Introduction
The surgical treatment of the hearing loss secondary to otosclerosis or stapes malformations has improved dramatically since the first description of stapes mobilisation by French physician Boucheron, in 1880.Reference Daneshi and Jahandideh1 The introduction of new equipment, in association with technological enhancements, has led to the development of less invasive procedures and a lower incidence of complications.
More recent studies have demonstrated that the use of endoscopes in ear surgical procedures might provide better visualisation of the middle-ear structures as compared with the microscopic view, thereby allowing less invasive and less traumatic procedures. The first description of endoscope use in otology was reported by Mer et al., in 1967, who studied the anatomy of the middle ear in the temporal bones of human and animal cadavers.Reference Mer, Derbyshire, Brushenko and Pontarelli2 The first description of endoscopes used in otological procedures was published in 1982.Reference Nomura3 Initially, the endoscope was proposed as an adjuvant tool for the operating microscope, to better assess the presence of residual disease in revision mastoidectomy procedures.Reference Nomura3 Since then, the promising preliminary results of surgical procedures using an endoscopic view led to increasing interest in endoscopic-assisted ear surgery.Reference Kozin, Gulati, Kaplan, Lehmann, Remenschneider and Landegger4
New optic equipment and surgical tools, adaptations in surgical techniques, and more detailed descriptions of endoscopic anatomy of the middle ear brought further possibilities for endoscopic otological surgery. In comparison with the conventional microscopic view, endoscopic approaches seem to allow greater exposure of hard-to-reach structures of the middle ear, with minimal bone drilling, allowing more physiological and less destructive techniques, with similar functional outcomes.Reference Daneshi and Jahandideh1,Reference Marchioni, Soloperto, Villari, Tatti, Colleselli and Genovese5,Reference Iannella and Magliulo6 However, papers describing the outcomes of endoscopic stapes surgery and their complications are scarce, and consist of case series with small numbers of patients. Therefore, this study aimed to review the literature on endoscopic stapes surgery, focusing on surgical techniques, approaches, audiological outcomes and complications.
Materials and methods
We performed systematic searches of the literature in PubMed, Web of Science and Scopus databases, from July 2017 to February 2018. We used the following search string, without any additional filters: (stape* AND (surgery OR surgical OR procedure* OR approach*) AND endoscop*). We selected papers that describe the outcomes of stapes surgery performed using a fully endoscopic view. The resulting studies were exported to reference manager software (Mendeley; Elsevier, Amsterdam, Netherlands). Duplicate studies were excluded both manually and using the Mendeley ‘check for duplicates’ tool.
The inclusion criteria were defined as: (1) studies involving patients subjected to stapes surgery using an endoscopic view; and (2) studies reporting objective post-operative hearing outcomes. We excluded studies reporting outcomes of middle-ear surgical procedures other than stapes surgery (malleus, incus or the tympanic membrane) and studies where the endoscope was used as a complementary tool (to ensure complete eradication of squamous epithelial matrix when performing mastoidectomy procedures or to confirm graft positioning during tympanoplasty procedures).
We initially selected relevant articles by reading the title and abstracts. The remaining papers were then read in full. All authors independently read the articles and extracted relevant information; discrepancies were resolved by mutual consensus. We classified the studies according to the impact factor of the journal in which they were published, based on the Journal Citation Reports classification (Clarivate Analytics, Philadelphia, Pennsylvania, USA).
Parameters investigated
The information we extracted from the selected papers included: (1) operating time; (2) early and late complications (such as perilymphatic ‘gusher’, chorda tympani nerve injury, tympanic membrane perforation, incus subluxation, floating footplate, vertigo, facial nerve paralysis, hypogeusia and prosthesis dislocation); (3) whether drilling of the posterior-superior part of the external auditory canal was required; (4) details of how the stapes superstructure was removed; (5) details of how the footplate was perforated; and (6) pre- and post-surgical audiometric assessment findings.
Results
The database search resulted in a total of 281 articles. After initial screening and full-text reading of relevant articles, 14 studies were finally included in our analysis. Figure 1 depicts the selection process of relevant articles.

