Introduction
It is now accepted that psychosis is influenced by social factors. Trauma is hypothesized to play a causal role in the occurrence and phenomenology of psychosis for a subgroup of people (Bebbington, Reference Bebbington2015; Okkels, Trabjerg, Arendt, & Pedersen, Reference Okkels, Trabjerg, Arendt and Pedersen2017; Varese et al., Reference Varese, Smeets, Drukker, Lieverse, Lataster, Viechtbauer and Bentall2012b). This opens up new possibilities for preventing and managing the devastating impact that psychosis can have on people's lives (Schizophrenia Commission, 2012). Given that resilience is the most common trajectory following trauma, we need to develop our understanding of the role of trauma-related mechanisms in distressing psychosis (Galatzer-Levy et al., Reference Galatzer-Levy, Huang and Bonanno2018; Hardy, Reference Hardy2017; Holmes et al. Reference Holmes, Ghaderi, Harmer, Ramchandani, Cuijpers, Morrison and Craske2018). These mechanisms can then be targeted in interventions, in line with a causal interventionist approach (Goekoop & Goekoop, Reference Goekoop and Goekoop2014; Kendler & Campbell, Reference Kendler and Campbell2009).
Progress will be hampered if research is constrained by diagnostic constructs (Brewin & Patel, Reference Brewin and Patel2010). This is because there is marked phenomenological, symptomatic and diagnostic overlap in psychosis and traumagenic mental health problems, such as depression and post-traumatic stress disorder (PTSD) (Geddes, Ehlers, & Freeman, Reference Geddes, Ehlers and Freeman2016; McCarthy-Jones & Longden, Reference McCarthy-Jones and Longden2015; Okkels et al., Reference Okkels, Trabjerg, Arendt and Pedersen2017). Further, PTSD and Schizophrenia-spectrum diagnoses have been criticised as they are highly heterogeneous categories. This heterogeneity suggests that different causal mechanisms may be involved for any given individual and that subtypes of trauma-related psychosis may exist (Bentall et al., Reference Bentall, de Sousa, Varese, Wickham, Haarmans and Read2014; Galatzer-Levy & Bryant, Reference Galatzer-Levy and Bryant2018).
Network theory can address this complexity, as it assumes that mental health difficulties arise not from a common latent variable, but from dynamic feedback loops between components (‘nodes’) which are investigated using network analysis (Borsboom, Reference Borsboom2017; Fried et al., Reference Fried, van Borkulo, Cramer, Boschloo, Schoevers and Borsboom2016) The feedback loops are the result of causal interactions between nodes (‘edges’) that are maintained in a network. The effect of any given node within a network varies by the strength, with certain nodes playing a relatively more central role. As network nodes often cut across diagnostic boundaries, network analysis provides a means of developing a transdiagnostic understanding of how post-traumatic stress and psychosis symptoms interact. Further, certain interactions may cluster, potentially allowing for the identification of hypothesized subtypes of trauma-related psychosis. To date, no studies have investigated post-traumatic stress and psychosis symptoms using network analysis. We therefore describe a proof-of-concept exploratory study examining the interactions between these symptoms, and any clusters within them, to inform future research.
Network analyses relevant to this study have tended to focus on either trauma and psychosis, or PTSD. For example, Fried et al. (Reference Fried, Eidhof, Palic, Costantini, Huisman-van Dijk, Bockting and Karstoft2018) compared four moderate to large samples with PTSD (with civilian, refugee, combat and professional-related traumas) and found that intrusive memories, hyperarousal and emotional detachment were among the most central symptoms. Similarly, intrusive memories, together with negative emotions and beliefs, were most central at baseline and 3-year follow-up in 311 military veterans with PTSD (Von Stockert, Fried, Armour, & Pietrzak, Reference Von Stockert, Fried, Armour and Pietrzak2018). It is of note that these central symptoms include both the characteristic symptoms of PTSD (e.g. intrusive memories and hyperarousal) and depression (e.g. negative emotions and beliefs, and emotional and behavioural detachment), in line with a transdiagnostic approach. Isvoranu, Borsboom, van Os, and Guloksuz (Reference Isvoranu, Borsboom, van Os and Guloksuz2016) investigated the network associations between childhood trauma types and psychotic dimensions (i.e. positive, negative and general psychopathology) in 552 people with psychosis. In support of an affective pathway to psychosis, they identified that all relationships were connected through emotional and behavioural difficulties, with anxiety having a dominant role in the network. These findings indicate the potential utility of examining the interactions between psychosis and post-traumatic stress symptoms.
