INTRODUCTION
Depression is a common disease in oncology, with an estimated prevalence of 15% (Hotopf et al., Reference Hotopf, Chidgev and Addington-Hall2002; Mitchell et al., Reference Mitchell, Chan and Bhatti2011). Early identification or diagnosis of depression in cancer patients is an issue of quality of care as its impact on quality of life is severe. Indeed, depression can aggravate such physical symptoms as pain and fatigue (Lloyd-Williams et al., Reference Lloyd-Williams, Dennis and Taylor2004; Rhondali et al., Reference Rhondali, Perceau and Berthiller2012b ). Nearly half of all depressed patients are reported as not being supported for their depression (Lees & Lloyd-Williams, Reference Lees and Lloyd-Williams1999; Rhondali et al., Reference Rhondali, Perceau and Berthiller2012b ), whereas the benefit of such a treatment (antidepressants associated with counseling) has been well established (Rayner et al., Reference Rayner, Price and Evans2010; Reference Rayner, Price and Hotopf2011a ; Reference Rayner, Price and Hotopf2011b ; Hart et al., Reference Hart, Hoyt and Diefenbach2012; Fulcher et al., Reference Fulcher, Badger and Gunter2008; Newell et al., Reference Newell, Sanson-Fisher and Savolainen2002; Strong et al., Reference Strong, Waters and Hibberd2008). More recent studies have shown that it is an independent predictor of cancer mortality (Lloyd-Williams et al., Reference Lloyd-Williams, Shiels and Taylor2009; Satin et al., Reference Satin, Linden and Phillips2009). The missed cases of cancer patients with depression also have significant economic ramifications (e.g., medical and drug consumption, increased length of hospital stay) (Sobocki et al., Reference Sobocki, Jonsson and Angst2006).
This situation can probably be partially explained by the fact that some symptoms—such as fatigue, anorexia, or sleep disorders—can be related to the cancer, to depression, or even to cancer treatments (Lloyd-Williams et al., Reference Lloyd-Williams, Dennis and Taylor2004). We previously proposed to distinguish specific and nonspecific depression symptoms in cancer patients (see Table 1), which was very close to work done by Endicott (Endicott, Reference Endicott1984; Rhondali et al., Reference Rhondali, Perceau and Saltel2012c ; Guan et al., Reference Guan, Sulaiman and Zainal2013). Our goal was mainly to help nonspecialists in mental healthcare to improve their ability to identify depression in cancer patients. There is also the false idea that depression, in the context of cancer, should be considered normal, or at least as an expected issue, along with the confusion between sadness and depression (Rodin et al., Reference Rodin, Lloyd and Katz2007).
Table 1. Symptom importance and specificity for depression diagnosis in cancer patients

For cancer patients, an interview conducted by an experienced psychiatrist based on the DSM–IV–TR (Diagnostic and Statistical Manual–Revision 4) remains the “gold standard” for a diagnosis of depression (Power et al., Reference Power, Kelly and Gilsenan1993; Hotopf, Reference Hotopf, Chidgev and Addington-Hall2002; Meyer et al., Reference Meyer, Sinnott and Seed2003). However, oncology teams that include a psychiatrist or a psycho-oncologist are rare, and it is thus essential for the initial assessment to be conducted by an oncologist or nurse (Stiefel et al., Reference Stiefel, Die Trill and Berney2001). Several studies have explored the agreement between nurses' assessments of patients' psychological distress and/or depression and found that nurses did not identify a large majority of patients who were depressed (Little et al., Reference Little, Dionne and Eaton2005; Rhondali et al., Reference Rhondali, Hui and Kim2012a ).
The current recommended approach to assessing depression in cancer patients is to utilize a scale combined with a clinical assessment (Holland et al., Reference Holland and Bultz2007; Rayner et al., Reference Rayner, Price and Hotopf2011b ), as opposed to just an intuitive judgment. Despite our growing knowledge and the existing international guidelines that recommend systematic screening and active management of depression, implementation in daily clinical practice remains difficult (Jacobsen et al., Reference Jacobsen, Shibata and Siegel2010; Mitchell et al., Reference Mitchell, Kaar and Coggan2008).
