Introduction
According to the Diagnostic and Statistical Manual of the American Psychiatric Association (DSM-IV; APA, 1994), a diagnosis of panic disorder (PD) requires the experience of recurrent panic attacks, identified via the sudden onset of intense apprehension or fear, accompanied by at least four out of a list of ten bodily and three cognitive symptoms. The conceptualization of PD has changed considerably from DSM-III (APA, 1980) to DSM-IV, but the list of panic attack symptoms (PAS) has only minimally changed. In DSM-IV, this list comprises (1) palpitations, pounding heart, or accelerated heart rate, (2) sweating (3) trembling or shaking, (4) sensations of shortness of breath or smothering, (5) feeling of choking, (6) chest pain or discomfort, (7) nausea or abdominal distress, (8) feeling dizzy, unsteady, lightheaded, or faint, (9) derealization (feelings of unreality) or depersonalization (being detached from oneself), (10) fear of losing control or going crazy, (11) fear of dying, (12) paresthesias (numbness or tingling sensations), (13) chills or hot flushes. The recently published DSM-5 adopted this symptom list with only one minor change in wording (chills or heat sensations).
By this definition of a panic attack, all symptoms are treated as equally important. However, some symptoms are endorsed consistently more frequently than others. For example, in the Cross-National Panic Study (CNPS; Briggs et al. Reference Briggs, Stretch and Brandon1993), a Japanese study (Shioiri et al. Reference Shioiri, Someya, Murashita and Takahashi1996), a Spanish study (Segui et al. Reference Seguí, Salvador-Carulla, Garcia, Canet, Ortiz and Farré1998), and a German study (Andor et al. Reference Andor, Glöckner-Rist, Gerlach and Rist2008), at least 83% of the patients reported palpitations, and more than 71% shortness of breath. On the other hand, paresthesias were endorsed by no more than 53% of the patients. These differences in the endorsement rates of the symptoms and their postulated emergence from different physiological systems have stimulated both the search for panic patient subgroups and for a dimensional structure of PAS. While subtyping approaches partition PD patients according to the predominance of certain PAS (cf. review by Kircanski et al. Reference Kircanski, Craske, Epstein and Wittchen2009), dimensional analyses focus on relating PAS to underlying dimensions. Understanding the dimensional structure of PAS is not only important for the discussion of necessary changes for the PAS list (cf. Craske et al. Reference Craske, Kircanski, Epstein, Wittchen, Pine, Lewis-Fernández and Hinton2010) by either reducing the number of PAS, or by adopting more PAS (i.e. to accommodate culture-bound varieties of PAS, cf. Lewis-Fernandez et al. Reference Lewis-Fernandez, Hinton, Laria, Patterson, Hofmann, Craske, Stein, Asnaani and Liao2010). It also allows specifying current research findings on the connection between PD and related risk factors, as described below.
We identified 11 studies of patients with PD that reported dimensional solutions of PAS as listed in DSM-III, DSM-III-R and DSM-IV. Four studies out of these 11 employed a binary answer format for PAS, but nevertheless subjected these to principal component analysis (PCA; De Beurs et al. Reference De Beurs, Garssen, Buikhuisen, Lange, Balkom and Dyck1994; Bandelow et al. Reference Bandelow, Röthemeyer, Sievert, Hajak and Rüther1996; Shioiri et al. Reference Shioiri, Someya, Murashita and Takahashi1996; Neerakal & Srinivasan, Reference Neerakal and Srinivasan2002). Because PCA has been found to produce biased dimensional solutions when applied to binary variables (e.g. Kolenikov & Angeles, Reference Kolenikov and Angeles2009), these studies are not included in the following overview. Briggs et al. (Reference Briggs, Stretch and Brandon1993) also employed a binary format and analysed their data with PCA, but fortunately Roberson-Nay & Kendler (Reference Roberson-Nay and Kendler2011) re-analysed these data with appropriate statistical methods.
Supplementary Table S1 lists the characteristics and results of the remaining seven studies that analysed PAS reports of patients with a diagnosis of PD (with or without agoraphobia). With the exception of Briggs et al. (Reference Briggs, Stretch and Brandon1993), they employed severity ratings of PAS with several answer categories. These ratings were applied to the last attack (Briggs et al. Reference Briggs, Stretch and Brandon1993; Sarp et al. Reference Sarp, Ali, Hatice, Ahmet and Abanoz2010) or typical full panic attacks (Meuret et al. Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006; not specified in the remaining four studies). While Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006) and Roberson-Nay & Kendler (Reference Roberson-Nay and Kendler2011) used statistical methods which are not biased by non-normal answer distributions, the remaining five studies employed PCA, which may produce biased results if linearity and normality requirements are not met. The studies also varied with respect to the nationality of the patients, the composition of the patient sample, the mode of assessment of the panic symptoms and the number of symptoms subjected to the dimensional analyses.
Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006) identified a cardio-respiratory factor associated with six PAS, defined by high loadings of dyspnoea and chest pain, but also including paresthesias and fear of dying. The second ‘autonomic/somatic’ factor comprised the remaining bodily symptoms. The third ‘cognitive’ factor was constituted by the fears of going crazy and losing control, and also derealization/depersonalization. By contrast, Roberson-Nay & Kendler (Reference Roberson-Nay and Kendler2011) reported a pure ‘respiratory’ factor, which resembles the cardio-respiratory factor of Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006), but did not include tachycardia. Instead tachycardia was allocated to a second factor which corresponds to Meuret et al.'s (2006) autonomic/somatic factor with respect to the other criteria loading on it. Thus, the allocation of tachycardia is the only major inconsistency, despite the considerable differences between these two studies in sample composition and answer categories (cf. Supplementary Table S1): both identified three dimensions which are largely equivalent.
Cox et al. (Reference Cox, Swinson, Endler and Norton1994) also found a ‘cardiorespiratory’ component that is virtually identical to the cardio-respiratory factor of Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006) with the exception that paresthesias was assigned to a separate ‘dizziness’ component. This component is comprised of all the criteria that belong to the autonomic/somatic factor of Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006). The third factor of Cox et al. (Reference Cox, Swinson, Endler and Norton1994) combines fear of losing control (0.82), fear of going crazy (0.82) and also feelings of unreality (0.47) and thus corresponds well to the cognitive factor identified by Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006). The remaining studies claimed more than three dimensions, rendering a direct comparison of their factor structures with those of Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006) and Roberson-Nay & Kendler (Reference Roberson-Nay and Kendler2011) difficult. Segui et al. (Reference Seguí, Salvador-Carulla, Garcia, Canet, Ortiz and Farré1998) identified a cardio-respiratory factor largely identical to the factor of Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006), but not including choking. The symptoms combined in Meuret et al.'s (2006) ‘autonomic/somatic’ factor appear in the Segui et al. (Reference Seguí, Salvador-Carulla, Garcia, Canet, Ortiz and Farré1998) study distributed over three components comprised of vestibular symptoms, other autonomic symptoms and ‘general arousal’. However, despite different numbers of dimensions and consequently different allocations of symptoms, most of the attack criteria covary in Segui et al. (Reference Seguí, Salvador-Carulla, Garcia, Canet, Ortiz and Farré1998) as in the models of Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006) and Roberson-Nay & Kendler (Reference Roberson-Nay and Kendler2011). Only with respect to the cognitive symptoms does the Segui et al. (Reference Seguí, Salvador-Carulla, Garcia, Canet, Ortiz and Farré1998) study differ. It located fear of going crazy and derealization/depersonalization on different factors.
Márquez et al. (Reference Márquez, Seguí, García, Canet and Ortiz2001) applied the same list of 14 DSM-III-R panic attack criteria as Segui et al. (Reference Seguí, Salvador-Carulla, Garcia, Canet, Ortiz and Farré1998). They identified a first factor that overlaps with the autonomous/somatic factor of Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006), but also includes palpitations. The second factor is defined by respiratory symptoms, a third factor by vestibular symptoms, and a fourth factor includes nausea and depersonalization-derealization. By contrast to most other studies, fear of dying and of going crazy do not define a cognitive factor, but were allocated to the respiratory factor. A Turkish study (Sarp et al. Reference Sarp, Ali, Hatice, Ahmet and Abanoz2010) found a respiratory-cardiac factor, an autonomic/somatic factor and a cognitive factor, rather similar to the dimensional solution offered by Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006).
Pio-Abreu et al. (Reference Pio-Abreu, Ramalheira and Valente1998) only studied the disaggregated DSM-IV bodily symptom criteria. They excluded the cognitive symptoms from the dimensional analysis. Most importantly, their five-component-solution separated the respiratory and cardiovascular symptoms present on the first factor of Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006) by assigning them to different components. The symptoms from the autonomic/somatic factor of Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006) are also distributed across two separate factors. Thus, the covariation among respiratory symptoms on the one hand, autonomic/somatic symptoms on the other hand is at least partly preserved, despite the more differentiated structure which is obtained with the disaggregated criteria and a further expanded symptom list.
To summarize, the model suggested by Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006) and by Roberson-Nay & Kendler (Reference Roberson-Nay and Kendler2011) for the Briggs et al. (Reference Briggs, Stretch and Brandon1993) data is largely in accord with the results from several other studies with different assessment and statistical methods. However, several of the symptoms appear only loosely tied to particular dimensions: While a respiratory symptom complex is consistently found, the cardiovascular symptom criteria are inconsistently allocated to different components. Moreover, a vestibular factor, defined by the symptoms of faintness and dizziness, is found in several of the studies, while Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006) subsumed these symptoms under the autonomic/somatic factor.