A drawback of network theory is that it has tended to focus on symptoms as network components (Borsboom, Reference Borsboom2017). Building on recent proposals, we argue that to enhance the usefulness of network methods to psychological theory and therapy, empirically based mechanisms (which may be reflected by symptoms or other psychosocial phenomena) should be included as nodes (Fried & Cramer, Reference Fried and Cramer2017; Jones et al., Reference Jones, Heeren and McNally2017). Hardy (Reference Hardy2017) highlights current evidence suggesting the key trauma-related psychological mechanisms involved in psychosis are intrusive trauma memories, beliefs, and cognitive, behavioural and interpersonal emotion regulation. Whilst these putative trauma-related processes have been investigated in the literature, multiple mechanisms are rarely examined and as a result, little is known about their relative associations with psychotic symptoms. Network analysis may help to elucidate which trauma-related variables are most related to psychotic symptoms. In this study, we focus on the associations between intrusive trauma memories (i.e. re-experiencing), emotional regulation (i.e. hyperarousal, avoidance and emotional numbing), beliefs (i.e. post-traumatic cognitions) and positive psychotic symptoms (i.e. auditory hallucinations and delusional beliefs). Our first two research questions aimed to highlight the most central symptoms in a sample of people with psychosis diagnoses, with the final question exploring whether symptom associations appeared to reflect distinct subtypes of trauma-related psychosis. The following questions were examined:
(1) Which symptoms are most influential in a network of post-traumatic stress and psychosis symptoms?
(2) Which symptoms account for identified associations in a network of post-traumatic stress and psychosis symptoms?
(3) Are there identifiable sub-clusters of associations in post-traumatic stress and psychotic symptoms?
Method
Baseline data from two randomized controlled trials of trauma-focused therapy for people with post-traumatic stress symptoms and psychosis diagnoses were combined for the retrospective analysis [cognitive behaviour therapy for PTSD in Schizophrenia (C-PAS) trial, Steel et al., Reference Steel, Hardy, Smith, Wykes, Rose, Enright and Mueser2017a, and treating trauma in psychosis (T.TIP) trial, van den Berg et al., Reference van den Berg, de Bont, van der Vleugel, de Roos, de Jongh, van Minnen and van der Gaag2015]. The C-PAS trial was given ethical approval by Berkshire Research Ethics Committee (SC/09/ H0505/85) and was registered as ISTCRN 67096137 and the T.TIP trial was approved by the medical ethics committee of the VU University Medical Centre and was registered as ISRCTN 79584912.
Participants
The combined sample (N = 216) represents a broad spectrum of individuals with psychosis diagnoses and post-traumatic stress symptoms. Both trials recruited adult participants (age 18–65), with a current or lifetime diagnosis of psychotic disorder from community psychosis teams, with sufficient language to participate and with no diagnosed organic impairment. Symptom variability is a requisite of network analysis which was supported by differences in the PTSD and psychosis diagnostic criteria for the two trials. For PTSD symptoms, the C-PAS trial participants reflected a broader range of PTSD symptom severity because 45% (n = 27) did not meet diagnostic criteria for PTSD. Psychotic symptom variability was ensured as the C-PAS trial criterion was current Schizophrenia-spectrum disorder whereas the T.TIP trial criterion was a lifetime diagnosis of a psychotic disorder. Sample characteristics are displayed in Table 1, further information on the sample and recruitment methods is published in the original papers.
Table 1. Sample demographics and symptom descriptives (N = 216)

These are %s and in italics to distinguish them from SDs in the other brackets.
Measures and variables
Measures were selected based on which assessments were included in both trials. Variables were then extracted from three measures. Data were taken from baseline assessments.
The clinician-administered PTSD scale (CAPS)
The CAPS is a semi-structured interview based on the DSM-IV (APA, 1994) criteria for PTSD. There are 17 symptoms items including five for re-experiencing, five for hyperarousal and seven for avoidance and emotional numbing. Each item is scored on two 5-point scales (0–4) for frequency and intensity that are then summed to produce a total item score ranging from 0 to 8, or a total severity score ranging from 0 to 136. The 17 individual item scores were used in this study. As described above, these symptoms were conceptualised as reflecting trauma-related psychological mechanisms (i.e. re-experiencing was a proxy for episodic trauma memory intrusions, and hyperarousal and avoidance and numbing symptoms as types of emotional regulation). The CAPS is a valid and reliable measure with high specificity and sensitivity and is a widely used interview for diagnosing PTSD in psychosis (Blake et al., Reference Blake, Weathers, Nagy, Kaloupek, Gusman, Charney and Keane1995; Mueser et al., Reference Mueser, Salyers, Rosenberg, Ford, Fox and Carty2001).
Post-traumatic cognitions inventory (PTCI)
The PTCI is a 36-item self-report questionnaire that assesses post-traumatic cognitions. These were viewed as reflecting the psychological mechanism of trauma-related beliefs. Scores range from 1 to 7 and are summed into three factors, which were used in the analysis: negative cognitions about self (21 items), negative cognitions about the world (seven items), and self-blame (five items). The PTCI has been found to have strong psychometric properties (Foa, Ehlers, Clark, Tolin, & Orsillo, Reference Foa, Ehlers, Clark, Tolin and Orsillo1999).
