative frequencies (n, %), whereas with quantitative variables both mean scores and standard deviations (mean ± SD) are specified. When the variables studied were categoric, for pairwise comparisons the chi-square test (or Fisher when appropriate) was applied. In case of parametric variables, the Student’s t-test for independent samples was utilized when comparing two groups, and the f-test of the analysis of variance followed by Bonferroni’s t-test for post hoc pairwise comparisons were utilized. In the case of nonparametric variables, on the other hand, the Mann–Whitney U-test was applied when comparing two groups, and Kruskall–Wallis’ test followed by Dunn’s test were applied for post hoc pairwise comparisons when more than two groups were involved.
All statistical analyses were carried out using the software package “Statistical Package for Social Science,” version 25.0.
Results
Background characteristics
A population of workers was evaluated at the Occupational Health Department of a university hospital in central Italy. The sample consisted of 345 subjects. This population broke down as follows: 189 women (54.8%) and 156 men (45.2%), with a mean age of 49.8 ± 8.7.
Sociodemographic and work-related characteristics of the overall sample are shown in Table 1. Sixty-one subjects (17.7%) had only a primary school education, 172 (50.0%) had only a high school diploma, and 111 (32.3%) had at least an undergraduate college degree.
Table 1. Sociodemographic and Work-Related Characteristics of the Overall Sample (N = 345) with Mean ± SD Age of 49.8 ± 8.7

Twenty-four subjects (7.0%) worked in educational services, 61 subjects (17.7%) worked in health services, 252 subjects (73.0%) worked in the tertiary sector, and 8 subjects (%) were police or military.
One hundred and twenty-three subjects (35.7%) were employed in a public company and 222 subjects (64.3%) were employed in a private company. One hundred and one subjects (29.3%) worked in a small company and 244 subjects (70.7%) worked in a big one.
Two hundred and forty-one subjects (69.9%) had a negative familiar history for mental disorders, while 104 subjects (30.1%) had a positive one. Eighty-three subjects (24.1%) also reported a psychiatric disorder (anxiety or a mood disorder) with onset having occurred before the work-related stress. Eighty subjects (23.2%) had a history of severe physical disease (eg, cancer or another chronic/debilitating disease).
Post-traumatic stress symptoms
One hundred and sixteen subjects (33.9%) presented full mean cluster symptoms of PTSD (obtained by the TALS-SR). Sixty-eight subjects (36.4%) were women and 48 subjects (31%) were men (see Table 2).
Table 2. PTSD Prevalence Rates in the Sample (N = 345) Stratified on all Variables

Abbreviation: PTSD, post-traumatic stress disorder.*We applied the Student’s t-test.
Endorsement rates of each of the DSM-V PTSD criteria (obtained by the TALS-SR) were investigated, breaking the population down based on socio-demographic and work-related variables, but few relevant correlations emerged. Statistically significant scores emerged based upon criterion B (intrusion symptoms) (P = .014), criterion D (negative alterations in cognitions and mood) (P = .023), and in all symptom criteria combined (B, C, D, and E) (P = .006) in subjects with a positive family history for mental disorders (see Table 3). Further, higher rates were found for criterion D (P = .033) and in all criteria combined (P = .018) for subjects who presented a comorbid psychiatric disorder (see Table 4). Finally, breaking the sample down by age, statistically significant rates were found for criterion D (negative alterations in cognitions and mood) (P = .009) in subjects over 50 years old.