Fig. 1. Flowchart of articles included and excluded in the literature search.
Of the 42 studies read in full, 28 were excluded for several reasons: 1 article was a short communication; 2 were descriptive technique studies, with no comparison of pre- or post-operative audiological results; 3 were animal model studies; 2 did not contain clinical data (1 comprised a histopathological description; 1 was an experimental study); 10 included patients with chronic otitis media; 1 described the use of endoscopes in sinus surgery; and 1 did not include patients subjected to stapes surgery. The other eight studies did not describe audiometric outcomes and were also excluded.
From the 14 selected studies, 5 were prospective and 9 were retrospective. One study was published in 1999, and the remaining 13 were all published after 2010. Regarding the journals in which the studies were published, one (7.1 per cent) was published in a journal with an index of less than 1 (0.82), six (42.9 per cent) ranged from 1.1 to 2.0, and six (42.9 per cent) had an impact factor of over 2.01; one paper (7.1 per cent) was published in a journal not indexed by the Journal Citation Reports.
All studies reported the post-operative outcomes as residual air–bone gap; nine reported the mean pre-operative air–bone gap. The selected studies included a total of 282 ears subjected to stapes surgery using an endoscopic-only view. The age of patients ranged from 6 to 87 years; 126 patients were men and 149 were women (no information regarding sex was provided for 7 patients in the study by TarabichiReference Tarabichi7). Seven studies described the mean surgery time using the endoscopic view. The type of anaesthesia varied among studies: five used general, two used sedation and local anaesthesia, and three used only local anaesthesia. The surgical techniques are described in Table 1.Reference Daneshi and Jahandideh1,Reference Marchioni, Soloperto, Villari, Tatti, Colleselli and Genovese5–Reference Sproat, Yiannakis and Iyer17
Table 1. Surgical techniques

N/A = not available
Five articles compared the outcomes of the same surgical technique using an endoscopic versus an operating microscopic view. Those studies compared both techniques in terms of surgery duration, auditory outcomes (Table 2),Reference Daneshi and Jahandideh1,Reference Iannella and Magliulo6,Reference Kojima, Komori, Chikazawa, Yaguchi, Yamamoto and Chujo11,Reference Surmelioglu, Ozdemir, Tarkan, Tuncer, Dagkiran and Cetik16,Reference Sproat, Yiannakis and Iyer17 and rates of surgical and late complications (Figure 2). The 5 articles included a total of 131 patients who underwent stapes surgery using an endoscope and 126 patients who were operated on using a microscope. Among those patients, we observed that the prevalence of transient vertigo (odds ratio = 0.543; 95 per cent confidence interval (CI) = 0.371–0.9303; p = 0.026) and chorda tympani injury (odds ratio = 0.27; 95 per cent CI = 0.1216–0.6018; p = 0.001) was significantly lower among patients operated on using an endoscope as compared with a microscope. We did not observe significant differences in the prevalence of tympanic membrane perforation or facial nerve paralysis between the two groups.
