Introduction
At the Newcastle Cognitive and Behavioural Therapies Centre (NCBTC), a tertiary specialist CBT service, it has been recognized that there are a group of patients receiving individual therapy who, alongside chronic, complex and refractory Axis I disorders and axis II traits and disorders, present with significant and pervasive difficulties with emotion regulation, particularly the regulation of negative emotions. This observation prompted the development of a Mindfulness-based Cognitive Behavioural Therapy (MBCT) intervention which focuses upon cognitive and behavioural factors which maintain problems with emotion regulation and which augments treatment as usual at the Centre (Liddell et al. Reference Liddell, Meares, Standart, Wood and Freeston2012). Our observation as result of this intervention is that engagement and progress in treatment is enhanced, symptoms associated with poor engagement and outcome such as dissociation and maladaptive coping strategies are reduced (Standart & Wood, Reference Standart and Wood2011).
The context of this service development arose from an inpatient ward staff team on a ward which was closed down shortly after this project began. In 2012 the NCBTC received an increase in referrals for tertiary-level intervention for patients with significant difficulties with emotion regulation who were struggling to stabilize sufficiently to make progress in treatment within their inpatient setting from Urgent Care services and in particular from this ward. What these patients had in common was that they were presenting with significant and often chronic emotion regulation difficulties, and that these difficulties were thought to be significant in an inability to stabilize and make progress in treatment offered in the setting they were in.
The therapeutic use of mindfulness has added a new way of promoting engagement and enhancing progress in CBT (Baer, Reference Baer2003; Hayes & Feldman, Reference Hayes and Feldman2004; Germer et al. Reference Germer, Siegal and Fulton2005; Singh et al. Reference Singh, Lancioni, Winton, Adkins, Wahler, Sabaawi and Singh2007). Mindfulness is the awareness and non-judgmental acceptance of moment-to-moment experience. It involves the development of a capacity to engage a calm, non-reactive mind, without either holding onto or pushing away experience. There is some evidence that acceptance and mindfulness-based interventions can be usefully adopted in clinical inpatient settings and for challenging problems, for example, borderline personality disorder, complex PTSD and dissociation, psychosis and to enhance treatment team progress (Linehan et al. Reference Linehan, Schmidt, Dimeff, Craft, Kanter and Comtois1999; Bohus et al. Reference Bohus, Haaf, Simms, Limberger, Schmaal, Unckel, Lieb and Linehan2004; Chadwick et al. Reference Chadwick, Newman-Taylor and Abba2005, Reference Chadwick, Hughes, Russell, Russell and Dagnan2009; Singh et al. Reference Singh, Singh, Sabaawi and Wahler2006; Cloitre et al. Reference Cloitre, Courtois, Charuvastra, Carapezza, Stolbach and Green2011; Kearney et al. Reference Kearney, McDermott, Malte, Martinez and Simpson2012).
There is also evidence that developing mindfulness in staff groups and carers not only improves general wellbeing and satisfaction of the staff group but enhances the therapeutic milieu and therefore outcomes associated with engagement and recovery (Singh et al. Reference Singh, Singh, Sabaawi and Wahler2006; Noone & Hastings, Reference Noone and Hastings2010; Voss, Reference Voss2011). While mindfulness is increasingly well known and various training exists, it is important to tailor any initiative to the specific context and characteristics of the recipients (Didonna, Reference Didonna2009). This is equally true whether staff or patients are the intended recipients of any training or intervention.
Planned course of intervention
Given the context of:
-
• recent developments at NCBTC in adapting MBCT for emotion regulation in complex and ‘stuck’ cases,
-
• the increased demand for this intervention across Urgent Care services, and
-
• the enthusiasm for learning and staff development which generated from this team,
it was intended that training these staff in mindfulness would enhance their ability to model and support patients in the acceptance and increased tolerance to negative emotions and promote helpful emotion regulation strategies. Further, training staff in mindfulness would enhance their resilience and ability to cope with the demands of working in this type of setting.
Discussions with the multi-disciplinary team on the ward indicated a desire to develop mindfulness-based interventions; however, rather than training a small number of staff to an advanced level in MBCT, it was considered to be a more effective use of time and resources to provide a high-quality foundation course in mindfulness for a wider staff group. This did not preclude later training of some staff to an advanced practitioner level.