The aim of our present study was to explore cancer nurses' perceptions of depression in their patients, and to identify the role they believe that nurses should play in the management of this disease.
METHODS
The local ethics committee and institutional review board of the Hospices Civils de Lyon approved our study.
Participants
We recruited nurses from four different departments caring for cancer patients at Centre Hospitalier de Lyon Sud: palliative care, hematology, medical oncology, and thoracic oncology. The inclusion criteria were that participants should be a nurse in current clinical practice and have responsibility for the care and management of cancer patients. All received information about the study and were invited to participate. We received a list of volunteers from the senior nurse. Written information about the study and its purpose was given to all participants, and a written informed consent was signed before enrollment.
Procedure
All participants were enrolled between February 22 and May 29, 2012. We documented the demographic characteristics of every nurse, including age, sex, specialty, and years in practice. The study was conducted in five steps:
-
• Step 1. The “card-rank test.” Nurses were invited to rank 22 cards representing symptoms, some of which are usually associated with depression (e.g., suicidal ideation, sleep disorders, loss of pleasure), some related to depression but can also be related to cancer and/or its treatment (e.g., anorexia, anxiety, fatigue, feelings of guilt), and some unrelated to depression (e.g., phobias, agitation, delusions) (Froissart et al., Reference Froissart, Chauchat and Terra1985). This list of symptoms was established based on the current literature dealing with depression in palliative care (see Table 1) (Hotopf et al., Reference Hotopf, Chidgev and Addington-Hall2002; Endicott, Reference Endicott1984; Chochinov, Reference Chochinov, Wilson and Enns1994; van der Lee et al., Reference van der Lee, van der Bom and Swarte2005; Breitbart et al., Reference Breitbart, Rosenfeld and Pessin2000; Emanuel et al., Reference Emanuel, Fairclough and Emanuel2000; Akechi et al., Reference Akechi, Okamura and Kugaya2000; Bailey et al., Reference Bailey, Geyen and Scott-Gurnell2005; Rayner et al., Reference Rayner, Price and Hotopf2011a ; Reference Rayner, Loge, Wasteson and Higginson2009). Participants were asked to rank each symptom by importance for the diagnosis of depression in cancer patients from “important” to “not important.” They were asked to include at least 10 symptoms in each of category.
-
• Step 2. After the baseline test, we showed participants a six-minute video of a psychiatric consultation (more information on the video is provided below). This consultation was conducted with a patient volunteer at the comprehensive cancer center who was being evaluated for depressive symptoms. We employed the same video that was used in a previous study for our group showing a complete consultation between a psychiatrist from a comprehensive cancer center and a depressed patient. The video development process was described in a previous work (Rhondali et al., Reference Rhondali, Perceau and Saltel2012c). The institutional ethics committee also approved the six-minute videotape and its use for our study.
-
• Step 3. Immediately after the video, we conducted semistructured interviews. These interviews were set in a private room, and questions were geared toward eliciting open-ended responses to acquire specific information about nurses' perceptions of depression in cancer patients and the role they thought they themselves should play. The specific questions used during the interviews are available on request from the authors. All interviews were audio recorded and then transcribed verbatim. The names and personal information of participants were removed from the transcripts, and participants were assigned a code number. All audio files were kept in a secure location. We conducted two preliminary interviews to test the quality of the questions we planned to use with study participants.
-
• Step 4. The card-rank test was repeated to see if there were any changes.
-
• Step 5. Finally, the nurses were asked to complete a five-item questionnaire about the acceptability and effectiveness of depression screening in cancer patients. This questionnaire is a self-constructed questionnaire that we previously used with oncologists (Rhondali et al., Reference Rhondali, Perceau and Saltel2012c ).