The psychotic symptom rating scales (PSYRATS)
The PSYRATS is a semi-structured interview that assesses the phenomenology of auditory hallucinations and delusional beliefs. For the purposes of this study, the frequency/intensity factor items were used as they best captured the psychological constructs of interest (Woodward et al., Reference Woodward, Jung, Hwang, Yin, Taylor, Menon and Erickson2014). For auditory hallucinations, these were the summed scores of frequency, duration, and disruption items and for delusional beliefs, they included the sum of the preoccupation, conviction, and disruption items. The PSYRATS scales have excellent inter-rater reliability and have been found to have strong validity (Haddock, McCarron, Tarrier, & Faragher, Reference Haddock, McCarron, Tarrier and Faragher1999).
Network analysis
The statistical software R (version 3.5) was used to conduct statistical analyses. Packages used included qgraph (Epskamp, Cramer, Waldorp, Schmittmann, & Borsboom, Reference Epskamp, Cramer, Waldorp, Schmittmann and Borsboom2012), bootnet (Epskamp, Borsboom, & Fried, Reference Epskamp, Borsboom and Fried2018), mgm (Haslbeck & Waldorp, Reference Haslbeck and Waldorp2018) and networktools (Jones, Reference Jones2017). The network modelling approach taken followed an Extended Bayesian Information Criterion (EBIC) least absolute shrinkage and selection operator (LASSO) procedure, implemented within a single Gaussian random fields network. This method controls model complexity through the model selection process and subjecting estimated regression parameters to a penalty (small associations are reduced to zero). Thus producing a model with good prediction accuracy and sparse representation of the predictors in the model (Zou, Hastie, & Tibshirani, Reference Zou, Hastie and Tibshirani2017). Missing cases were handled with pairwise deletion. The variables were ordinal but were not normally distributed as such a nonparanormal transformation was applied to network items to relax assumptions of normality in our dataset. Within the graphical representation, ‘edges’ are the lines between nodes representing regularized partial correlations; the estimated relationship between two variables while controlling for all other variables. These associations represent predictive associations (similar to multiple regression). The presence of an edge indicates a dependent relationship between variables, the absence indicates that they are conditionally independent (given all other nodes in the network). Blue edges illustrate positive associations and red edges negative associations. The wider and more saturated the edge, the stronger the association. The accuracy of edges and stability estimates for the network were calculated using a bootstrapping procedure (1000 iterations) (Epskamp & Fried, Reference Epskamp and Fried2018).
Our first research question was examined through the calculation of centrality metrices of expected influence (Haslbeck & Waldorp, Reference Haslbeck and Waldorp2018) and predictability (Jones, Reference Jones2017) for each item. Expected influence reflects the total level of involvement of a node in the network. One-step expected influence is defined as the sum of all edge strengths extending from a given node (local centrality), whereas two-step expected influences assesses centrality up to two edges away from the node (global centrality). A node could be highly central but share nearly no variance with other nodes. As such we have also calculated predictability which quantifies how much influence we can have on a node by intervening on all its neighbours: item variance predicted by connected items (R 2). If a node displays high centrality and predictability, this supports the interpretation of the importance of this node within the network.
To address our second research question, we computed the shortest path (Dijkstra, Reference Dijkstra1959) from flashbacks (the hallmark symptom of PTSD, Brewin, Reference Brewin2015; Brewin, Gregory, Lipton, & Burgess, Reference Brewin, Gregory, Lipton and Burgess2010) to positive psychotic symptoms (auditory hallucinations and delusions) within the network. This analysis identified the nodes (symptoms) which mediate the predictive quality between them. We also included a bridge expected influence strength metric (Jones, Reference Jones2017) to quantify symptoms which connect post-traumatic stress symptoms to positive psychotic symptoms. Identifying the bridging items between post-traumatic stress and positive psychotic symptoms used the 80th percentile cut off on the scores of bridge expected influence metric.
For the third research question, a model-based, dimension reducing clustering approach (Scrucca, Reference Scrucca2010) was taken to reveal subpopulations, given the expected heterogeneity in psychosis samples (e.g. Millan, Fone, Steckler, and Horan, Reference Millan, Fone, Steckler and Horan2014). R package Mclust version 5 (Scrucca, Fop, Murphy, & Raftery, Reference Scrucca, Fop, Murphy and Raftery2016) was used for analysis. A description of the modelling procedure is included in online supplementary materials.
Results
Descriptive statistics
The descriptive statistics for the sample are shown in Table 1. The majority of participants had a schizophrenia diagnosis and scored above the threshold for severe post-traumatic stress disorder (CAPS >65; Mueser et al., Reference Mueser, Salyers, Rosenberg, Ford, Fox and Carty2001) (further information on the T.TIP and C-PAS samples is provided in online supplementary materials Table S1 and Steel et al. Reference Steel, Hardy, Smith, Wykes, Rose, Enright and Mueser2017a, Reference Steel, Doukani and Hardy2017b; van den Berg et al. Reference van den Berg, de Bont, van der Vleugel, de Roos, de Jongh, van Minnen and van der Gaag2015).
Research question one: which post-traumatic stress and psychosis symptoms have the strongest associations with each other?