Our first goal for this study was to further clarify the dimensional structure of panic attack symptoms. We will present a dimensional analysis for a sample of German patients with PD with agoraphobia. We followed the strategy of Pio-Abreu et al. (Reference Pio-Abreu, Ramalheira and Valente1998), confining this analysis to the ten bodily DSM-IV PAS. Cognitive models consider bodily PAS and catastrophic cognitions as functionally different components of panic attacks and postulate that the perception of bodily PAS activates catastrophic cognitions, which in turn provokes or amplifies further panic symptoms (e.g. Clark, Reference Clark1986). Pio-Abreu et al. (Reference Pio-Abreu, Ramalheira and Valente1998) argue that simultaneous factor analyses or cluster analyses of both bodily and psychological PAS are not appropriate for this ‘vicious circle’ model, as the cognitive symptoms are qualitatively different from the bodily symptoms. Thus, we first determined the factorial structure of the bodily symptoms of panic attacks. We hypothesized a two-factor solution consisting of a respiratory and a vestibular/mixed somatic factor. We tested whether a joint respiratory-cardiac dimension or two separated dimensions better represent the respiratory and cardiac symptoms. A second aim was to test the association between the resulting dimensions and catastrophic cognitions in anxiety situations. We expected strong associations between respiratory symptoms and ‘fear of choking to death’, and cardiac symptoms and ‘fear of a cardiac infarct’. We expected less specific relationships between ‘fear of going crazy’ or ‘fear of losing control’ and any of the bodily symptoms of a panic attack dimensions. These two cognitive symptoms either formed a factor of their own or did not reach high loadings when subsumed under a bodily symptom factor in the previous analyses.
Reiss et al. (Reference Reiss, Peterson, Gursky and McNally1986) defined anxiety sensitivity as ‘beliefs that the experience of anxiety/fear causes illness, embarrassment or additional anxiety’ (p. 1). Anxiety sensitivity predicts the development of panic attacks (Schmidt et al. Reference Schmidt, Lerew and Jackson1997, Reference Schmidt, Zvolensky and Maner2006). Specifically the subscale ‘physical sensations’ is associated with the course of PD (Pérez Benitez et al. Reference Pérez Benítez, Israel, Tracie, Susan, Richard, Ingrid, Holly, Maria and Martin2009) and the risk of developing panic attacks (Zinbarg et al. Reference Zinbarg, Brown, Barlow and Rapee2001; Schmidt et al. Reference Schmidt, Zvolensky and Maner2006). Similarly, the construct ‘fear of suffocation’, is not only linked to a higher rate of panic attacks in the past, but also to a higher risk of experiencing experimentally provoked (breathing through a narrow straw) panic (Taylor & Rachman, Reference Taylor and Rachman1994). In a student sample, both anxiety sensitivity and suffocation fear were correlated with anxiety and self-reported bodily sensations experienced during experimental carbon dioxide challenges (hyperventilation into a paper bag), but suffocation fear was the better predictor (McNally & Eke, Reference McNally and Eke1996). Our third research question concerned the relationship of anxiety sensitivity to the bodily symptom dimensions. Our fourth research aim was to examine the relationship of fear of suffocation to the bodily symptom dimensions, especially to a respiratory symptom dimension.
Method
Participants and procedure
Outpatients diagnosed with PD with agoraphobia (N = 369) were recruited in eight German treatment centres as part of a multicentre trial named ‘Mechanisms of Action in cognitive behaviour therapy (MAC)’. Participants were screened, signed an informed consent, and were examined in a diagnostic appointment to ascertain if they met the following inclusion criteria: (1) age 18–65 years, (2) a current primary diagnosis of PD with agoraphobia according to DSM-IV-TR, (3) a clinical interview score ⩾18 on the structured interview for the Hamilton Anxiety Rating scale (Shear et al. Reference Shear, Vander Bilt, Rucci, Endicott, Lydiard, Otto, Pollack, Chandler, Williams, Ali and Frank2001), (4) a Clinical Global Impression scale (CGI) score ⩾4, (5) ability to regularly attend treatment sessions. Exclusion criteria were (1) psychotic or bipolar I disorder, (2) substance abuse or dependence (alcohol, benzodiazepines or other psychoactive substances), (3) current suicidal intent, (4) borderline personality disorder, (5) current psychotherapeutic or psycho-pharmacological treatment, and (6) medical contraindications to exposure-based cognitive behavioural therapy (CBT; for more details see Gloster et al. Reference Gloster, Wittchen, Einsle, Höfler, Lang, Helbig-Lang, Fydrich, Fehm, Hamm, Richter, Alpers, Gerlach, Ströhle, Kircher, Deckert, Zwanzger and Arolt2009, 2011).
All measures considered in our study were measured during the initial diagnostic appointment (Anxiety Sensitivity Index and Claustrophobia Questionnaire) and baseline assessment (symptoms of a panic attack and Agoraphobic Cognitions Questionnaire), both of which preceded the beginning of the treatment. Participants were seated in front of a computer for the presentation and answering of the measures. Missing data were minimized (N = 8) by a computerized feedback algorithm that alerted patients not to skip items (Gloster et al. Reference Gloster, Wittchen, Einsle, Höfler, Lang, Helbig-Lang, Fydrich, Fehm, Hamm, Richter, Alpers, Gerlach, Ströhle, Kircher, Deckert, Zwanzger and Arolt2009). The bodily PAS answers were missing completely for one participant. For all others (N = 7), only singular items were missing. Nineteen patients were first assigned to a waiting control group before receiving therapy and answered the questionnaires of the pre-assessment twice. In order to avoid any influence of the repeated assessments on our results, only the first measurement was included in the analyses reported here resulting in the remaining 350 patients. The characteristics of the sample are listed in Table 1.