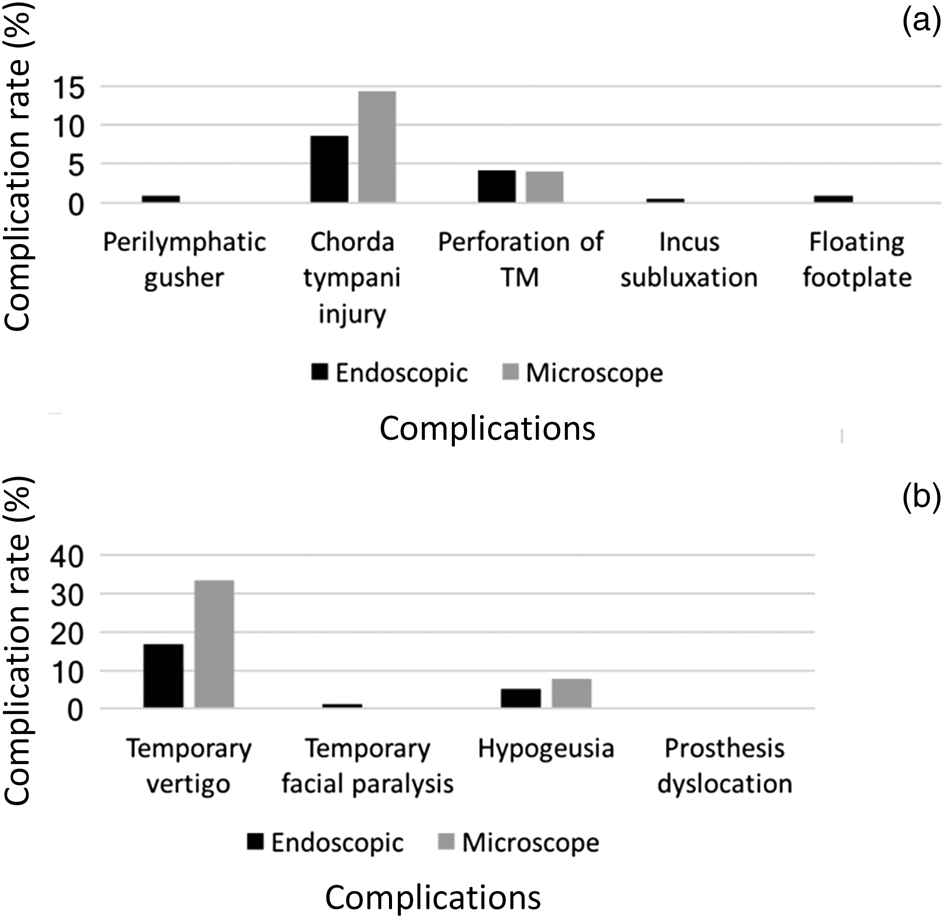
Fig. 2. Comparison of rates for (a) surgical complications and (b) late complications for stapes surgery performed using an endoscope versus an operating microscope. TM = tympanic membrane
Table 2. Summary of published literature comparing audiological outcomes after endoscopic and microscopic stapes surgery

ABG = air–bone gap; M = male; F = female; pre-op = pre-operative; N/A = not available; post-op = post-operative; SD = standard deviation
Discussion
Advantages of endoscopic surgery
Several authors have described previously that the use of endoscopes in the surgical management of otosclerosis leads to better visualisation of the middle-ear structures, thereby allowing less traumatic and invasive surgery, and potentially better audiological outcomes (Table 3).Reference Daneshi and Jahandideh1,Reference Marchioni, Soloperto, Villari, Tatti, Colleselli and Genovese5–Reference Kojima, Komori, Chikazawa, Yaguchi, Yamamoto and Chujo11,Reference Naik and Nemade13–Reference Hunter, Zuniga, Leite, Killeen, Wick and Ramirez18
Table 3. Summary of published literature regarding audiological outcomes after endoscopic stapes surgery

Pre-op = pre-operative; ABG = air–bone gap; N/A = not available
Bennett et al.Reference Bennett, Zhang, Labadie and Noble19 corroborated those assumptions by demonstrating that endoscopes allow better exploration of several middle-ear regions – except the antrum – as compared with the microscopic view. In addition, Daneshi and Jahandideh demonstrated several benefits of using the endoscopic approach for stapes surgery, including the decreased surgery time, the possibility of performing the whole surgery with less drilling and trauma, and audiological results that are similar to those achieved using the operating microscope.Reference Daneshi and Jahandideh1
These advantages further support the association of endoscope use with less risk of intra-operative chorda tympani nerve injury and a decreased prevalence of post-operative transient vertigo. However, only a few studies compared the audiological outcomes of microscopic versus endoscopic techniques in stapes surgery (Table 2).
Disadvantages of endoscopic surgery
Although generally associated with less trauma, the use of endoscopes for stapes surgery can be challenging, especially for surgeons who are not experienced in otological surgery. The one-handed surgical technique is probably the most critical issue. Excessive bleeding may preclude the use of endoscopes; therefore, attention to haemostasis is essential to complete the procedure with one hand alone. Furthermore, the two-dimensional image provided by the endoscope may lead to loss of stereoscopic vision (loss of depth perception). Stereoscopic vision is fundamental for ear surgery, and some of the crucial steps of stapes surgery (e.g. cutting the stapedial limb or tightening the wire) require an adequate sense of depth.