The network (see Fig. 1) yielded 82 positives (and 1 negative) relationships out of 231 possible edges. Edge and strength centrality stability was adequate (0.44 and 0.36, respectively) (see online supplementary materials Figs S1–S3 for stability analysis). Assessing expected influence revealed that negative cognitions about the self and negative cognitions about the world had the largest direct influence on the network (locally and globally) (see online supplementary materials Fig. S4). Predictability estimates (the proportion of item variance explained by pairwise interactions within the network) are displayed in Fig. 1 (see online supplementary materials Table S2). Predictability of nodes was low overall (mean of 22%). Negative cognitions about self (52%) and the world (43%) could be best explained by associated nodes (including each other). Auditory hallucinations (18%), trauma memory intrusions (21%) and flashbacks (19%) displayed relatively moderate predictability, and may be independent of other factors or determined by factors not included in the network.
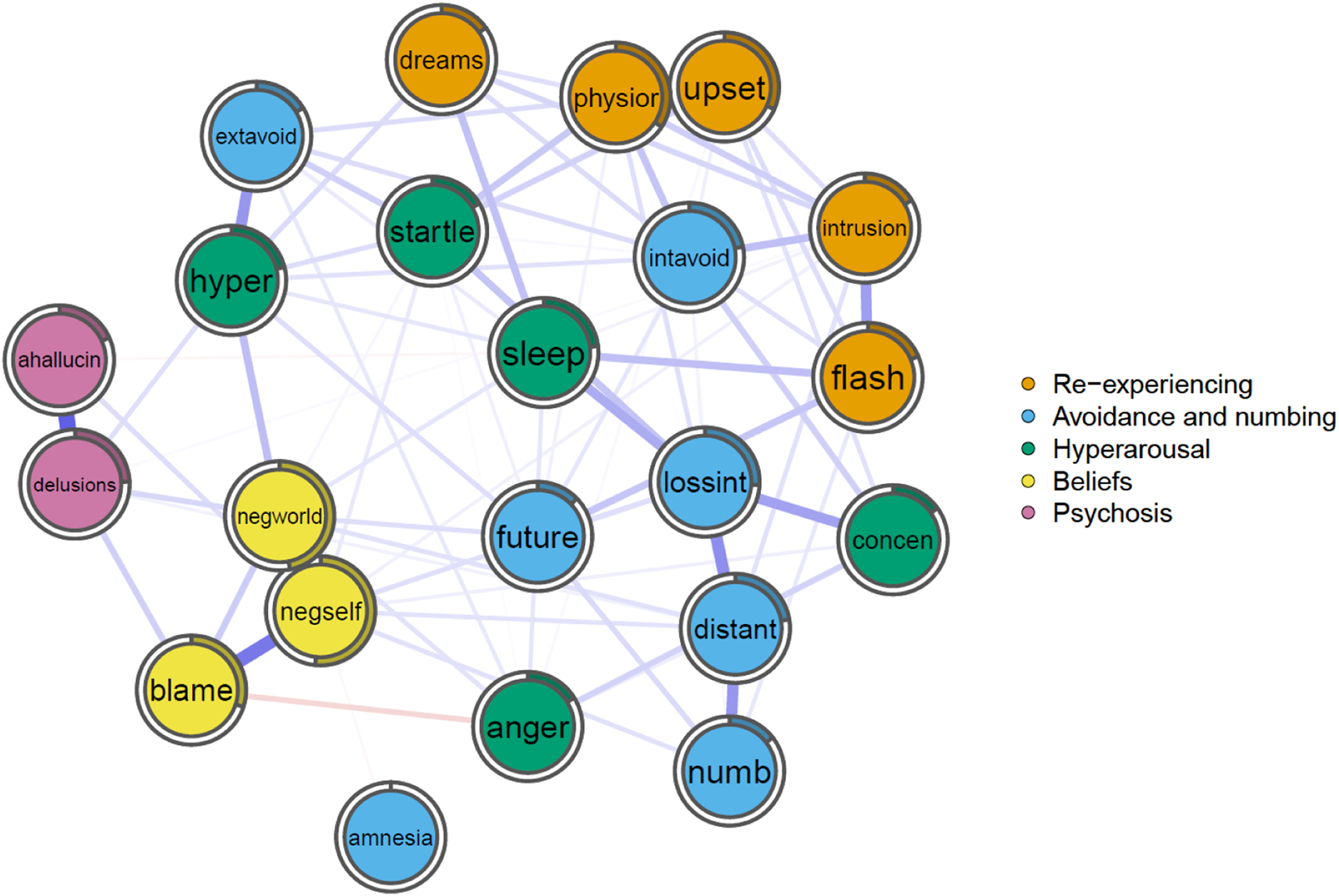
Fig. 1. The network graph shows associations and predictability estimates between post-traumatic stress symptoms (i.e. re-experiencing, avoidance and numbing, hyperarousal), post-traumatic cognitions, and positive symptoms of psychosis (i.e. auditory hallucinations and delusional beliefs). The edges represent the strength of association between nodes (used to calculate expected influence), with the shaded area of the pie chart around the nodes indicating the predictability measure (i.e. dark segment representing higher predictability).