Data Analysis
We summarized nurses' demographic data using descriptive statistics. For analysis of the card-rank test, we employed conventional parametric methods (comparison tests), and we used univariate analyses to examine associations between nurses' characteristics and their responses. For analysis of the card-rank test, we merged the four subcategories into two main categories (“very important” and “important” into “important”; “less important” and “not important” into “not important”). We classified an answer as correct when the participants chose “important” for the related and specific symptoms and “not important” for the related and nonspecific symptoms and the nonrelated symptoms. A value of p < 0.05 was considered significant for all statistical tests. Statistical analyses were performed using SPSS software (version 17, SPSS Inc., Chicago).
We performed qualitative analysis of the interviews using a thematic analysis framed by the “grounded theory” approaches (Chesebro & Borisoff, Reference Chesebro and Borisoff2007), the first step of which was open coding, consisting of multiple reviews of transcripts to identify and categorize data (Lindlof & Taylor, Reference Lindlof and Taylor2002). Two authors (WR and TL) performed this first step independently. The second step divided the interview into “units of meaning” to highlight, in a third step, the underlying meaning of what the participants wanted to express. Careful comparison of interviews identified common elements and differences among participants' responses. During this last step, all the elements were categorized into major themes. The first author (WR) performed the translations of the reported comments. To complete this qualitative analysis, we employed ALCESTE software (Analyse de Lexème Co-occurents dans les Enoncés Simples d'un Texte [analysis of lexeme cooccurrence in a text]), which provided another method of analysis to strengthen our findings. We decided to use it after the thematic analysis in order to not impact the first step with the statistical findings. The hypothesis developed in this program considered distribution of vocabulary in a corpus as a linguistic trace of a cognitive work of the reconstruction of a specific object (Reinert, Reference Reinert1983; Geka & Dargentas, Reference Geka and Dargentas2010). ALCESTE software allows lexical distributional analysis in a short sequence of a corpus to produce “simple statements.” The objective was to obtain a first classification of these statements based on cooccurrences of words in order to identify the main lexical classes. The classes obtained represented the ideas and dominant themes of the corpus. The coefficient of association of a statement to a class was calculated using a chi-square test.
Sample Size Determination
In qualitative research, sample size is determined when none of the analysts recognize new or unique themes. This is known as data saturation. In our study, data saturation occurred after 18 interviews.
Presenting Results
Editing was minimal to preserve authenticity. We used ellipses (. . .) to indicate that part of the quote was truncated when irrelevant information was deleted. When it was necessary to clarify the context, we added information in square brackets [].
RESULTS
We included 18 nurses from four different departments caring for cancer patients—palliative care (n = 5, 28%), hematology (n = 5, 28%), medical oncology (n = 4, 22%), and thoracic oncology (n = 4, 22%)—with 12 women (67%) and a median age of 40 years (Table 2).
Table 2. Nurses' characteristics (n = 18)

*Q1–Q3 = first through third quartiles.
Card-Rank Test Results
Before the interview, more than 70% of participants correctly classified the related and specific symptoms, except for loss of pleasure (61%), requests for hastened death (61%) and psychomotor impairment (56%). For the related but nonspecific symptoms, more than 70% of participants correctly classified only one symptom: anxiety (72%) (Table 3).
Table 3. Rates of correct classification of symptoms related to depression and specific to cancer and symptoms related to depression but not specific to cancer at baseline and after the interview

*Fisher's exact test. #Chi-square test.
Following the interview, more than 70% of participants correctly ranked the related and specific symptoms, with the exception of personal history of depression (51%), requests for hastened death (67%), and psychomotor impairment (33%). More than 70% correctly ranked the related but nonspecific symptoms of fatigue (78%). There were no significant changes when we compared nurses' answers before and after the interview.
For several symptoms, we found significant associations between the correctness of the rating and nurses' characteristics, with inexperienced nurses (i.e., those with fewer years in practice) being more likely to classify sleep disorders (p = 0.004) as less important and weight loss (p = 0.017) more important for a diagnosis of depression than experienced nurses.