Other disadvantages include the need for additional physician training and the cost of equipment. Experienced otolaryngologists who routinely perform nasal endoscopy or functional endoscopic sinus surgery are more likely to master these necessary skills in a shorter time. However, otological surgeons who lack extensive endoscopic training may find it difficult to perform these procedures using endoscopes. The availability of equipment is not an issue, as most hospitals do have the necessary equipment available in the operating theatres, and the required instruments are minor modifications of existing ones. It has been previously suggested that the extra costs associated with new equipment and instruments are justified in the long-term, when one considers the shorter surgery time and the reduced number of in-patient days associated with less traumatic procedures;Reference Tarabichi7 however, our findings do not robustly support such an argument. Further prospective studies that include a larger sample of patients operated on by surgeons who are experienced in fully endoscopic ear surgery may corroborate those assumptions.
Surgical considerations
All studies reviewed were in concordance that the endoscopic technique has advantages over conventional techniques. These advantages include an excellent view of the oval window niche and anterior crus, allowing less manipulation of the chorda tympani and less bone drilling.
Daneshi and Jahandideh,Reference Daneshi and Jahandideh1 Kojima et al.Reference Kojima, Komori, Chikazawa, Yaguchi, Yamamoto and Chujo11, and Iannella and Magliulo,Reference Iannella and Magliulo6 demonstrated that using the endoscope may allow less external auditory canal bone removal as compared with surgery performed using the microscope, leading to lower rates of post-operative pain. However, our review of the literature revealed that, in 10 studies (71.4 per cent), the authors either routinely or occasionally removed the scutum. Thus, these results suggest that, despite the better view provided by the endoscope, manipulation of the external ear canal and of the annulus is still needed in a significant proportion of cases.
Regarding surgery duration, the selected studies described inconsistent results. Iannella and MagliuloReference Iannella and Magliulo6 showed reduced operation time with the microscopic technique (36.5 vs 45.0 minutes, p = 0.01), while Daneshi et al.Reference Daneshi and Jahandideh1 demonstrated reduced surgery time with the endoscopic approach (31.78 vs 54.33 minutes, p = 0.05). Although most studies generally reported that the surgical procedures performed with an endoscope were faster than those performed with a microscope, the studies do not provide sufficient data for analysis to determine whether such a statement is true. In this regard, most of the studies only provided average surgery time, but no range, standard deviations or medians. Furthermore, the learning curve of endoscopic stapes surgery may have had an additional impact on surgery time. In this regard, Iannella and MagliuloReference Iannella and Magliulo6 showed a decrease in operation time from 52.5 minutes in the first three months, to 35.9 minutes after four months. There was no statistical difference between surgery times for each approach in the last period of the study.
Auditory outcomes
The auditory outcome was generally reported among studies as the air–bone gap size. In those studies, 116 of 160 ears (73 per cent) had a residual air–bone gap of less than 10 dB. Also, 199 of 208 ears (96 per cent) had a residual air–bone gap of less than 20 dB after surgical treatment of stapes fixation. There were no significant differences in the mean residual air–bone gap in patients who underwent endoscopic surgery as compared with microscopic approaches among the studies.
Although those results are promising, the study of Vincent et al.,Reference Vincent, Sperling, Oates and Jindal20 which used a computerised database to review the auditory results of 3050 stapedotomies performed over 14 years, demonstrated contradictory findings. Those authors reported that 94.2 per cent of their patients had post-operative air–bone gaps of less than 10 dB. However, it must be considered that the endoscopic-assisted techniques may require extra training and have different learning curves. Thus, to better assess the real differences between endoscopic and microscopic approaches for stapes surgery, further well-designed, randomised, prospective studies, which include a large number of patients undergoing procedures performed by experienced surgeons who are extensively trained in endoscopic ear surgery, are warranted.