* Dreams = recurrent distressing dreams, physior = physiological reactivity to trauma cues, upset = psychological distress to trauma cues, intrusions = intrusive distressing trauma recollections, flash = acting or feeling as if the traumatic event were recurring, extavoid = avoiding trauma-related activities, places or people, intavoid = avoiding trauma-related thoughts, feelings and conversations, lossint = diminished interest or participation in activities, future = sense of foreshortened future, distant = feeling of detachment or estrangement from others, numb = restricted range of affect, amnesia = inability to recall important parts of trauma, hyper = hypervigilance, startle = exaggerated startle response, sleep = difficulty falling or staying asleep, concen = difficulty concentrating, anger = irritability or outbursts of anger, negworld = negative beliefs about world, negself = negative beliefs about self, blame = self-blame, ahallucin = frequency/intensity of auditory hallucinations, delusions = frequency/intensity of delusions.
Research question 2: which symptoms account for associations between post-traumatic stress and psychosis?
Negative cognitions about the self, negative cognitions about the world, self-blame and hypervigilance bridged post-traumatic stress and psychosis symptoms in this sample (see online supplementary materials Fig. S5). The shortest path analysis (see Fig. 2) displays the route from flashbacks to delusions and auditory hallucinations. Flashbacks and delusions are conditionally independent and indirectly connected through the sense of a foreshortened future and negative cognitions about the world. The shortest pathway between flashbacks and auditory hallucinations was indirectly connected by the same nodes, although also passed through delusions. Thus, the estimated models and metrics suggest that auditory hallucinations, delusions and flashbacks are conditionally independent and mediated by these associated variables.
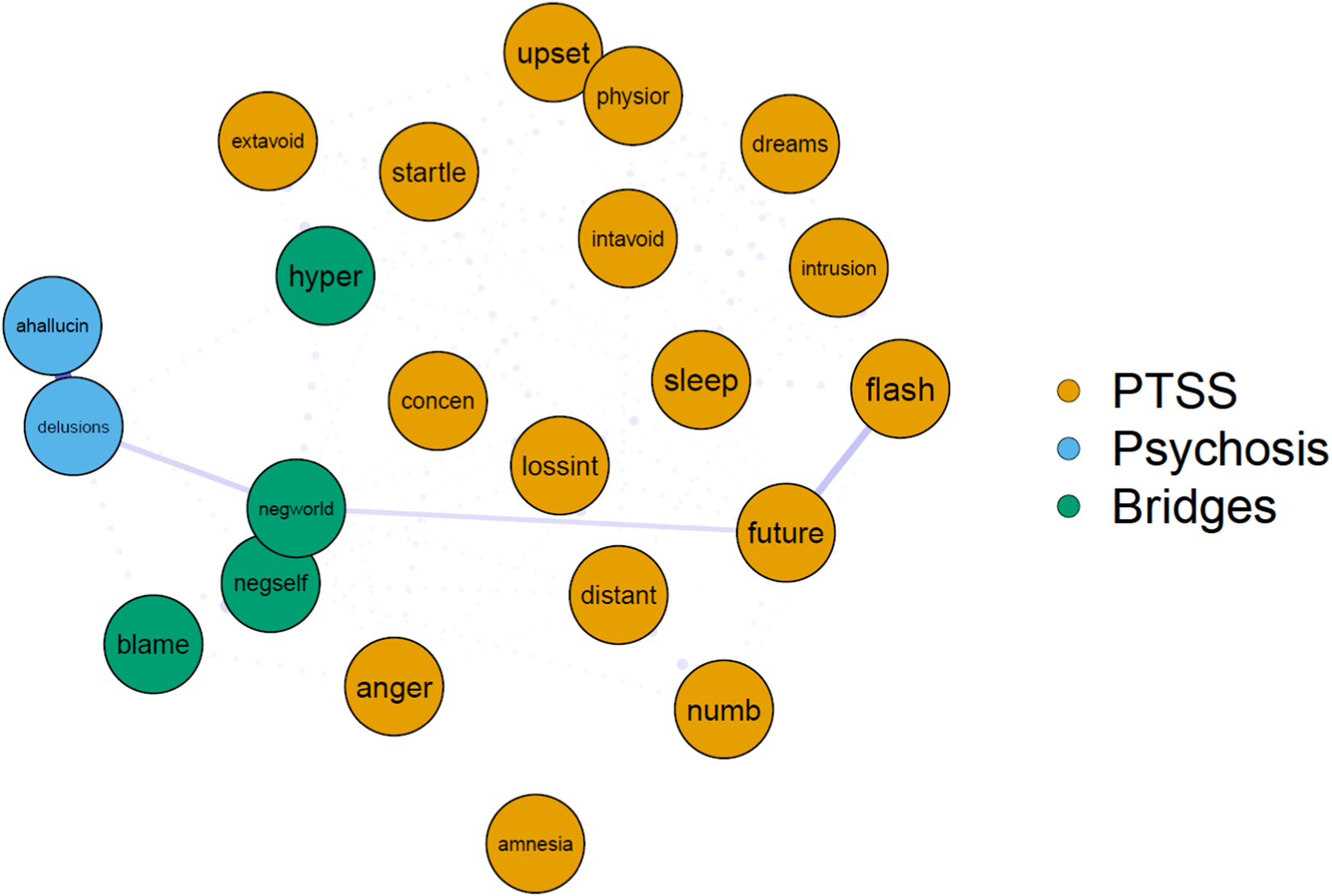
Fig. 2. Bridging symptoms between post-traumatic stress and positive psychotic symptoms are highlighted in green, and shortest paths between flashbacks, auditory hallucinations and delusions are shown.