Questionnaire Results
According to our final questionnaire (see Table 4), nurses caring for cancer patients endorsed systematic screening (89%) but also expressed the need for training regarding such screening (72%). They also believed themselves to have a role to play in this process (100%).
Table 4. Responses to the questionnaire about screening acceptability and effectiveness (N = 18)

Qualitative Analysis
The average length of an interview was 20 minutes (standard deviation (SD) = 9 min). We identified four main themes: symptoms of depression, depression in the context of cancer, depression management by a mental health specialist, and depression management by nurses.
Depression and Its Symptoms
Nurses identified several common symptoms of depression—such as sadness, anhedonia, social withdrawal, hopelessness, sleep disorders, anxiety, and suicidal ideation—and also changes in their behavior:
(N14) “It is true that the notion of (. . .) sadness, loss of desire, it talks to me pretty well.”
(N4) “It happens to have people who used to come and talk and then don't talk no more.”
(N14) “She [the patient] said that she had no desire to do much; she was less interested in social activities, had some suicidal ideations (. . .) well, to make it more like an accident than a suicide. (. . .) She was not sharp; she was not looking me in the eye.”
Nurses reported that depression is difficult to identify because patients do not admit to feeling depressed, they do not want to show it, and rarely report it spontaneously. Nurses hypothesized that this is because of the negative perception of depression in our society and a patient's desire to protect their own family:
(N1) “There are many [patients] who succeed in hiding it [depression] because they did not want to talk, they will use all their strategies to not show it: ‘I feel that depression in (…) our society, it is not very well considered.’ Finally, (. . .) there are some patients that (. . .) do not accept to say that they are depressed. (. . .) So they hide it. Because they don't want to show their family that they feel bad, because they do not want to hurt them.”
Depression in the Context of Cancer
Several nurses reported that depression in this context should be considered as normal, and that all patients might be subject to depressive symptoms during the cancer journey. Some nurses clearly distinguished adjustment disorders in the context of cancer as an adaptive and normal process as distinct from persistent depressive disorders:
(N1) “If you just tell him that he has a cancer, it is clear that he will react to this announcement. Then, we cannot say right now he is depressed. I mean, this is a reaction to me, which is normal. When you have a cancer diagnosis told to someone, I mean, this is the blow. (. . .) Sometimes it happens that I ask, ‘How is your mood today?’ And the patient answers me, ‘How do you want me to feel today with what they just told me?’”
However, in several interviews we found confusion between sadness, or adjustment disorder, and depression, underlying that a cancer diagnosis is so distressing that depression is always in the air:
(N2) “Well, I think it's so (. . .) it must be so hard to be sick like that (. . .) and I think it [depression] is not very far (. . .) Then either you fall down into depression, or, in all the cases it was touch and go. (. . .) I do not want to say that this is inevitable, but in any case for me, it is a close thing.”
It was very rare that cancer patients expressed or complained of suicidal ideations, and, as for several other symptoms of depression, they reported that suicidal ideation was often hidden behind such somatic symptoms as fatigue and pain, and also psychological symptoms, like anxiety and guilt:
(N7) “They hide their depression with fatigue that is easier to report and/or to complain of in the context of cancer where it is uncommon for patients to tell us, ‘Yes, I have trouble sleeping,’ ‘Yes, I want to kill myself,’ ‘Yes, I cannot read a book or a newspaper anymore.’”
(N9) “I think guilt is the symptom that is most characteristic [of depression].”
We found important variations between nurses from hematology and thoracic oncology regarding requests for hastened death, with more patients expressing this type of request in thoracic oncology:
(N11) “Personally, I have never experienced people who will say, ‘I'll (. . .) I'll jump,’ or ‘I'll take some drugs [to die].’ On the other hand, we had a lot of requests for hastened death. Yes, for active euthanasia (. . .) There are often some requests (. . .) well, patients who say, ‘But push me some product so that it will be over.’”