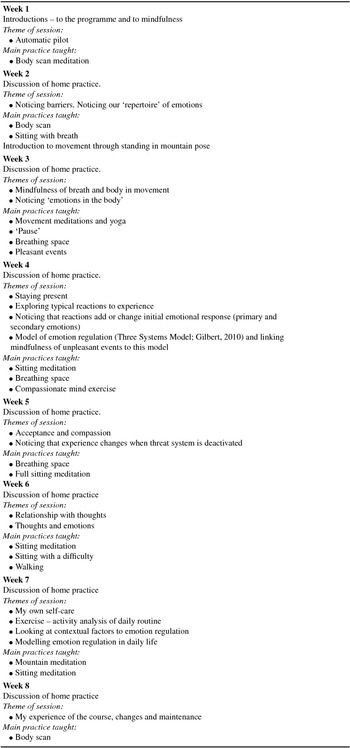
It was proposed that the first author (C.M.), a therapist from NCBTC, who has developed the mindfulness-based emotion regulation programme at NCBTC would lead the training. She had undergone formal training in mindfulness approaches, is an experienced teacher/trainer and supervisor in mindfulness and CBT. The plan was to develop and deliver a tailored foundation course in mindfulness to up to 15 of the ward staff multi-disciplinary team. This foundation course is an 8-week programme of 2 hours per week (see Appendix A).
In light of proposed changes to the configuration and delivery of Urgent Care services, including the closure of the ward in the coming months, it was recognized that there would be changes to the staffing and organization of clinical teams, and that the ward team would be undergoing potentially major changes. Discussions with service managers indicated support for the continuation of this work, recognizing that a training course that has a focus on staff wellbeing and an element of stress reduction could be essential in promoting resilience as clinical teams adapt to change in service delivery and a new working environment.
Method
Participants
Ten staff members attended the induction, all attended the first subsequent session and eight completed the course. The participants who dropped out did so before week 3, and did not volunteer reasons for this. However, other group participants stated that it had been difficult for these two people to arrange adequate cover on their ward. Participants were a mixture of qualified and unqualified nursing staff and occupational therapy staff. They all volunteered to participate and were nominated by their service manager. Managers were asked to select staff who had expressed an interest in learning more about mindfulness, and who would benefit from being able to use a more mindful approach to their own wellbeing and work.
Design
The present study used a double baseline pre-post design with the baseline and pre-training points at least 1 month apart and subsequent evaluations at mid-, post- and 1-month follow-up.
Measures
In a review of research into psychometric assessment of mindfulness, Grossman (Reference Grossman2008) described a number of issues with the psychometric assessment of self-reported ‘mindfulness’, these include but are not limited to: (1) disagreement between practitioners, teachers and researchers within the field of mindfulness to what is meant by mindfulness, which translates into discrepancies as to what is considered relevant and significant to measure, (2) difficulties that arise from assuming participants, no matter how experienced or inexperienced they are in the practice of mindfulness, will have comparable semantic knowledge of the terms used in the rating scales, and (3) potential for the self-reported level of mindfulness to be very different to actual level of mindfulness. We therefore decided to use measures which limited these difficulties as much as possible.
Freiburg Mindfulness Inventory (short form, FMI-14)
Walach and colleagues (Reference Walach, Buchheld, Buttenmüller, Kleinknecht and Schmidt2006) have presented a one-dimensional 14-item short form (FMI-14) of the original FMI which has 30 items and assumes a knowledge of a Buddhist or meditation context. The short form proved to be semantically independent from knowledge of a Buddhist or meditation context and this version also shows acceptable internal consistency (α = 0.86). Both forms (short form and 30-item full versions) have been validated empirically in German- and English-speaking populations (Leigh et al. Reference Leigh, Bowen and Marlatt2005; Heidenreich et al. Reference Heidenreich, Ströhle and Michalak2006). In this study, we used the short form as the participants were not assumed to have an understanding of Buddhist psychology or prior experience of meditation.
Newcastle Mindfulness Training Questionnaire (NMTQ; Moorhead, Reference Moorhead2012)
This face-valid 9-item scale was developed in response to a requirement for a measure that integrated concepts from the practice of mindfulness (Bishop et al. Reference Bishop, Lau, Shapiro, Carlson, Anderson, Carmody, Segal, Abbey, Speca, Velting and Devins2004) with learning and the application of learning to behaviours in the real world (Kirkpatrick & Kirkpatrick, Reference Kirkpatrick and Kirkpatrick2000). Questions are rated on a 1–7 scale in terms of agreement with a given statement (from 1 not at all agree, to 7 completely agree; see Appendix B). It is not designed to be an additive construct; each item tracks an aspect of mindfulness over the five measurement points. The scale first measures progression through three main stages of learning (three items):
-
(a) Understanding mindfulness: to demonstrate a basic awareness and understanding of mindfulness to one's own experiences; participants are asked to rate their confidence in knowing what mindfulness is.