* Dreams = recurrent distressing dreams, physior = physiological reactivity to trauma cues, upset = psychological distress to trauma cues, intrusions = intrusive distressing trauma recollections, flash = acting or feeling as if the traumatic event were recurring, extavoid = avoiding trauma-related activities, places or people, intavoid = avoiding trauma-related thoughts, feelings and conversations, lossint = diminished interest or participation in activities, future = sense of foreshortened future, distant = feeling of detachment or estrangement from others, numb = restricted range of affect, amnesia = inability to recall important parts of trauma, hyper = hypervigilance, startle = exaggerated startle response, sleep = difficulty falling or staying asleep, concen = difficulty concentrating, anger = irritability or outbursts of anger, negworld = negative beliefs about world, negself = negative beliefs about self, blame = self-blame, ahallucin = frequency/intensity of auditory hallucinations, delusions = frequency/intensity of delusions.
Research question 3: Are there subgroups of associations between post-traumatic stress and psychosis symptoms?
To address the question of whether the data indicated subtypes of trauma-related psychosis, we examined whether there were sub-clusters of associations between post-traumatic stress and psychotic symptoms. We performed a dimensional reduction in order to explore possible clusters. A one-dimensional equal variance model supported a 2-class solution, which yielded a best-fitting model with a BIC value of – 823.75 (see online supplementary materials Fig. S6). This model explained a large proportion of the variation across variables (eigenvalue = 0.757). This suggests the observed scores in the entire sample are not from a distinct severity population, but are instead related to two distributions, reflecting two subpopulations (n = 70, n = 146). One group (n = 70) was characterised by significantly more severe PTSD symptoms, auditory hallucinations and trauma-related beliefs, although there were no differences between the groups for self-blame, amnesia and delusional beliefs. The sample size of each group precluded a reliable interpretation of networks, however, the severe population form a distinct separate class in which the correlational structure is fundamentally different from the less severe population.
Discussion
This study is the first to use network analysis, which generates partial correlations, to examine the interplay between post-traumatic stress and psychotic symptoms. Trauma-related beliefs were the most influential symptoms, and together with hypervigilance, accounted for the shortest paths between flashbacks, delusions and hallucinations (with the latter only connected to re-experiencing through delusional beliefs). These results are in contrast to findings which suggest a central role for re-experiencing and dissociative detachment in hallucinations to explain the association between trauma and psychosis (Berry, Varese, & Bucci, Reference Berry, Varese and Bucci2017; Luhrmann et al., Reference Luhrmann, Alderson-Day, Bell, Bless, Corlett, Hugdahl and Waters2019; McCarthy-Jones & Longden, Reference McCarthy-Jones and Longden2015). Instead, this study suggests beliefs reflecting a lack of safety, control and self-esteem account for the interactions between PTSD and psychosis. This is consistent with the emphasis on inter- and intrapersonal threat in theoretical models and research evidence (Freeman & Garety, Reference Freeman and Garety2014). Threat beliefs are likely to interact with emotions, sensory-perceptual experiences, cognitive biases, appraisals, behaviour and interpersonal relating, thereby contributing to psychosis and PTSD (Brewin et al., Reference Brewin, Gregory, Lipton and Burgess2010; Hardy, Reference Hardy2017).
Symptoms that can be conceptualised as linked to emotional regulation (e.g. loss of interest, interpersonal distance and hypervigilance) were the next most influential nodes in the main network. Further, hypervigilance was a bridge symptom between post-traumatic stress and psychotic symptoms. These findings are in line with previous network analyses of PTSD and suggest that understandable attempts to regulate threat may paradoxically perpetuate symptoms of post-traumatic stress and psychosis (Fried et al., Reference Fried, Eidhof, Palic, Costantini, Huisman-van Dijk, Bockting and Karstoft2018; Von Stockert et al., Reference Von Stockert, Fried, Armour and Pietrzak2018). They are also consistent with the proposed role of selective attention for threat in paranoia, which is often not distinguishable from trauma-related hypervigilance (Freeman et al., Reference Freeman, Thompson, Vorontsova, Dunn, Carter, Garety and Ehlers2013). Interestingly, trauma-related dissociative detachment as measured by emotional numbing (which can be conceptualised as an emotion regulation strategy, Brown, Reference Brown2006) did not appear to have a strong impact on psychosis, despite proposals implicating its role in voice hearing (Berry et al., Reference Berry, Varese and Bucci2017; Dalenberg et al., Reference Dalenberg, Brand, Gleaves, Dorahy, Loewenstein, Cardena and Spiegel2012; Luhrmann et al., Reference Luhrmann, Alderson-Day, Bell, Bless, Corlett, Hugdahl and Waters2019; McCarthy-Jones & Longden, Reference McCarthy-Jones and Longden2015; Pearce et al., Reference Pearce, Simpson, Berry, Bucci, Moskowitz and Varese2017; Varese et al., Reference Varese, Barkus and Bentall2012a). This suggests that activation of the sympathetic nervous system (associated with flight and fight responses) may be more potent in maintaining psychotic experiences than parasympathetic activation (related to flag and freeze responses).