Table 1. Sample characteristics with respect to demographics and disorder (N = 350)
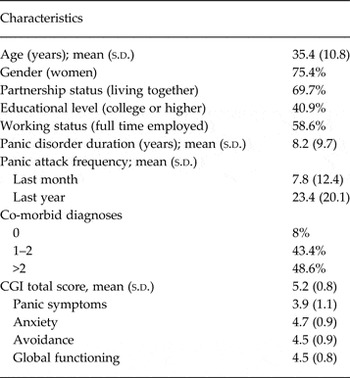
CGI (Clinical Global Impression scale) ranging from 1 (normal) to 7 (amongst the most severely ill patients).
Measures
Panic attack bodily symptoms
Participants rated how strongly (0 = not at all, to 4 = extremely) they had experienced each of the ten DSM-IV-TR bodily PAS during a recent typical panic attack.
Agoraphobic Cognitions Questionnaire (ACQ)
The ACQ (Chambless et al. Reference Chambless, Caputo, Bright and Gallagher1984) is a self-report-questionnaire designed to capture catastrophic cognitions activated during anxiety situations. It contains 14 items rated on a 5-point scale (1, thought never occurs to 5, thought always occurs). Four of the ACQ items were selected to assess the fear cognitions listed among the DSM-IV panic attack criteria: item no. 4 ‘I will have a heart attack’ and item no. 5 ‘I will choke to death’ were substituted for the less specific ‘fear of dying’ criterion. Item no. 8 ‘I will not be able to control myself’ corresponds to the ‘fear of loss of control’ criterion. Finally, item no. 11, ‘I am going to go crazy’ corresponds to the criterion ‘fear of going crazy’.
Anxiety Sensitivity Index (ASI)
The ASI (Reiss et al. Reference Reiss, Peterson, Gursky and McNally1986; German version by Alpers & Pauli, Reference Alpers and Pauli2001) assesses the tendency to fear anxiety-related symptoms (e.g. increased heart rate, sweating) because of their perceived aversive physical, social, or mental consequences. The 16 phrases (e.g. ‘It scares me when I feel faint’) are rated on 5-point scales (0, very little to 4, very much). Previous studies reported inconsistent results regarding the dimensional structure of the ASI (see meta-analysis by Olatunji & Wolitzky-Taylor, Reference Olatunji and Wolitzky-Taylor2009; Naragon-Gainey, Reference Naragon-Gainey2010). Therefore we investigated the factorial structure of this measure anew in our patient sample with nonlinear confirmatory factor analyses (CFA). The statistically and substantively most convincing model comprised three anxiety sensitivity dimensions. This is in accordance with the model originally reported by Zinbarg et al. (Reference Zinbarg, Barlow and Brown1997). The dimensions were labelled ‘physical concerns’ (3, 4, 6, 8–11, 14), ‘mental incapacitation concerns’ (2, 12, 15, 16) and ‘social concerns’ (1, 5, 13). The model had acceptable model fit [Comparative Fit Index (CFI) = 0.95, Tucker–Lewis Index (TLI) = 0.93, Root Mean Square Error of Approximation (RMSEA) = 0.09) and after the inclusion of two residual correlations between similar items (3–4 and 6–9) no remaining significant residual correlation. All of the items yielded factor loadings ⩾0.53. The factor inter-correlations varied between 0.60 (physical and social) and 0.76 (physical and mental).
Claustrophobia Questionnaire (CLQ)
The 26-item CLQ (Radomsky et al. Reference Radomsky, Rachman, Thordarson, McIsaac and Teachman2001) is a revised and shortened version of the original CLQ (Rachman & Taylor, Reference Rachman and Taylor1993) comprising 36 items. The CLQ rates the degree of anxiety aroused by different potentially claustrophobic situations (5-point answer scales: 0, not at all to 4, extremely). Since our sample consisted of PD patients, not claustrophobia patients, we analysed the CLQ answers with nonlinear CFA in order to test previously established two-factorial structure reflecting suffocation fear (14 items) and restriction fear (12 items) (Radomsky et al. Reference Radomsky, Rachman, Thordarson, McIsaac and Teachman2001). The structural analyses did not corroborate this two-factor structure. Instead, results suggested that besides suffocation fear (items 1, 4, 5–7, 13) and physical restrictions fear (items 15–25) a third dimension (agoraphobic situations fear; items 2, 3, 8–12, 14, 26) has to be taken into account in order to sufficiently explain CLQ answer covariance in this patient sample. Factor loadings ranged from 0.45 to 0.87. Factor inter-correlations ranged between 0.59 (restriction and suffocation) and 0.81 (restriction and agoraphobic situations). The model fit of this three-factor model was acceptable (RMSEA = 0.08, CFI = 0.96, TLI = 0.96).