-
(b) Ability to be mindful: participants are asked to rate their ability to bring mindful awareness to emotions, an attentional aspect of mindfulness.
-
(c) Confidence in practice: participants are asked to rate confidence in their own practice of mindfulness outside of sessions as an evaluation that the skills have minimally transferred from the training session.
The next two items measure the core skill of mindful attention to experience and ask participants to rate mindful awareness to internal OR external aspects of experience.
The last four items form a conceptual group related to transfer of the skills to everyday life with both an awareness of and a response to challenging situations in two separate parts of their life, at home and at work:
Awareness: perceived ability to bring mindful awareness to challenging situations at home OR at work (two items).
Skilful response: perceived ability to respond skilfully to challenging situations at home OR at work (two items).
Procedure
Induction workshops and interviews
Induction workshops were provided prior to the course to investigate current understanding, concerns and expectations, and to describe course content and potential demands so that participants could make an informed choice to engage. Following the training, individuals participated in semi-structured interviews to investigate their experiences of training, how it may have influenced their work on the ward, and in relation to specific situations. It was not expected that information from these interviews would be fully representative of staff experiences but that it may inform understanding of the process and future plans. Given that service reconfiguration would be taking place at the same time, it was decided that it would be too difficult to measure impact on patients and on ward activity at this stage as we would effectively have been tracking a moving target.
Consent
Information about the data collection and dissemination was given to each individual in the form of an information leaflet (see Appendix C). Written informed consent was sought from each individual to participate in the data collection. Participation in data collection was voluntary and participants were informed they could withdraw consent at any stage.
Structure and content of the course
The mindfulness course that was delivered was an 8-week MBCT programme tailored specifically to meet the needs of this particular group of participants. The course was structured to allow an initial emphasis on cueing into experience through practices aimed at developing the ability to become aware of moment-to-moment experience; for example, noticing sensations in the body, sounds, sights, smells, and tastes. To develop a ‘calm, non-reactive mind’, there was a particular emphasis upon becoming aware of the body and then, when being aware of the body, learning to observe any emotional, behavioural, and cognitive reactions that happen at the same time.
The course then moved to explore the relationship between thinking styles and processes, behavioural responses, and emotional wellbeing. A cognitive behavioural model was introduced to formulate typical cognitive and behavioural patterns that are known to undermine emotional resilience and wellbeing, and therefore to provide an explicit understandable context to the application of the mindfulness training.
The study was registered as a service improvement project with Northumberland, Tyne and Wear NHS Foundation Trust's Research and Development Department.
Analysis
As far as the data allowed, repeated measures analysis of variance were used on the state and trait mindfulness measures. These measures were the FMI-14 and the NMTQ. There was <10% missing data; the last observation carried forward was implemented. All analyses reported are intention-to-treat. Repeated-measures ANOVA were conducted according to the grouping of variables: single, i.e. time only for the FMI-14, double (stage of learning and attention), and triple (applications in challenging situations) forms, respectively. With a five time-point design, significant time effects were examined through polynomial contrasts (linear through to quartic); no paired comparisons were made between time points. Interactions were investigated through examining the graphs (see Figs 1–3). A significance level of 0.05 was used; effect sizes (η2 p) are reported. Content analysis was used on the information from the staff interviews.

Fig. 1. Changes in awareness of internal and external experience over the course of training.

Fig. 2. Changes in mindful awareness and skilful response over the course of training.

Fig. 3. Mindful awareness vs. skilful response at home vs. work (collapsed across all time points).
Results
The nine NMTQ items were grouped in the following ways. First, understanding mindfulness, ability to be mindful and confidence in practice, were conceptualized as stages of learning. Awareness of internal and external experience were conceptualized as aspects of attention. The remaining four items (mindful awareness and skilful response at both home and work) were conceptualized as applications to challenging experiences. The total FMI score was used. The means and standards deviations are given in Table 1.