Complications
Four studies showed a smaller incidence of chorda tympani nerve injury in the endoscopic surgery group as compared with the microscopic technique group. Such a difference may be explained by the better view of the middle-ear structures. Iannella and Magliulo showed reduced post-operative pain in patients who underwent endoscopic approaches as compared with traditional microscopic surgery (90 per cent and 75 per cent of pain absence, respectively).Reference Iannella and Magliulo6 The same study demonstrated similar rates of dizziness on the first day after surgery in both groups, which affected up to 80 per cent of patients. Dursun et al.Reference Dursun, Özgür, Terzi, Oğurlu, Coşkun and Demirci14 reported tympanic membrane perforation in three patients who underwent endoscopic stapes surgery.
Endoscopy versus operating microscope
The first study to report the comparison between endoscopic stapes surgery and conventional stapes surgery using an operating microscope was performed by Kojima et al., in 2014.Reference Kojima, Komori, Chikazawa, Yaguchi, Yamamoto and Chujo11 In their study, 15 patients underwent endoscopic surgery (15 ears) and 35 patients underwent microscopic surgery (41 ears). The authors found no differences in operating time and post-operative air–bone gap between the two techniques (air–bone gap of less than 20 dB in 93.3 per cent of the endoscopic group and in 97.5 per cent of the microscopic group). Only one patient in the endoscopic group complained of facial palsy, which fully recovered one month after the procedure. No patient complained of dysgeusia in the endoscopic group, while four patients reported this complaint in the microscopic group.
Daneshi and Jahandideh compared the results of 19 patients who underwent endoscopic stapes surgery versus 15 patients who underwent microscopic surgery.Reference Daneshi and Jahandideh1 They found similar audiological results for both techniques (94.71 per cent in the endoscopic group vs 93.33 per cent in the microscopic group). The authors reported a shorter surgery duration in the endoscopic group than the microscopic group (p < 0.05), and higher patient satisfaction rates in the endoscopic group as compared with the microscope group (p < 0.05). No cases of dead ear, facial nerve palsy or dysgeusia were observed.Reference Daneshi and Jahandideh1
In 2016, Iannella and Magliulo found no statistical differences in the audiological outcomes following endoscopic or microscopic approaches (20 patients in each group).Reference Iannella and Magliulo6 No cases of facial palsy were reported. Four patients in the endoscopic group and five patients in the microscopic group reported transient dysgeusia. The authors also found that total operative time was higher in the endoscopic group compared to the microscopic group (p = 0.01), which might be explained by the lack of surgeon experience for the first cases. Additionally, they observed that total operative duration decreased over time in the endoscopic group (potentially related to the learning curve), but remained similar in the microscopic group over the study period.Reference Iannella and Magliulo6
Iannella and Magliulo,Reference Iannella and Magliulo6 and Surmelioglu et al.Reference Surmelioglu, Ozdemir, Tarkan, Tuncer, Dagkiran and Cetik16 reported statistically significant differences in total operative times between the two techniques (p = 0.033). However, Surmelioglu et al. found that total operative time was shorter in the endoscopic group. Nevertheless, they observed a more significant air–bone gap difference from the pre- to the post-operative period in the endoscopic stapedotomy group (p = 0.023).
Finally, Sproat et al.Reference Sproat, Yiannakis and Iyer17 found that 79 per cent of both endoscopic and microscopic groups had an air–bone gap of less than 10 dB HL. However, the air–bone gap closure did not vary significantly between the two groups. Furthermore, no cases of vertigo, facial nerve palsy or sensorineural hearing loss were reported.
Conclusion
The few available studies demonstrate that endoscopic stapes surgery is safe and provides similar audiological results when compared to microscopic procedures. We recommend that additional well-designed, randomised, prospective studies are conducted. These should include a large number of patients undergoing procedures performed by experienced surgeons who are extensively trained in endoscopic ear surgery. This will allow better assessment of the auditory outcomes and complications rates for endoscopic stapes surgery versus the traditional approach using an operating microscope.
Acknowledgement
This study was partly financed by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (‘CAPES’), Finance Code 001.
Competing interests
None declared