Statistical analyses
All instruments used here provided ordinal answer categories. As a consequence, the answers were presumably not multi-normally distributed and especially not linearly related to underlying continuous dimensions (latent variables; LV). Therefore all analyses relied on nonlinear CFA based on the two-item parameter (2P) Item Response Theory (IRT) model. This model class has been specifically developed for the appropriate handling of binary and ordinal dependent variables and applies logistic instead of linear regression to compute the associations between LVs and their indicators. It prevents biased results when the assumptions of multi-normality and linearity made by conventional linear methods are not met. The 2P-IRT-model analyses tetrachoric or polychoric correlations estimated from the matrix of the observed answer covariance. Its factor-analytical re-parameterization requires that besides the item discriminations also the item difficulties are computed (for further explications of this model class, see e.g. Glöckner-Rist & Hoijtink, Reference Glöckner-Rist and Hoijtink2003). Muthén (Reference Muthén2002) has integrated this model class within a generalized structural equation modelling (SEM) framework in Mplus (http://www.statmodel.com). All nonlinear continuous CFA and SEM models were computed with this program (version 6.0).
The following CFA models, which formalize different assumptions about the factorial structure of the 10 DSM-IV bodily PAS, were investigated and compared:
-
(1) A model positing two bodily PAS factors, i.e. a cardio-respiratory and a vestibular/mixed somatic factor following Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006).
-
(2) A model excluding the cardiac symptoms from the respiratory dimension by specifying three PAS factors (i.e. a respiratory, a vestibular/mixed somatic, and in addition a separate cardiological factor).
All model computations were performed with a robust mean and variance adjusted, weighted least squares (WLSMV) estimator. The CFI, TLI, and RMSEA are reported as descriptive indices of statistical fit. Values >0.90 and >0.95 for the first two indices and values <0.10 and close to 0.05 for the RMSEA are interpreted as indicating an acceptable and good fit (cf. Bollen, Reference Bollen1989). Studies following the original recommendations of Bollen (1989) show that for linear models a cut-off criterion of 0.08 might be too lenient. Yet for nonlinear models with several answer categories for indicators – here even five – this criterion is appropriate (Yu, Reference Yu2002). In contrast to linear models, nonlinear models require the estimation of significantly more parameters, thereby necessarily increasing RMSEA values. However, the substantive interpretability of the models was also considered an important criterion to judge the adequacy of the results. Bivariate residual correlations were also considered in order to uncover possible additional systematic influences on answer processes.
The association of the PAS dimensions with the four specific ACQ fear cognitions was tested by regressing each of them on the final measurement model for the bodily PAS criteria. The resulting regression coefficients may indicate specific associations of fear cognitions to bodily PAS criteria dimensions.
Results
Prevalence of bodily panic attack symptoms
A heart rate increase (item 3) was the most common symptom. Nearly all of the patients (98.3%) endorsed such an increase within a typical panic attack. The next most frequent symptom endorsed was dizziness (96%), followed by shortness of breath (92%), sweating (88%), chest pain (85%), chills (84%), trembling (84%), nausea (83%), and choking (79%). Paresthesia was the least frequent symptom (69.5%). Palpations were most often rated ‘extremely’ (highest answer category, 47%), whereas only 14% used this answer category to rate paresthesias.
Confirmatory factor analysis of the bodily attack symptom criteria
The allocation of the body symptoms and the factor loadings for the respective model are presented in Table 2. We first tested a two-dimensional model representing Meuret et al.'s (2006) respiratory-cardiac and mixed-somatic factors (M1). However, the fit of this model was not acceptable (CFI = 0.83, TLI = 0.78, RMSEA = 0.15). Moving symptom 8 (‘numbness’) from the cardio-respiratory factor to the vestibular/mixed somatic factor in accordance with the modification indices improved the fit of M2 compared to M1, but the fit was still not acceptable (CFI = 0.90, TLI = 0.87, RMSEA = 0.12).
Table 2. Item allocation and factor loadings for the tested dimensional models

M1, Model representing Meuret's dimensions; M2, item 8 (numbness) of model M1 relocated to the V/M factor; M3, Model with separated cardiac and respiratory factor; M4 = M3 with one residual correlation; R, respiratory factor; V/M, vestibular/mixed somatic factor; C, cardiac factor.
The modification indices both for model 1 and model 2 suggested a strong residual correlation between symptom 1 (shortness of breath) and symptom 2 (choking). Both criteria asked specifically and uniquely about respiratory symptoms. We tested a three-dimensional model (M3) retaining the vestibular/mixed somatic factor, but including separate respiratory and cardiac factors. This model explained the answer covariance clearly better than the two-dimensional models. CFI (0.96), TLI (0.95) and RMSEA (0.07) were acceptable. The factor loadings were all sufficiently large, with only one loading slightly smaller than 0.40 (symptom 7, ‘nausea’). No residual correlation >0.20 was left, but the modification indices suggested to include the residual correlation between symptoms 5 (‘sweating’) and 9 (‘chills or hot flushes’) into the model specification. This appeared reasonable, as the two criteria presumably are functionally related.