Table 1. Means and standard deviations for the Newcastle Mindfulness Training Questionnaire (NMTQ) and Freiberg Mindfulness Inventory at baseline, pre-, mid-, post-training and follow-up

Stages of learning
A 3 × 5, Stage of learning × Time, within-participant ANOVA indicated that Mauchly's test was significant for the main Time effect and for Stage of learning so the assumption of sphericity was not met; Greenhouse–Geisser corrected significance values were used. There was a significant main effect of Time (F 4,28 = 18.45, p = 0.001, η 2 p = 0.73), but no main effect of Stage of learning (F 2,14 = 1.20, p = 0.317, η 2 p = 0.15), and no interaction (F 8,56 = 1.76, p = 0.171, η2 p = 0.20). So, the three stages (understanding mindfulness, ability to be mindful, and confidence in practice) all increased similarly over the training course. Both linear (F 1,7 = 21.93, p = 0.002, η 2 p = 0.76), and cubic (F 1,7 = 22.83, p = 0.002, η 2 p = 0.77), contrasts were significant. Inspection of the means (see Table 1) and the cubic pattern (two points of inflection) indicate an increase between pre-training and mid-training followed by a levelling off. This means that most of the change occurred during the first half of training with a 2-point increase from approximately 3 to 5 during this period, remaining stable through to follow-up.
Attention
A 2 × 5, Awareness (Internal vs. External) × Time, within-participant ANOVA was conducted; sphericity was met. There was a significant Time effect (F 4,28 = 18.16, p = 0.000, η 2 p = 0.72), no Awareness effect (F 1,7 = 0.78, p = 0.407, η 2 p = 0.10), but a significant interaction (F 1,7 = 3.01, p = 0.035, η 2 p = 0.30). As can be seen in Figure 1, both internal and external awareness increased over time, but internal awareness started lower but finished higher than external awareness. Linear (F 1,7 = 25.36, p = 0.002, η 2 p = 0.78), and quartic contrasts (F 1,7 = 15.99, p = 0.005, η 2 p = 0.70), were both significant with the quartic contrast (three points of inflection) suggesting the main increase between pre- and mid-training but also a slight dip from mid- through post-training followed by an upward trend through to 1-month follow-up.
Applications to challenging situations
A within-participant repeated-measures ANOVA was conducted over five time points (Time: baseline, pre-intervention, mid-intervention, post-intervention, follow-up), two levels of Reactions to challenging situations in mindfulness (Reactions: Mindful Awareness vs. Skilful Response) and two contexts (Context: Home vs. Work). Mauchly's test indicated that sphericity was met, so F tests involving Time or interactions with time assumed sphericity. There were significant main effects of Time (F 4,28 = 20.64, p<0.001, η 2 p = 0.75), Reactions (F 1,7 = 15.15, p = 0.006, η 2 p = 0.65), and Context (F 1,7 = 10.97, p = 0.013, η 2 p = 0.61). There were also two significant interactions, namely, Time × Reactions (F 4,28 = 6.35, p = 0.001, η 2 p = 0.48), and Reactions × Context (F 1,7 = 12.44, p = 0.010, η 2 p = 0.64). The other two-way and the three-way interactions were not significant; Time × Context (F 4,28 = 1.40, p = 0.26, η 2 p = 0.17), and Time × Reactions × Context (F 1,28 = 0.18, p = 0.947, η 2 p = 0.03), respectively.
For the time main effect, both the linear contrast (F 1,7 = 31.04, p = 0.001, η 2 p = 0.82, increasing steadily over time) and cubic contrast (F 1,7 = 25.58, p = 0.001, η 2 p = 0.79, rapid change between pre- and mid-intervention) were both highly significant (see the solid line in Fig. 2) and suggest that the greatest change occurred in the early part of the intervention. The Time × Reactions interaction indicates that mindful awareness was initially lower and skilful response was higher (see broken lines in Fig. 2), but they both increased and finished at the same level.
Finally, the Reactions × Context interaction (see Fig. 3) indicate that a similar level of mindful awareness was reported in both contexts, but that there was greater skilful response in the work context. So, overall there was an increase in both mindful awareness and skilful response over time, with awareness lower than response before the intervention and both increased to similar levels by mid-intervention where they essentially remained stable through to follow-up. Irrespective of time point, there was greater mindful responding than awareness at work, whereas at home, similar (and somewhat lower) levels of awareness and responding were reported.
