Introduction
Silicone lymphadenopathy is defined as the presence of silicone in a lymph node, and is an uncommon complication of using silicone prostheses for either joints or plastic surgical procedures, specifically breast augmentation or reconstruction.Reference Truong, Cartwright, Goodman and Woznicki1, Reference Christie, Weinberger and Dietnich2 Such cases pose a diagnostic challenge as malignancy is often the initial consideration. In this report, we discuss a rare case of silicone lymphadenopathy occurring in the supraclavicular lymph nodes of a patient with a prior history of cosmetic augmentation mammoplasty with silicone implants. In such cases, fine needle aspiration cytology (FNAC) is a useful initial investigation and may be sufficient for diagnosis. If inconclusive, excisional biopsy of the affected lymph node for histological analysis should also be performed.Reference Tabatowski, Elson and Johnston3
Case report
A 52-year-old woman presented to the ENT out-patient clinic with a two-month history of a non-tender lump in the left supraclavicular region, having been referred by her general practitioner. There was no history of dysphagia, dysphonia or otalgia, and on questioning she reported no weight loss, poor appetite, feverishness or night sweats. She had a 10 pack-year smoking history. She reported having undergone bilateral breast augmentation for cosmetic purposes 13 years earlier, and was currently being treated for hyperthyroidism, but there was no other past medical history of note.
Clinical examination confirmed a well circumscribed, firm, non-tender, 2 cm lump in the left supraclavicular fossa. No lymphadenopathy was noted elsewhere, and examination of the ears, nose and throat was otherwise unremarkable.
An initial ultrasound scan of the neck revealed several areas of abnormal, increased echogenicity in the left supraclavicular fossa (Figure 1). A 0.5 cm, ill-defined nodule in the thyroid isthmus was also noted, which was initially thought to be the primary site of pathology. Fine needle aspiration of the thyroid lesion unfortunately yielded an insufficient specimen for diagnosis; hence, further investigations were performed. The differential diagnoses considered at this stage included primary head and neck malignancy, metastasis, lymphoma and reactive lymphadenopathy secondary to infection such as tuberculosis.

Fig. 1 Ultrasound scan of the neck showing abnormally increased echogenicity in the left supraclavicular fossa. In retrospect, this is the classically described ‘snowstorm’ appearance of silicone in lymph nodes.
A subsequent magnetic resonance imaging scan of the neck demonstrated a cluster of abnormal left level IV lymph nodes (Figure 2).

Fig. 2 Coronal magnetic resonance imaging scan of the neck demonstrating a cluster of abnormal left level IV lymph nodes.
The patient was recalled for fine needle aspiration of one of these lymph nodes. Cytological examination showed a background of lymphocytes, numerous clusters of adipocytes, and a significant number of multinucleate giant cells with ingested fatty material. No features of malignancy were seen (Figure 3).

Fig. 3 Photomicrograph of fine needle aspiration cytology specimen from the abnormal left level IV lymph nodes, showing multinucleate giant cells together with macrophages containing clear material. (May Grunwald Giemsa stain; ×400)
Since no definitive cytological diagnosis could be made, the patient was scheduled for direct endoscopy of the upper aerodigestive tract and excisional biopsy of the enlarged left supraclavicular lymph node. On macroscopic inspection, the specimen was solid and grey-white in colour. Endoscopy of the pharynx, larynx and upper oesophagus was unremarkable. Histological analysis identified a lymph node which had largely been replaced by foreign material masses, with a pronounced foreign body response (Figure 4). No evidence of malignancy was seen. It was concluded that the appearances were in keeping with a foreign body response to silicone from a leaking breast implant. Tissue culture yielded no growth and no acid-alcohol-fast bacilli were seen on direct staining, making a diagnosis of tuberculosis unlikely.
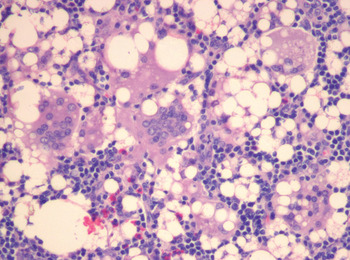
Fig. 4 Photomicrograph of left enlarged supraclavicular lymph node following excisional biopsy, showing that normal lymph node contents have been displaced by multinucleate giant cells and clear globular areas (where the silicone is located). (H&E; ×200)
Subsequent computed tomography (CT) scanning of the neck, thorax, abdomen and pelvis revealed no lung or mediastinal lesions. Apart from small nodes in the porta hepatis, which were deemed to be within normal limits, no other areas of lymphadenopathy were seen. Hence, a diagnosis of lymphoma was very unlikely. The CT images were later reviewed by a breast radiologist who noted irregularity of the capsule of both breast implants, consistent with bilateral rupture (this is termed the ‘linguine sign’) (Figure 5).