The three-factor model with the additional residual correlation between symptoms 5 (‘sweating’) and 9 (‘chills or hot flushes’) (M4) reached a still better model fit (CFI = 0.98, TLI = 0.97, RMSEA = 0.05), although with smaller factor loadings of symptoms 5 (‘sweating’) and 9 (‘chills or hot flushes’) on the vestibular/mixed somatic factor than before (cf. Table 2). Whereas the correlation between the respiratory and the cardiac factor remained the same, the correlation between the vestibular/mixed somatic and the cardiac factor (r = 0.62) and the vestibular/mixed somatic and the respiratory factor (r = 0.34) changed slightly. This three-factor CFA model with one residual correlation included achieved both the best fit and also appeared substantively reasonable.
Relationship of the three panic attack criteria dimensions to the specific ACQ fear cognitions
The three attack criteria dimensions established in the measurement model (M4) were used to predict each of the four ACQ items in turn. The resulting standardized regression coefficients are listed in Table 3. As expected, the fear of a heart attack (item 4) was predicted well by the cardiac dimension, and the fear of choking to death (item 5) by the respiratory dimension. Both the fear of a loss of control (item 8) and the fear of going crazy (item 11) were predicted by the vestibular/mixed somatic factor. The prediction of item 4 (heart attack) by the cardiac factor and item 8 (loss of control) by the vestibular/mixed somatic factor was accompanied by significant negative regression coefficients for both remaining factors, which added to the specificity of the associations of these two items to the bodily symptoms dimensions.
Table 3. Standardized regression coefficients for the regression of four ACQ specific fear items on the three dimensions of the measurement model for the DSM-IV bodily symptom attack criteria

ACQ, Agoraphobic Cognitions Questionnaire.
** p < 0.01, *** p < 0.001.
Relationship between the bodily symptom factors and ASI and CLQ
Next, we examined the relationship between the bodily PAS dimensions and the ASI and CLQ dimensions. The model fit was good, with RMSEA = 0.05, TLI = 0.95, and CFI = 0.95. The correlations between the PAS dimensions and the ASI and CLQ are shown in Table 4. The three CLQ factors were significantly related only to the respiratory factor. The respiratory dimension was only modestly associated with the ASI physical dimension and not associated with the other ASI dimensions. By contrast, the vestibular/mixed somatic factor was linked to all ASI dimensions, including the ASI social dimension. The cardiac dimension correlated with the mental and physical dimensions of the ASI, with the later having the strongest association.
Table 4. Correlation between the factors of the SEM

SEM, Structural equation modelling, CLQ, Claustrophobia Questionnaire, ASI, Anxiety Sensitivity Index.
* p < 0.01.
The bodily PAS factors were not significantly correlated with age and gender. Moreover, correlations between single bodily PAS criteria and gender (r ⩽ 0.16) and age (r ⩽ −0.14) were rather low. Including gender and age in the SEM relating the bodily PAS dimensions to the CLQ and the ASI did not change the pattern of associations. Furthermore, site of treatment centres was not significantly correlated with any of the PAS dimensions (r ⩽ 0.18) and was not a significant covariate in the PAS model.
Discussion
Comparing different models using CFA, we found that the DSM-IV bodily PAS are best represented by a three-factor solution consisting of respiratory, vestibular/mixed somatic, and cardiac dimensions. The vestibular/mixed somatic dimension includes all the PAS criteria allocated to the autonomic/somatic dimension of Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006). By contrast, our separate cardiac and respiratory factors differ. A respiratory dimension has been reported consistently by several studies. However, previous studies are inconsistent with respect to the allocation of the PAS chest pain and palpitations. Although chest pain also appeared to be associated with the respiratory factor in our models, the best fit was obtained when subsuming this symptom together with palpitations under a separate cardiac factor. Such a distinct cardiac factor is consistent with Pio-Abreu et al. (Reference Pio-Abreu, Ramalheira and Valente1998).
The three dimensions of our model related differentially to the specific anxiety constructs we introduced (i.e. fear cognitions, claustrophobic fear and anxiety sensitivity). This supports the notion that they did not artificially result from over-extraction or reflect reporting biases of the PD patients. The fear of having a heart attack and choking to death were predicted well by the cardiac and the respiratory dimensions, respectively. In addition, the fear of having a heart attack was also negatively related to the respiratory and the vestibular/mixed somatic dimension, but less strongly. This underscores the specificity of the association of the heart attack cognition to the cardiac dimension. The cognitions of losing control and going crazy were both predicted by the vestibular/mixed somatic factor and were not related to any of the other factors. Incidentally, this pattern of associations advises against including the cognitive PAS criteria together with the bodily PAS into dimensional analyses. That is, the PAS criterion of fear of dying apparently harbours two distinct fears, each tied closely to particular bodily PAS. Arguably, fear of dying would load on the respiratory and the cardiac dimension and thus hinder their separation in dimensional analyses.