Overall, all three groups of items increased significantly over time, with most increase occurring between pre- and mid-training. While the stages of learning items increased in consort, the two attention items and the four challenging situations items increased differentially within each grouping.
FMI
To benchmark the changes observed on the NMTQ we conducted a repeated-measures ANOVA for the FMI over the five time points: baseline, pre-, mid-, and post-intervention, and follow-up. As for the other measures, there was a significant Time effect (F 4,28 = 9.07, p = 0.004, η 2 p = 0.56). In this case, the linear contrast was the only significant contrast (F 1,7 = 18.00, p = 0.004, η 2 p = 0.72), indicating linear change over the five time points from approximately 31 to 39. However, the non-significant cubic contrast was next in effect size (F 1,7 = 4.96, p = 0.061, η 2 p = 0.43), and together with inspection of the means may suggest once again the increase occurred mainly between pre- and mid-intervention. Effect sizes for the training Time effect (main effect and contrasts) were very large for all groups of items from the NMTQ and also for the FMI.
Discussion
The purpose of this study was to examine whether a MBCT training course would increase levels of mindfulness in clinical staff and to explore potential effects upon staff wellbeing and patient care. The study found that for all participants there was an increase in mindfulness as a result of the training, with the most change happening in the first half of the course. Three areas of change are worth particular comment.
Timing of change in mindfulness skills
The most change in mindfulness skills occurred during the first half of the course. When considering this phenomenon, several possible, not mutually exclusive explanations occurred to the researcher. First, there is evidence that there is a relationship between mindfulness practice and levels of mindfulness (Carmody & Baer, Reference Carmody and Baer2008). Participants did observe that they found regular practice more difficult to maintain as the weeks progressed and so it may follow that the most gains in mindfulness skills were made in the first half of the course when participants were engaged in more home practice.
Second, that there was no imminent or pressing need in participants to apply the mindfulness to their own lives. After the first 4 weeks when participants are introduced to a variety of mindfulness practices, there is a progression to applying what has been learnt to challenges or difficulties. Although a theoretical CBT model of understanding emotion regulation (Gilbert, Reference Gilbert2010) was introduced at the appropriate time in the course, there was no urgency or need to apply this model to a difficulty or problem, such as stress or depression, in this group of staff. This again could account for the tailing off in the rate in which learning increased from the mid-point.
Third, the combination of steep increase from baseline to mid-point and then the tailing off may be influenced by social desirability. At the beginning of the course there may have been a reluctance to report low scores; participants may wish to present themselves in a particular socially desirable way to others and the facilitator. As participants settled, got to know each other and the teacher, they began to rate themselves with more accuracy.
Finally, as stated above, Grossman (Reference Grossman2008) identified that one of the issues with the self-assessment of mindfulness is that there is often a discrepancy between how mindful a person considers themselves to be and how mindful they actually are, and this discrepancy decreases as the person becomes more experienced in the practice of mindfulness. If this was the case in this course, then it would follow that recalibration was occurring after the mid-point as a response to the reduction in the discrepancy.
Changes in attention
In the context of mindfulness practice, paying attention involves noticing moment-to-moment, internal and external experience. There was evidence of differential change between the rate in which awareness of internal vs. awareness of external experiences occurred; awareness of internal experience was rated lower than awareness of external experience at the beginning of the course; however, both of these increased over the course, and at the end of the course awareness of internal experiences was rated higher than external experiences.
Possible explanations for this are that in caring roles, clinical staff may prioritize their focus upon the caring environment; a focus upon internal experience may be considered as a distraction from, or inhibiting, effective care. In a ward setting where high levels of risk and challenging behaviours are managed on a daily basis, a high level of vigilance is necessary to maintain acceptable levels of safety.
In post-course interviews several staff members discussed this area of change. They noticed that prior to the training there was an assumption that noticing their own internal experience, particularly at work, might be associated with over-involvement with their own issues and therefore interfere with their ability to manage demands and provide effective care for patients. As they progressed through the course, the finding was in fact that the opposite was true: while attending to patient care, the ability to include awareness to their own experience was associated with the ability to self-regulate and that this self-regulation had benefits for both patient care and for staff wellbeing. Comments included:
‘I can focus on how I am feeling rather than getting the task done’ therefore ‘I can prioritize more effectively.’
‘I can notice when I am stressed and now know that I need to stop, recognize the urge to charge on, note my bodily sensations and feel calmer.’