We found that intrusive trauma memories also had a less central relationship than has been previously reported in studies of PTSD and voice hearing (Alsawy, Wood, Taylor, & Morrison, Reference Alsawy, Wood, Taylor and Morrison2015; Fried et al., Reference Fried, Eidhof, Palic, Costantini, Huisman-van Dijk, Bockting and Karstoft2018). This finding is also consistent with the T.TIP trial which reported that effectively reducing re-experiencing did not significantly affect hallucination severity, although it did have a significant impact on paranoia and other symptoms of PTSD. The re-experiencing symptoms of emotional distress and physiological reactivity did have a relatively more central role in the network. However, this may be attributable to the activation of beliefs in autobiographical memory leading to trauma-congruent emotions and bodily responses, not to involuntary recollections of specific episodic memories. It may also be that the intrusion of event memories in psychosis occurs differently to re-experiencing in PTSD. Severely decontextualised trauma memories (i.e. whereby arousal has inhibited the encoding of the spatial and temporal context of events) could manifest as intrusions which are experienced as occurring in the ‘here and now’ without any sense of a past experience being recollected, and so would not be experienced as memories (Hardy, Reference Hardy2017; Steel, Fowler, & Holmes, Reference Steel, Fowler and Holmes2005).
Two networks of interactions distinct from those in the main network were also identified, suggesting our sample may reflect two distinct subtypes of trauma-related psychosis. One was more severe and characterised by beliefs, re-experiencing, voices and delusions, whereas beliefs were most influential in the other, and occurred with delusions, interpersonal detachment, emotional reactivity and physiological reactivity. The possibility of a subtype of post-traumatic stress in psychosis typified by entrenched trauma-beliefs that generalise to delusions and detachment, with another subtype also being maintained by intrusive memories and hallucinations, requires further investigation. It may be that the latter subgroup reflects the occurrence of complex PTSD with psychosis symptoms (Frost, Louison Vang, Karatzias, Hyland, & Shevlin, Reference Frost, Louison Vang, Karatzias, Hyland and Shevlin2019).
Whilst sample size limits the reliability of this analysis and it requires replication, it provides a preliminary indication that distinct subgroups of symptom interactions may exist, which may plausibly require distinct therapeutic approaches (van den Berg & Hardy, Reference van den Berg, Hardy, Badcock and Paulik2020). In relation to therapeutic targets, overall our analysis suggests modifying trauma-related beliefs may have a beneficial impact on both PTSD and psychosis, in line with evidence that they are a key mechanism of change in trauma-focused therapy (Cooper, Clifton, & Feeny, Reference Cooper, Clifton and Feeny2017). However, the C-PAS trial targeted trauma-related beliefs using cognitive restructuring to reduce PTSD in psychosis and obtained a null result on all outcomes (Steel et al., Reference Steel, Hardy, Smith, Wykes, Rose, Enright and Mueser2017a). This illustrates that directly targeting the mechanism with the strongest impact on the network may not be an effective way to destabilise it (Bringmann et al., Reference Bringmann, Elmer, Epskamp, Krause, Schock, Wichers and Snippe2019). Given the high predictability of trauma-related beliefs, it could be more effective to intervene on the mechanisms which interact with them. In support of this, the T.TIP trial focused on modifying re-experiencing and avoidance using Prolonged Exposure and EMDR and found these interventions were effective in reducing trauma-related beliefs, paranoia and other PTSD symptoms (van den Berg et al., Reference van den Berg, de Bont, van der Vleugel, de Roos, de Jongh, van Minnen and van der Gaag2015). As re-experiencing and avoidance are mechanistically linked to trauma-related beliefs and psychosis, it makes sense that targeting the former has a beneficial effect on the latter (Hardy, Reference Hardy2017). For example, flashbacks of a sexual assault and avoidance of memories may be maintained by beliefs that ‘others will harm me’ and ‘I cannot cope’, which also contribute to paranoia. By reducing avoidance and reprocessing the memories of sexual assault through exposure techniques, the person may learn that ‘not everyone will harm me’ and ‘I can manage’. These alternative trauma-related beliefs may then have a negative interaction with paranoia and reduce psychosis severity (van den Berg & Hardy, Reference van den Berg, Hardy, Badcock and Paulik2020).