Finally, several nurses identified that there were some specific times when there was an increased risk for cancer patients to develop depression, such as immediately after completion of specific treatments (because of less follow-up) or recurrence or diagnosis of metastasis:
(N6) “I've noticed that a lot of patients are depressed after, when the treatment [the chemotherapy] is finished. When we (. . .) when we tell them, ‘Well, it goes well, you will simply be monitored,’ and there they just collapse.”
Depression Management by a Mental Health Specialist
Almost all the participants reported that communication with patients about referral to a psychologist/psychiatrist was a real challenge, explaining that in general patients were afraid of mental health specialists. The fear of being referred to a psychiatrist was reported as being greater than of being referred to a psychologist. However, nurses considered that it was part of their job to inform patients about the content of an encounter with a mental health specialist and the associated outcomes in order to facilitate access to care:
(N1) “It is not because you meet with a psychologist that you're crazy. I often explain this [to patients], because there is still the idea that psychologists are for psychos.”
(N16) “I think it is important to distinguish between a psychologist and a psychiatrist for patients. Because psychiatrist (. . .) it means madness and (. . .) it's (. . .) I've already heard, ‘Well no, wait, I do not need a psychiatrist.’”
Nurses also acknowledged that their decision to suggest that a patient be referred to a psychologist or psychiatrist would be based on their feelings or intuition:
(N16) “I propose it (. . .) well, according to what I feel, according to the discussion with the patient.”
Depression Management by Nurses
Nurses reported that they played a pivotal role in mood assessment and depression screening; however, they also had only a limited amount of time to provide psychological support for patients:
(N2) “I think that nurses have a role to play, (…) especially nurses. We spend a lot of hours with [patients]. More than a physician who will perhaps see the patient during the daily visit and at what might be a good time (. . .) Nurses will see the patient during the entire day; they will notice if there is a change in their behavior.”
(N11) “We have less and less time. (. . .) It cost me a lot to say to a patient who is crying, because he or her feels bad or sad, ‘Look, I do not have time to discuss this with you this evening; we'll talk tomorrow about it.’”
Nurses also reported depression as a second-line symptom that they would look for after such physical symptoms as pain, nausea, and dyspnea. We found variations regarding the use of specific tools for depression screening and/or identification among the interviewed nurses, with very few of them reporting that they would use one in their daily practice (n = 2):
(N9) “It's very difficult to be in front of someone who has a serious illness and (. . .) here, to detect (. . .) in fact (. . .) sometimes we find ourselves a little helpless because (. . .) well (…) have something to ask them (. . .) ask questions and to say at the end, well, he is depressed or he is not.”
Finally, nurses described two types of behavior regarding depression management in cancer patients—mothering a patient and stimulation—with several nurses reporting some conflict in the type of care provided to these patients.
Results of the ALCESTE Analysis
The scope of our analysis was on 73% of the full verbatim text (excluding interviewer questions) and revealed four classes of meaning (Table 5). Class 1 consisted of terms related to cancer-related symptoms of depression (fatigue, suicide, hide, mood, loss, fall, withdraw into oneself). This class also contains several words describing the difficulties involved in identifying these symptoms (express, show, hide, sensation, verbalize, look for, describe, speak). Class 2 showed a significant presence of words related to the management of depression, including their own role as nurses (offer, team, call, discuss, time, nurse, explain, systematic, physician, assessment), as well as management by a mental healthcare specialist (psychologist, psychiatrist, management, meet, outside, mindful, interview, antidepressant). In this class, the words offer, discuss, and explain highlight the importance of nurses in patient referral to mental health specialists. Class 3 is related to the cancer itself (cancer, diagnostic, treatment, fight, chemotherapy, recurrence, cure, remission) and the potential impact of cancer on a patient's mood (difficult, chronic, secondary, usually, associated, loose, history, depend, face, resource). Class 4 consisted of specific vocabulary describing the general relationship between cancer patients and nurses (go, leave, take care, go back, stay, touch, understand, try, give). In this class, we can also find several words related to temporality (day, hour, time), highlighting the lack of time nurses have when caring for cancer patients with depression.
Table 5. Specific words from the four classes identified in the corpus*

* Only words with a χ2 result >12 appear in this table.