Table 3. DSM-V Single and Total Criteria’s Mean Scores ± SD (and Mean Ranks) Divided by Psychiatric Family History
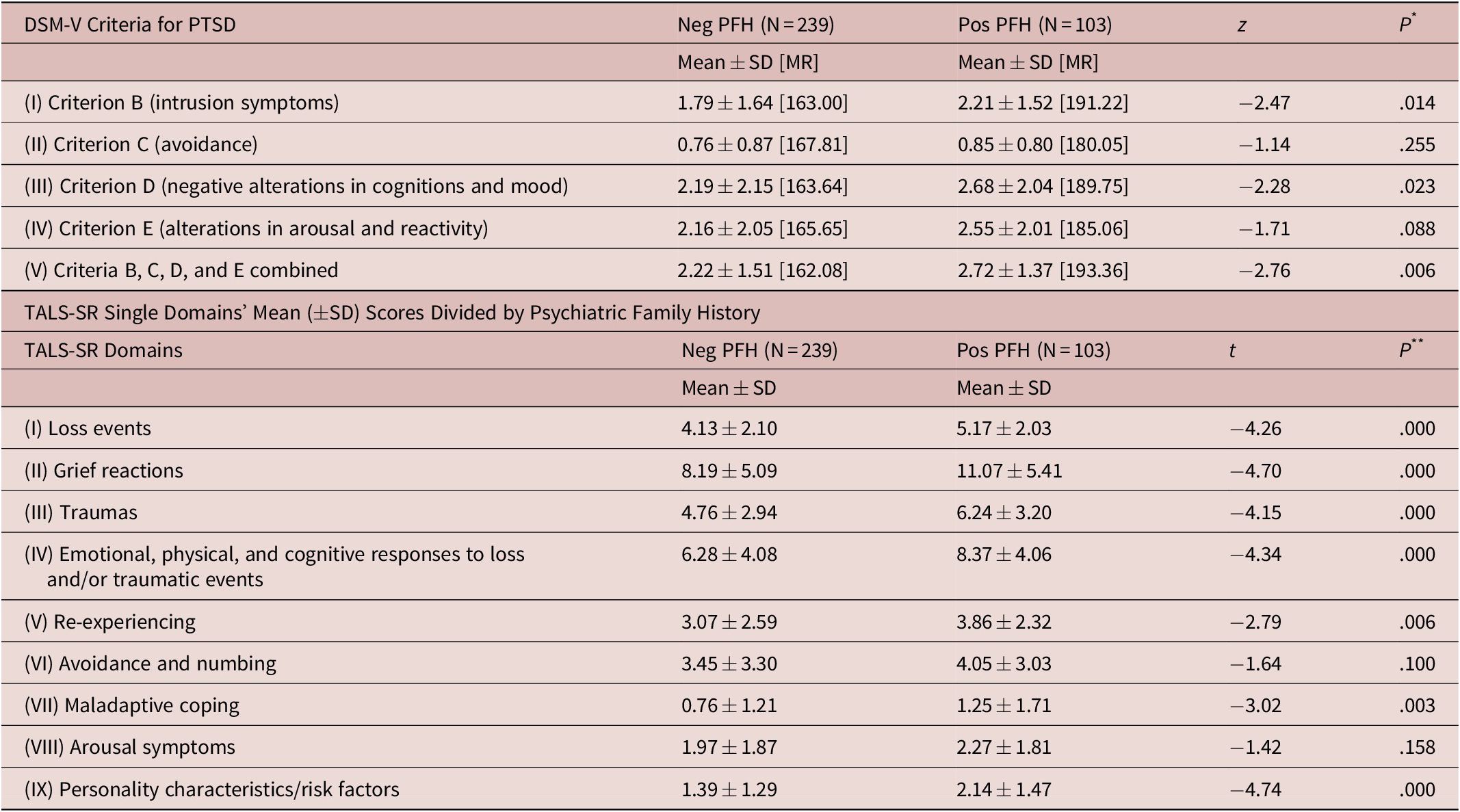
Abbreviations: PFH, psychiatric family history; PTSD, post-traumatic stress disorder; TALS-SR, Trauma and Loss Spectrum Self Report.*We used the Mann–Whitney U test.**We applied the Student’s t-test.
Table 4. DSM-V Single and Total Criteria’s Mean Scores ± SD (and Mean Ranks) Divided by Psychiatric Disorders
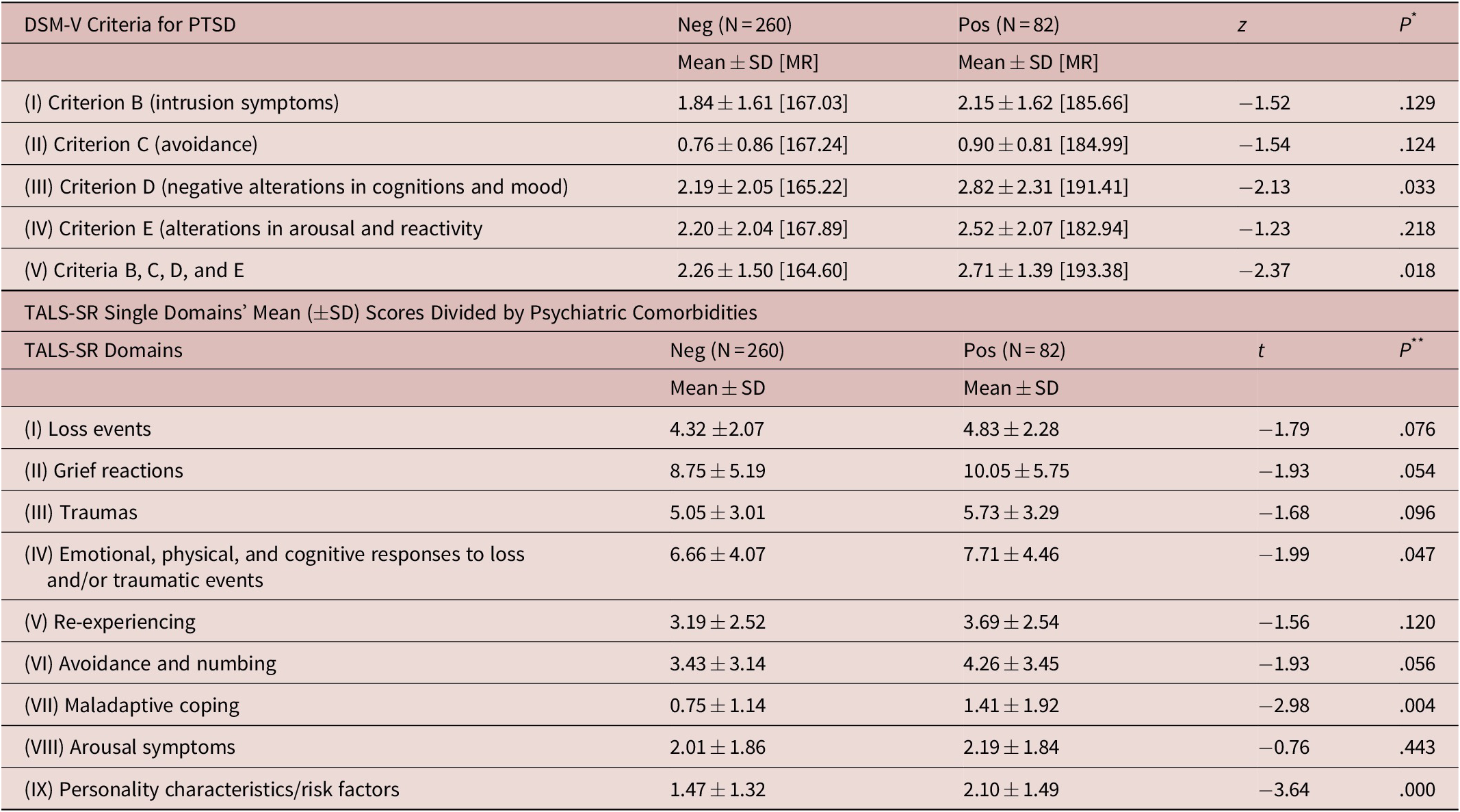
Abbreviation: PTSD, post-traumatic stress disorder; TALS-SR, Trauma and Loss Spectrum Self Repot.*We used the Mann–Whitney U test.**We applied the Student’s t-test.
When comparing the single TALS-SR domains in all subsamples, stratifying according to the same previously mentioned variables, various statistically significant relevant data emerged. Females reported significantly higher endorsement rates in the following domains: “loss events” (P = .000), “grief reactions” (P = .018), and “reactions to losses and traumatic events” (P = .011). As for age, the only significant difference that emerged was for endorsement rates of the “avoidance and numbing” domain (P = .046) that were higher in subjects over 50 years old. A positive family history for mental disorders was correlated with higher scores in almost all domains: “loss events” (P = .000), “grief reactions” (P = .000), “traumas” (P = .000), “reactions to losses and traumatic events”(P = .000), “re-experiencing” (P = .006), “maladaptive coping” (P = .003), and “personality characteristics/risk factors” (P = .000) (see Table 3). Similar results were evidenced when breaking the sample down based on psychiatric comorbidities: “reaction to losses and traumatic events” (P = .047), “maladaptive coping” (P = .004), and “personality characteristics/risk factors” (P = .000) in subjects with a history of mental disorders comorbidity (see Table 4).
Finally, patients with FM reported significantly higher scores in the first two TALS-SR domains: “loss events” (P = .048) and “grief reactions” (P = .041).
Education level, work-related characteristics, and physical comorbidities were not associated with any statistically significant correlations.
Discussion
The present study provides insight into the current situation in Italy, since it evaluates subjects exposed to different degrees of work-related stress over a 3-year period.