Applications to challenging situations
Data from the NMTQ identified that levels of mindful awareness and skilful response to challenging situations both at work and at home increased from pre- to post-course and the increase was maintained at follow-up. Again, the rate of increase was greater from pre- to mid-point. Further analysis of data in the area of applications to challenging situations revealed that staff viewed themselves as relatively confident about their ability to respond skilfully to challenging situations at work prior to beginning the course, but less able to bring mindful awareness to those situations. As the course progressed, staff began to bring mindful awareness to challenging situations at work and noticed further increase in their ability to respond skilfully.
In the mindfulness training the term ‘skilful response’ was used to refer to a response generated from a mindful position. It is interesting to note pre-course co-existing high rating of ability to respond skilfully to challenging situations at work with lower rating of ability to bring mindful awareness to those situations. An explanation could be simply that recalibration occurred during the course as participants became more knowledgeable about was is meant by a skilful response within mindfulness and less concerned with potential consequences of admitting they might be less than skilful at work.
On the other hand, pre-course interviews revealed that staff had elected to attend the course, often in their own time. This was because they were motivated to expand skills and knowledge that would enhance their ability to provide good quality care and interventions to patients; they already had a positive set of beliefs about their ability to perform well at work. These staff worked in a busy and demanding environment where they were often called upon to make quick decisions with little time to reflect. Connelly (Reference Connelly2005) would argue that clinicians who can bring a mindful awareness into interactions such as clinical assessment are more able to focus clearly and support patients to articulate need and to feel validated, and this enhances the clinical interaction. Singh and colleagues (Reference Singh, Singh, Sabaawi and Wahler2006) highlight the improvement to patient experience of care and reduction of aggressive behaviour when care staff are able to bring a mindful awareness to their own experience of the interaction.
Support from interviews
At the end of the course, interviews uncovered that staff felt that their internal, or intrapersonal behaviours, and their ability to relate to themselves and others in a calmer, less reactive way, was very different compared to at the beginning of the course. A shared observation from several participants was that when they engaged in this mindful way of responding to demanding or stressful situations, they noticed that this had a positive and unexpected impact upon patient care. This was summed up beautifully by one participant who said,
when I am with someone who is angry or upset, and I'm feeling stressed, I tell myself to stop and take a breath . . . I don't know who needs to take a breath, me or them, . . . but when I stop and breathe they follow my lead . . . we can then find out together what is going on before deciding what to do about it.
Limitations
The present study was small (N = 8), but the five time-point design, sensitivity of the measures, and the analyses meant that the study was still adequately powered. This study requires replication, both with the current design, but eventually in a randomized controlled trial, if a suitable comparator can be identified. Further study is required to investigate the impact such courses have upon patient care in adult inpatient mental health services such as the ward in question. Likewise, longer follow-up would address the question of retention of benefits. With larger roll-out, other indicators could be examined such as staff absence, illness, and variables related to the ward environment.
The measures used in the present study, especially the NMTQ, proved highly sensitive to perceived changes in knowledge and skill in mindfulness. However, due to its limited use in patient populations, further use of the questionnaire on large samples would enable more formal evaluation of its psychometric properties. However, there remains a question as to whether the pattern of change is a recalibration effect. Asking the participants to re-rate themselves in retrospect would be one way to answer the questions about recalibration, i.e. ‘now that you now know a little more about . . ., would you now rate yourself as you were at the start?’ Alternatively, or in addition, daily self-monitoring of individual participants using single-case design approaches could also address the pattern of change effect.
Conclusion
In conclusion, this service development project successfully supported eight members of staff working within a challenging, demanding clinical area in developing mindfulness skills. There was some evidence that these skills had a positive impact upon decision making and were felt, but not measured, as having a positive impact upon wellbeing and patient care. Most change appeared to occur in the first half of an 8-week programme, and the gains were maintained to the end of the course and through to 1-month follow-up.
Summary of main points
-
• The delivery of training in mindfulness was in response to both clinical demand and expressed interest from a group of staff within an inpatient psychiatric unit.
-
• The delivery was aimed at improving mindfulness skills in the staff group.
-
• The delivery was effective at improving mindfulness skills in this group of staff.
-
• Most gains were made during the first half of the course.
-
• Participants described impact upon their own wellbeing and ability to reflect at work.
-
• Potential impact upon patient care were described by participants.