DISCUSSION
We found that nurses have good general knowledge about the symptoms of depression in cancer patients, and the vast majority of them are able to distinguish specific and important symptoms from nonspecific ones. However, nurses also acknowledged depression as a second-line symptom that they would look for after such physical symptoms as pain, nausea, and dyspnea management. We also found some confusion between sadness and depression in several interviews. Almost all participants reported that they did not employ a screening tool in their daily practice and supplied different reasons for this (e.g., barrier to natural discussion, might scare patients).
Another major finding was that all participants believed that they had a role to play in the management of depression, even if they also acknowledged that they lacked specific training to enhance their confidence in identifying the symptoms of depression. These results are consistent with that of previous work conducted in the United Kingdom (Lloyd-Williams & Payne, Reference Lloyd-Williams and Payne2002; Reference Lloyd-Williams and Payne2003), where nurses reported a lack of training and difficulties in persuading medical staff that patients required further assessment and/or antidepressants.
Our findings suggest that the educational video intervention did not improve nurses' perceptions of depression because there was no significant difference when we compared their answers before and after the interview. For the related and specific symptoms, this is probably because nurses' answers were already correct before the video.
Our findings are different from what we have previously reported regarding the perceptions of oncologists and palliative care physicians about the resources available for systematic screening (Rhondali et al., Reference Rhondali, Perceau and Saltel2012c ). We previously found that physicians considered that they lacked time (62%) and training (55%) to systematically screen patients for depression, whereas in this study we found that the main barrier for nurses to systematically screen patients for depression was training (72%). These results are consistent with the results of the qualitative analysis, with the vast majority of nurses reporting that they were uncomfortable with depressive symptoms as compared to physical symptoms, and especially regarding referrals. These difficulties might be corrected by specific training (Strong et al., Reference Strong, Waters and Hibberd2008) about the availability of specific tools, and communication with patients about referral to mental healthcare services. This type of training could also help nurses understand when the team should decide whether to adopt a mothering or a stimulating approach. It is also important to reinforce collaboration between nurses and psychologists to prevent nurses from being involved in counseling tasks. Finally, our results suggest that nurses missed some resources (especially training) to be able to correctly manage depression in cancer patients.
Based on previous studies (e.g., Rhondali et al., Reference Rhondali, Perceau and Saltel2012c ; Reference Rhondali, Chirac and Laurent2013), we would like to propose an algorithm defining the possible roles of all care partners, including patients' caregivers (Figure 1). This algorithm follows the National Comprehensive Cancer Network (NCCN) and European Association for Palliative Care (EAPC) guidelines (Holland et al., Reference Holland and Bultz2007; Rayner et al., Reference Rayner, Price and Hotopf2011a ) and aims to allow all care partners to be involved in depression management according to their skills and resources. Further research should test this type of strategy, using specific tools according to the clinical setting and population.
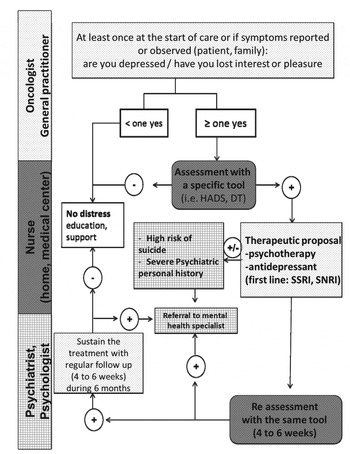
Fig. 1. Algorithm for management of depression according to profession of the healthcare provider. HADS, Hospital Anxiety Depression Scale; DT, Distress Thermometer; SSRI, selective serotonin reuptake inhibitor; SNRI, serotonin–norepinephrine reuptake inhibitor.
More research is necessary to confirm our findings and to better determine the best way to support nurses, as well as all care partners, for the purpose of depression management in cancer patients.
ACKNOWLEDGMENTS
This research was supported by a grant from the Fondation APICIL and the Fondation de France. The authors state that they have no conflicts of interest to declare.