Fig. 5 Axial, arterial phase, soft tissue window, computed tomography scan of the thorax, demonstrating irregularity of the capsule of both breast implants (the ‘linguine sign’) consistent with bilateral rupture.
The patient was reassured that malignancy had not been detected. She was referred back to the plastic surgeon who had performed the original breast augmentation, with a view to further assessment of leakage or rupture of the silicone breast prostheses.
Discussion
Silicone lymphadenopathy, involving a foreign body reaction to silicone, is a well documented complication of breast augmentation using silicone-containing materials.Reference Truong, Cartwright, Goodman and Woznicki1, Reference Rivero, Schwartz and Mies4
It has been postulated that silicone can migrate through tissues via two distinct mechanisms: firstly, through rupture or erosion of a silicone-containing surface; or secondly, through continued leakage through an intact surface.Reference Adams, Cox and Rao5, Reference Hausner, Schoen, Mendez-Fernandez, Henly and Geis6 When silicone tissue migration occurs via either of these mechanisms, fibrosis and foreign body granulomatous reactions can occur.Reference Van Diest, Beekman and Hage7 Silicone particles may be transported to regional lymph nodes via macrophages in the reticulo-endothelial system.Reference Tabatowski, Elson and Johnston3 The resulting foreign body reaction may produce local swelling of the involved lymph node, such as the left supraclavicular lymph nodes in the case reported.
Silicone lymphadenopathy following breast augmentation primarily affects the axillary nodes,Reference Adams, Cox and Rao5, Reference Kulber, MacKenzie, Steiner, Glassman, Hopp and Hiatt8 but there have been reported cases involving intramammary,Reference Rivero, Schwartz and Mies4 internal mammaryReference Kao, Rand, Holt, Pierce, Timmons and Wood9 and supraclavicular lymph nodes.Reference Shipchandler, Lorenz, McMahon and Tubbs10 The current case is particularly unusual in that, to our knowledge, it is the first reported case of silicone lymphadenopathy manifesting solely in a supraclavicular lymph node in a patient with no prior history of breast cancer. Shipchandler et al. described a similar case of supraclavicular lymphadenopathy due to silicone breast implants in 2007; however, this patient later developed bilateral axillary silicone lymphadenopathy.
Silicone lymphadenopathy poses important clinical considerations in the approach to the patient with a lump in the neck or axilla and a prior history of silicone augmentation mammoplasty. Although the clinician's initial priority should be to exclude malignancy, it is important to note whether there is any prior history of breast augmentation using silicone-containing materials. If not considered in the initial differential diagnosis, silicone foreign body reaction is a difficult diagnosis to arrive at. Furthermore, in patients who have had breast cancer treated with mastectomy followed by reconstructive mammoplasty using silicone gel implants, the possibility of metastatic breast cancer should obviously be high in the differential diagnosis; however, silicone lymphadenopathy should not be disregarded. For the majority of individuals who have had silicone augmentation mammoplasty purely for cosmetic purposes, silicone lymphadenopathy should be considered, in addition to a possible new diagnosis of malignancy.
Once a silicone foreign body reaction is suspected, FNAC of the affected lymph node has been shown to be a cost-effective and accurate initial investigation to aid diagnosis.Reference Tabatowski, Elson and Johnston3,Reference Santos-Briz, Lopez-Rios, Santos-Briz and De Agustin11 In such cases, FNAC shows a foreign body reactive, lymphoid background with numerous giant cells, as in the case described. If there is clinical suspicion of silicone lymphadenopathy, FNAC alone may be sufficient for a definitive diagnosis. However, if FNAC is inconclusive, or if other, more sinister diagnoses are suspected, a conservative excisional lymph node biopsy is advisable to provide a histological diagnosis and to exclude concomitant malignancy.Reference Tabatowski, Elson and Johnston3
• Silicone lymphadenopathy is a rare complication of procedures involving silicone
• Axillary lymph nodes are the most commonly affected after silicone mammoplasty
• Supraclavicular lymph nodes are very rarely involved
• Malignancy is the most important differential diagnosis
• Diagnosis is by fine needle aspiration cytology, plus excisional biopsy histology if needed
• Plastic or breast surgeons should assess implant leakage or rupture before considering removal
Here, we describe a rare case of supraclavicular lymphadenopathy secondary to silicone foreign body reaction. In patients with a prior history of silicone augmentation mammoplasty, silicone lymphadenopathy should be considered in the differential diagnosis of supraclavicular neck lumps. However, the initial priority in such cases should be to exclude malignancy. Fine needle aspiration cytology may be sufficient for diagnosis, but in the absence of conclusive findings excisional biopsy should also be performed to provide a histological diagnosis.
Conclusion
Silicone lymphadenopathy is a rare but recognised complication of procedures involving the use of silicone. In the case of silicone augmentation mammoplasty, the axillary lymph nodes are the most commonly affected site; very rarely, the supraclavicular lymph nodes may be involved. In such cases, malignancy is the most important differential diagnosis, but silicone lymphadenopathy should also be considered. Although fine needle aspiration cytology alone may be sufficient for definitive diagnosis, in doubtful cases lymph node excisional biopsy should also be performed for histological analysis. Affected patients should be referred to a plastic or breast surgeon for assessment of implant leakage or rupture before removal is considered.