Acknowledgements
Cate Moorhead is grateful to Kyle Dunn for his hard work, patience and support with the final stages of writing this paper. Thanks are also due to the clinical staff who participated in the course and to ward and management staff who supported them to attend.
Declaration of Interest
None.
Appendix A
Overview of 8-week MBCT programme
Appendix B. Newcastle Mindfulness Training Questionnaire (NMTQ; Moorhead, Reference Moorhead2012)
Newcastle Cognitive and Behavioural Therapies Centre
Mindfulness-Based Cognitive Therapy (8-week foundation course)
This questionnaire is to help us evaluate the effectiveness of this mindfulness group. Initials/name: _________________________

Appendix C. Participant information leaflet
Information Leaflet
Introduction
You have been selected to participate in a training project in Mindfulness. This training course will be evaluated to measure aspects of acceptability and impact. This information leaflet will provide you with information about the evaluation of the training.
What is Mindfulness?
Mindfulness means ‘paying attention in a particular way, on purpose, in the present moment, and non-judgementally’. This means being able to intentionally pay attention to our bodies, emotions and thoughts to be able to monitor our internal reactions to life and respond on a regular basis to reduce stress by employing healthy strategies, meditation, emotion regulation skills, relationship and problem solving skills.
Mindfulness on ******* Ward
The interest in the use of mindfulness–based interventions in clinical settings has become more commonly known particularly in outpatient settings with patients with a range of usually chronic conditions. The therapeutic use of mindfulness has added a new way of promoting engagement and enhancing progress in CBT. There is some evidence that acceptance and mindfulness-based interventions can be usefully adopted in clinical inpatient settings and for challenging problems, for example, borderline personality disorder, complex PTSD and dissociation, psychosis and to enhance treatment team process. There is also evidence that developing mindfulness in staff groups and carers not only improves general wellbeing and satisfaction of the staff group but enhances the therapeutic milieu and therefore outcomes associated with engagement and recovery.
The context of this service development has arisen from the ******* Ward staff team. The CBT Centre has received in increase in referrals for tertiary level intervention for some of the most stuck patients over the last year from referrers across Urgent Care services and in particular from this ward, what these patients had in common was that they were presenting with significant and often chronic emotion regulation difficulties and that these difficulties were thought to be significant in an inability to stabilize and make progress in treatment offered in the setting they were in.
The course
This training course is an 8 week foundation course which has been designed to enable clinical staff to develop mindfulness for themselves. In the longer term training to use specific Mindfulness-Based Interventions will be considered.
The course will take place over 8 weeks for approx. 2 hours per week.
More information about this course will be given at an orientation workshop before the course and evaluation begins.
Evaluation
As a service improvement project this training will be evaluated to look at how effective the course delivered is at enabling participants to develop mindfulness. Impact upon quality of service will also be explored informally.
What do I have to do for this evaluation?
You will be asked before and after the training to complete outcome measures for levels of skills, knowledge and attitudes associated with mindfulness as well as basic levels of wellbeing and satisfaction with the course. A smaller group of participants will be invited to attend a small discussion or focus group before and after the training in which you will be invited to share experiences related to mindfulness and observations about the impact of mindfulness on patient care.
How will my information be used?
Information gathered from outcome measures and from the focus group will be collected anonymously and will be stored securely in accordance with the data protection act. Information will be used solely for the purposes of evaluating the project. An analysis of the information will form part of a report at the end of the project which will be presented at NTW-wide forums, national conferences and also published in national journals. You are welcome to see a copy of the report and/or articles before presentation and/or publication.
Will my taking part be confidential?
During the training we will ask those participating not to divulge anything said in sessions to anyone outside the group of participants. With regards to the evaluation you can give as much information or as little as you wish. No-one will be named in any way in the reports of the study.
Can I withdraw consent for taking part in the evaluation?
Your participation in the evaluation of this project is voluntary and you can withdraw at any time you wish without giving a reason.
Contact information
If you would like further information about the training and/or the evaluation of the training please do not hesitate to contact:
[contact details inserted here]
Learning objectives
At the end of the paper the reader will:
-
(1) Have an understanding of a context in mental health services that supports the introduction of mindfulness skills in clinical staff.
-
(2) Be able to describe the measures used and the rationale for selection of those measures.
-
(3) Be able to describe outcomes of the training in terms of increased mindfulness and its impact upon patient care.
-
(4) Recognize potential areas for further service development and research.







Comments
No Comments have been published for this article.