Comorbidity for a positive family history of mental disorders and comorbidity for personal mental disorders were related to higher scores in the core cluster symptoms of PTSD, intrusive thoughts, and negative alterations in cognition and mood as well as in almost all TALS domains. This result supports theories that identify familiar and personal vulnerability as being the greatest risk factors for the development of post-traumatic stress symptomatology.Reference Husky, Mazure and Kovess-Masfety 33 , Reference Dell’Osso, Corsi and Gesi 34
Having a debilitating physical illness, either acute or chronic, did not affect PTSD domain scores except for FM, which is not considered to be a physical illness of extreme severity. Nevertheless, several current studies suggest that there is a meaningful relationship between FM and the psychological symptoms of PTSD. This suggests the presence of a relationship between lifetime exposure to potentially traumatic events and lifetime post-traumatic stress symptoms in predisposed individuals. 35–37
An increased risk for developing PTSD symptoms also emerged in the female gender. In particular, women presented statistically significant rates of endorsement in TALS clusters associated with lifetime exposure to traumatic events: “loss events,” “grief reactions,” and “reactions to losses and traumatic events.” This highlights the increased vulnerability of females to traumas and their consequences. This has been discussed and confirmed in previous studies.Reference Carmassi, Corsi and Bertelloni 20 , Reference Chatzea, Sifaki-Pistolla, Vlachaki, Melidoniotis and Pistolla 29 , Reference Coppens, Van Wambeke and Morlion 36 , Reference Conversano, Carmassi and Bertelloni 37 Contrary to what has been reported in previous studies, the level of education does not seem to be protective in the development of a post-traumatic symptomatology.Reference Carmassi, Gesi and Corsi 27 , Reference Perrin, DiGande, Wheeler, Thorpe, Farfel and Brackbill 38 , Reference Mealer, Conrad and Evans 39
Finally, evaluating the sample population based on age, statistically significant higher endorsement rates were evidenced in subjects over 50 years old at criterion D which regards personal negative emotions about ourselves and the world surrounding. It seems that with aging subjects become more vulnerable to the depressive component of PTSD.Reference Daniels, Boehnlein and McCallion 40 , Reference Knight, Naaz, Stoica and Depue 41
This study’s results suggest that almost one-third of the subjects satisfied main cluster criteria for PTSD. This highlights how post-traumatic symptomatology is noteworthy in a workplace context.
These data corroborates the notion that the development of a PTSD is much more closely related to the subjective perception that the individual has of the traumatic event, as opposed to the objective characteristics of the event. The DSM-5 itself (APA, 2013) highlights the significance of repeated traumas. Repetitive exposure to distressing details of an event exacerbates it, and can be the determining factor in it being categorized as a traumatic index event (criterion A4, PTSD, DSM-5) paving the way for new considerations and broader approaches to PTSD.
In this way, subjects who experience minor traumas (such as work-related traumas which are not life-threatening) may present atypical or subthreshold manifestations that might be unrecognized as stress related. The TALS-SR fits into this context since it explores behaviors and personal characteristics that might also represent atypical manifestations of a stress response.
The systems that are currently in place have proven insufficient to prevent workplace trauma. People are often left without support within their job or from clinicians, while attempting to navigate the fallout from these experiences.Reference Gale, Mordukhovich, Newlan and McNeely 16
The authors believe that the dimensional approach to the TALS-SR can be used by clinicians alongside the SCID to detect not only the Axis I symptoms, but also the subthreshold ones and any atypical manifestations and characteristics that the SCID, due to its strictly categorical nature, fails to identify. 42–47 Given the dimensional nature of PTSD, this can be considered a particularly effective tool during the investigation and classification of occupational diseases.
Results of the current study should be interpreted in light of several limitations. First, the limited sample size cannot be said to have epidemiological value, despite it being one of the largest samples in literature. Second, this is a cross-sectional study without a control group. All subjects presented themselves at the Occupational Health Department because of persistent exposure to stress at the workplace. Finally, this study relied on self-reported data and not on structured clinical interviews.
Despite the aforementioned limitations and the fact that psychosocial hazards with different degrees of severity could interact with different mental disorders requiring different methods to preserve workers’ health and safety, this study suggests the importance of evaluating symptoms from a post-traumatic stress perspective. The risk of not doing so could result in attributing symptoms to other mental disorders and to underestimate the risk of working environments.
Conclusions
The ability of a self-assessment instrument to utilize a dimensional approach to capture symptoms that are not yet clinically evident could be useful from the perspective of preventive medicine in order to be aware of PTSD-like symptomatology in its earliest phases.
Nevertheless, further work is needed for both psychiatrists and occupational doctors to elucidate whether this study’s results can be confirmed on larger populations in order to extend the research field to apply evidence-based practice to work-related stress.
Acknowledgment
The authors would like to thank Mr. Alex Grey for handling English language revision process of this paper.
Disclosure
The authors report no conflicts of interest in this work.