Differential associations of the three bodily PAS dimensions were also found for anxiety sensitivity. To date, no consensus exists regarding the association between panic symptoms and anxiety sensitivity. Panic symptoms have both been linked to ‘mental concerns’ (Naragon-Gainey, Reference Naragon-Gainey2010) and characterized as ‘almost entirely attributable to the fear of physical sensations dimension of anxiety sensitivity’ (Olatunji & Wolitzky-Taylor, 2009, p. 993). Our data seem to support both positions in that all three bodily PAS dimensions were correlated with the physical concerns facet of anxiety sensitivity, but were also differentially associated with the remaining two facets of anxiety sensitivity. The cardiac and the vestibular/mixed somatic factor but not the respiratory factor were associated with mental concerns, and only the vestibular/mixed somatic factor was correlated with the social concerns facet of anxiety sensitivity. It might be interesting for future studies to examine the reasons why especially vestibular symptoms are related to concerns with mental incapacity.
Given the correlational nature of our data, we cannot conclude whether the ASI or the suffocation scale is better suited to predict panic attacks. However, our results will contribute to this discussion. The CLQ factors including fear of suffocation were only correlated with the respiratory dimension, whereas the ASI physical concerns correlated highest with the cardiac dimension, and the ASI mental and the social concerns were both associated with the vestibular/mixed somatic dimension. Thus, it seems reasonable to expect that the potential of these questionnaires to predict panic attacks depend on the particular symptoms prominent in an individuals’ typical panic attack. For example, the CLQ should be a better predictor of panic attacks for individuals with respiratory symptoms than for individuals with predominant cardiac or vestibular PAS.
Our findings regarding the structure of the ASI are consistent with previous dimensional analysis of the ASI even though the ASI structure has previously not been examined in a homogenous sample of PD patients with agoraphobia. The CLQ was not explicitly designed for the assessment of PD and its structure had not previously been analysed based on ratings by PD patients. Our failure to replicate the often-reported two-dimensional structure may consequently be due to our sample. That is, our third ‘agoraphobic fear’ factor might be due to the answer covariance produced specifically by PD patients with agoraphobia.
Limitations
Our results are limited in several ways. Patients in our study were asked to rate symptoms for a recent typical panic attack. The results might have differed if we had collected ratings of the most severe panic attacks. Thus our findings are limited to typical panic attacks. Further, it could be argued that all of the symptoms – both physical and cognitive – reflect the nature of panic (i.e. they are two factors that relate to a higher order factor). Because we made the a priori decision to follow the cognitive model of panic, we only asked about physical symptoms during a typical panic attack. Thus we were not able to directly test factor analytic models of PAS dimensions including both cognitive and physical symptoms.
Our model for the bodily PAS achieved a good fit and performed well in terms of low residual correlations. Nonetheless, the factor structure was not entirely satisfactory. Two of the factors only consisted of two items and at least three or four items have been recommended to substantiate the estimation of a dimension (Schmidt & Joiner, 2002). A serious limitation is inherent in the practice of subjecting PAS criteria consisting of several symptoms to dimensional analyses. When symptoms that tend to co-occur in a panic attack are already combined in the PAS criteria, then they cannot contribute to the covariance between PAS. This reduces the chances of adequately determining PAS dimensions. Thus, future attempts to uncover the structure of PAS should disaggregate the combined symptoms into single symptoms and also include more items to represent hitherto neglected symptom domains (Ottaviani & Beck, Reference Ottaviani and Beck1987). For example, Pio-Abreu et al. (Reference Pio-Abreu, Ramalheira and Valente1998) have both disaggregated the DSM-IV PAS and included abdominal PAS in addition to the bodily DSM-IV PAS and reported a separate abdominal factor in addition to a respiratory and a cardio factor.
Although the prevalence of PAS reported is comparable to previous studies with respect to their rank order, our patients generally were among the more severely affected patient samples described in the literature. Only Cox et al. (Reference Cox, Swinson, Endler and Norton1994) reported similarly high symptom endorsement rates. This may be due to agoraphobia being an inclusion criterion in our study. Shioiri et al. (Reference Shioiri, Someya, Murashita and Takahashi1996) and Segui et al. (Reference Seguí, Salvador-Carulla, Garcia, Canet, Ortiz and Farré1998) both found a relationship between vestibular symptoms and agoraphobia. Thus, the inclusion of only agoraphobic patients might have increased symptom reports. Meuret et al. (Reference Meuret, White, Ritz, Walton, Hofmann and Brown2006) reported that most of their PD patients also had agoraphobia – in contrast to less than half of the PD patients in the study of Shioiri et al. (Reference Shioiri, Someya, Murashita and Takahashi1996).
Further, and consistent with most studies of this nature, our data consisted of retrospective reports of the symptoms. These might differ from the symptoms experienced by patients during a panic attack. For example, symptoms linked to an individual's fear (e.g. palpitations when fearing a heart attack) may be remembered as being extremely strong, while such sensations as chills seem less threatening during the panic attack and may therefore not explicitly be remembered. De Beurs et al. (Reference De Beurs, Garssen, Buikhuisen, Lange, Balkom and Dyck1994) collected data from continuous self-monitoring of panic attacks and compared these data to recalled symptoms. By computing the concordance rates between response modalities, the authors concluded that ‘many patients do not have a consistent profile of panic symptoms’ (p. 43). Thus further research on panic subtypes should include the use of self-monitoring data.