Whilst the study shows that the network approach holds promise for developing our understanding of post-traumatic stress and psychosis, there are important limitations. First, the sample was biased as it only included people with significant PTSD symptoms which may have limited its variance and meant it did not reflect the range of trauma-related presentations in psychosis (e.g. people with a solely negative symptom profile would not have been included). The base rate of symptoms may, therefore, account for the findings, and replication is needed in a more representative sample reflecting the full spectrum of post-traumatic stress reactions. The limited strength of associations between some nodes (including auditory hallucinations and re-experiencing) possibly indicates that not all the relevant mechanisms were included. Other potential psychological mechanisms include emotions, metacognitive beliefs and a broader range of emotional regulation strategies, which could be investigated alongside micro (e.g. neurochemical) and macro (e.g. social) processes (Isvoranu, Boyette, Guloksuz, & Borsboom, Reference Isvoranu, Boyette, Guloksuz, Borsboom, Tammina, Ivleva, Reininghaus and van Osin press). This study did not include some commonly used measures of trauma-related processes, and the assessment of dissociative detachment being restricted to emotional numbing and not including depersonalisation and derealisation is a significant limitation. The low predictability may also be the result of the heterogeneous nature of symptoms. If distinct subtypes of trauma-related psychosis exist, they are likely to be associated with different causal processes and associations with post-traumatic stress symptoms (McCarthy-Jones et al., Reference McCarthy-Jones, Thomas, Strauss, Dodgson, Jones, Woods and Sommer2014). We emphasise the hypotheses we have outlined from the findings require further investigation, as causal inferences are not possible given the study's cross-sectional design, the modest network stability, and the undetermined flow of mechanisms in the network (Bringmann et al., Reference Bringmann, Elmer, Epskamp, Krause, Schock, Wichers and Snippe2019; Fried et al., Reference Fried, van Borkulo, Cramer, Boschloo, Schoevers and Borsboom2016). Time series investigation of the role of trauma-related mechanisms in psychosis is required to improve our understanding of the dynamic interactions between post-traumatic and psychotic symptoms. Indeed, it has been argued that focusing on the overall dynamics of a network may be more useful in identifying intervention targets than trying to analyse the most central network nodes, given that modifying these may not be effective in destabilising the network (Bringmann et al., Reference Bringmann, Elmer, Epskamp, Krause, Schock, Wichers and Snippe2019). A limitation of the analysis is that EBIC tuning parameter (set to zero), can lead to the estimation of false-positive associations emphasising sensitivity (at the cost of specificity). While the absence of an edge may reflect the absence of a true association it may also reflect insufficient power to identify a small association. Confirmation of the results in a large sample using a more conservative LASSO tuning parameter is warranted.
In summary, this is the first study to examine the interplay of post-traumatic stress and psychotic symptoms using network analysis. To investigate the potential role of trauma-related psychological processes in psychosis, re-experiencing symptoms were conceptualised as reflecting the involuntary retrieval of episodic trauma memories, hyperaroused, avoidant and numbing symptoms as types of emotional regulation, and post-traumatic cognitions as schematic beliefs. In line with trauma-focused theories of psychosis and evidence from therapy trials, the findings support the role of cognitive, emotional, behavioural and interpersonal processes in psychosis (Brand et al., Reference Brand, McEnery, Rossel, Bendall and Thomas2018; Hardy, Reference Hardy2017; van den Berg et al., Reference van den Berg, de Bont, van der Vleugel, de Roos, de Jongh, van Minnen and van der Gaag2015). Whilst the approach is in its infancy, network models may provide a compelling opportunity to tailor micro, meso and macro level interventions to target the specific processes underlying the development and maintenance of problems (Borsboom, Reference Borsboom2017; Fried & Cramer, Reference Fried and Cramer2017; Looijestijn, Blom, Aleman,, Hoek, & Goekoop, Reference Looijestijn, Blom, Aleman, Hoek and Goekoop2015). The network identified in this study suggests that building a sense of safety, control and self-worth could reduce the widespread influence of trauma-related beliefs on symptoms. Longitudinal investigations incorporating comprehensive assessment of putative mechanisms are now needed to advance our understanding of post-traumatic stress in psychosis, and support the development of effective interventions.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291720001300
Acknowledgements
We would like to thank all the participants, clinicians and researchers involved in the T.TIP and C-PAS trials for supporting this work. AH, CS and DvB receive payment for training and supervision on post-traumatic stress in psychosis. MvG and CO'D declare no conflicts of interest in relation to this work. This work was supported by the National Institute for Health Research (NIHR) for the C-PAS Trial, under its Research for Patient Benefit (RfPB) Programme (Grant Reference Number PB-PG-1207-15077). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. The T.TIP trial was supported by the Dutch support foundation Stichting tot Steun Vereniging voor Christelijke Verzorging van Geestes en Zenuwzieken (Dr van der Gaag). CO'D is supported by the UCLH NIHR BRC.