Final remarks
In summary, we found that the DSM-IV bodily panic attack symptoms experienced during a typical panic attack of PD patients are best described by three dimensions: respiratory, cardiac and vestibular/mixed somatic. These three dimensions are differentially related to specific fear cognitions, anxiety sensitivity, and suffocation fear. Consideration of panic dimensions and subtypes is therefore important for future research trying to link PD to the ASI or other variables of the cognitive model of panic attacks. For example, Ehlers & Breuer (Reference Ehlers and Breuer1996) remarked that an increased perception of an individual's heart rate could not be found in general among PD patients, but rather for the subgroup with cardiac neurosis. The present results, in particular with regard to the differential association of ASI and CLQ further support the notion that the symptom profiles and the specific associated fears of patients require specific therapeutic interventions (e.g. specific symptom provocation exercises), which should be further examined (cf. Gerlach & Neudeck, Reference Gerlach, Neudeck, Neudeck and Wittchen2012).
Further research using other methods and samples will be necessary to explore panic dimensions and subtypes. A better description of symptom profiles and associated constructs could improve the poor detection rates of PD in the healthcare system (cf. Sansone & Sansone, Reference Sansone and Sansone2009; Fernández et al. Reference Fernández, Rubio-Valera, Bellón, Pinto-Meza, Luciano, Mendive, Haro, Palao and Serrano-Blanco2012), and support the development of more efficacious PD treatment.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S0033291714002803.
Acknowledgements
This work is part of the German multicentre trial ‘Mechanisms of Action in CBT (MAC)’. The MAC study is funded by the German Federal Ministry of Education and Research (BMBF; project no. 01GV0610) as part of the BMBF Psychotherapy Research Funding Initiative. Centres: Principal investigators (PI) with respective areas of responsibility in the MAC study are V. Arolt (Münster: Overall MAC Programme Coordination), H. U. Wittchen (Dresden: Principal Investigator (PI) for the Randomized Clinical Trial and Manual Development), A. Hamm (Greifswald: PI for Psychophysiology), A. L. Gerlach (Münster: PI for Psychophysiology and Panic subtypes), A. Ströhle (Berlin: PI for Experimental Pharmacology), T. Kircher (Marburg: PI for Functional Neuroimaging), and J. Deckert (Würzburg: PI for Genetics). Additional site directors in the RTC component of the programme are G. W. Alpers (Würzburg), T. Fydrich and L. Fehm (Berlin-Adlershof), and T. Lang (Bremen). Data Access and Responsibility: All principlal investigators take responsibility for the integrity of the respective study data and their components. All authors and co-authors had full access to all study data. Data analysis and manuscript preparation were completed by the authors and co-authors of this article, who take responsibility for its accuracy and content. Acknowledgements and staff members by site: Greifswald (coordinating site for psychophysiology): Christiane Melzig, Jan Richter, Susan Richter, Matthias von Rad; Berlin-Charité (coordinating centre for experimental pharmacology): Harald Bruhn, Anja Siegmund, Meline Stoy, Andre Wittmann; Berlin-Adlershof: Irene Schulz; Münster (Overall MAC Program Coordination, Genetics and Functional Neuroimaging): Andreas Behnken, Katharina Domschke, Adrianna Ewert, Carsten Konrad, Bettina Pfleiderer, Peter Zwanzger; Münster (coordinating site for psychophysiology and subtyping): Judith Eidecker, Swantje Koller, Fred Rist, Anna Vossbeck-Elsebusch; Marburg/Aachen (coordinating centre for functional neuroimaging): Barbara Drüke, Sonja Eskens, Thomas Forkmann, Siegfried Gauggel, Susan Gruber, Andreas Jansen, Thilo Kellermann, Isabelle Reinhardt, Nina Vercamer-Fabri; Dresden (coordinating site for data collection, analysis, and the RCT): Franziska Einsle, Christine Fröhlich, Andrew T. Gloster, Christina Hauke, Simone Heinze, Michael Höfler, Ulrike Lueken, Peter Neudeck, Stephanie Preiß, Dorte Westphal; Würzburg Psychiatry Department (coordinating centre for genetics): Andreas Reif; Würzburg Psychology Department: Julia Dürner, Hedwig Eisenbarth, Antje B. M. Gerdes, Harald Krebs, Paul Pauli, Silvia Schad, Nina Steinhäuser; Bremen: Veronika Bamann, Sylvia Helbig-Lang, Anne Kordt, Pia Ley, Franz Petermann, Eva-Maria Schröder. Additional support was provided by the coordinating centre for clinical studies in Dresden (KKS Dresden): Xina Grählert and Marko Käppler. The RTC project was approved by the Ethics Committee of the Medical Faculty of the Technical University of Dresden (EK 164082006). The neuroimaging components were approved by the Ethics Committee of the Medical Faculty of the Rheinisch-Westfälische Hochschule University Aachen (EK 073/07). The experimental pharmacology study was approved by the Ethics Committee of the state of Berlin (EudraCT: 2006-00-4860-29). [The study was registered with the ISRCTN: ISRCTN80046034.]






