Introduction
Recent calls to improve survival from out-of-hospital cardiac arrest (OHCA) 1 , Reference Neumar, Shuster and Callaway 2 have led to the development, implementation, and study of “high-performance cardiopulmonary resuscitation (CPR)” in many Emergency Medical Services (EMS) systems.Reference Bobrow, Eisenberg and Panczyk 3 - Reference Levy, Yost, Walker, Scheunemann and Mendive 5 High-performance CPR has been defined as “the delivery of minimally interrupted chest compressions with the proper target rate, depth, and release, synchronized with appropriate ventilations and attempts at defibrillation;” in other words, the focus is not solely on the percentage of cases receiving CPR or receiving CPR quickly, but on the provision of high-quality resuscitation that meets all current standards of care and practice.Reference Bobrow, Eisenberg and Panczyk 3 Its implementation has been instrumental in achieving higher rates of both overall and neurologically-intact survival from OHCA in implementing systems.Reference Hopkins, Burk, Moser, Meersman, Baldwin and Youngquist 4 , Reference Hansen, Kragholm and Pearson 6
For cardiac arrests reported to 911, professional CPR typically begins once the first EMS responders arrive on scene—yet, average response times generally range between four and seven minutes in urban and suburban locales, and potentially much longer in rural areas.Reference Persse, Key, Bradley, Miller and Dhingra 7 - Reference Sladjana, Gordana and Ana 11 Given that the likelihood of survival from OHCA decreases with each minute without resuscitation,Reference Larsen, Eisenberg, Cummins and Hallstrom 12 , Reference Gold, Fahrenbruch, Rea and Eisenberg 13 calls for comprehensive, high-performance CPR must include recommendations for implementation of dispatcher-assisted CPR (DA-CPR; also called telephone CPR or tCPR). Dispatcher-assisted CPR is the provision of CPR instructions over the phone to a layperson-caller by a trained emergency medical dispatcher (EMD); DA-CPR has been shown to increase both overall and neurologically-intact survival from OHCAReference Hansen, Kragholm and Pearson 6 , Reference Song, Shin and Park 14 , Reference Rea, Eisenberg, Culley and Becker 15 since resuscitation attempts can often begin significantly earlier (ie, closer to the time of patient collapse).
While a few studies and position papers have called for the implementation of DA-CPR as part of an overall high-performance CPR system implementation, they provide very few specifics for providing high-quality DA-CPR beyond the mention of early identification of cardiac arrest and rapid “hands-on-chest” time by bystanders.Reference Bobrow, Eisenberg and Panczyk 3 , Reference Lewis, Stubbs and Eisenberg 16 Early arrest recognition and short hands-on-chest times are critically important, but they should not be the only measures of quality applied to DA-CPR. Just as with high-performance CPR for field EMS providers, DA-CPR should be measured and evaluated on its ability to provide compressions of the correct rate and depth.
Several previous studies have investigated the effects of metronomes in simulated DA-CPR settings, with a trained professional providing instructions to untrained laypersons.Reference Rasmussen, Nebsbjerg and Krogh 17 - Reference Kim, Lee, Lee, Lim and Kim 19 These studies show marked improvements in compression rate when using the metronome to control rhythm during layperson-delivered compressions, suggesting that such changes to dispatcher practice have the potential to improve layperson-caller CPR during a real cardiac arrest.
However, these studies had significant limitations. Two of the three studies required callers to place the phone on speaker before giving instructions (removing that requirement from the instruction sequence itself). All gave the CPR instructions as a standalone process—not within the context of a call or the simulated experience of finding a collapsed person and having to dial 911, report the problem, and so on. One study even gave the callers, as well as the dispatchers, pre-written scripts. Another simultaneously tested multiple (non-metronome-related) novel changes to the DA-CPR instructions, and all used recently-developed scripts and procedures designed solely for the study setting, untested in a true live-dispatch environment. What has yet to be studied is the use of a metronome in the context of a complete cardiac arrest discovery scenario, with the complexities and caller variation that go along with that. Moreover, no study has tested the integration of a metronome tool into an established medical dispatch protocol with demonstrated usability in such complex, real-world events.
The primary objective of this study was to assess the effect of a dispatcher-controlled Compression Monitor Diagnostic Tool (ie, a software-embedded, automated metronome tool), set at a rate of 100 compressions per minute (cpm), on both the rate and depth (mm) of layperson-caller-performed chest compressions. The hypothesis was that use of the metronome tool would increase the proportion of callers able to perform CPR within the target rate without affecting depth.
Methods
Design and Setting
This prospective, randomized, controlled study was conducted by simulating cardiac arrest calls to 911 using layperson-caller participants at four locations in Salt Lake City, Utah USA: a high school, an assisted-living residential facility, a community college, and a state (flagship) university. Generally, the study was conducted for a full day at each location. Sites were chosen to provide as broad a range of ages, experience levels, and backgrounds as possible.
The high school, a secondary school established in 1999, had a population of approximately 800 students, but for the study, only students from four health classes participated. This population comprised 100 students, age range 14-17 years; a majority (53.0%) were female.
The assisted-living location was an active senior living community that provided independent care for older adults and those who required some assistance with basic chores and tasks. The facility housed approximately 90-100 residents, age 34-94 years; a majority (65.0%) of the population were female.
The community college had nine campuses across the state, with a student population of over 62,150. One campus, with a population of 32,003 students, was involved in the study. At this campus, 52.0% of the students were female, 17.0% of the students were younger than 18 years old, 43.0% were 18-24, and 39.0% were 25-64. There were no students 65 years old or older.
At the time of the study, the state university had a student population of 32,062, of which 55.3% was male. Additionally, approximately 54.0% were 25 years old and younger, with 41.0% between 18-22 years.
The Compressions Monitor Studied
The Compressions Monitor Diagnostic Tool included in the automated (software) version of the Medical Priority Dispatch System (MPDS; MPDS version 13.0, released 2015; Priority Dispatch Corp.; Salt Lake City, Utah USA; Figure 1) is designed to help EMDs instruct layperson-callers in providing effective compressions during DA-CPR. This Tool provides a visual screen display for the EMD that dynamically paces the EMD at a compression rate of 100 cpm, as he/she calls out this rate to the bystander delivering chest compressions to a patient in arrest.
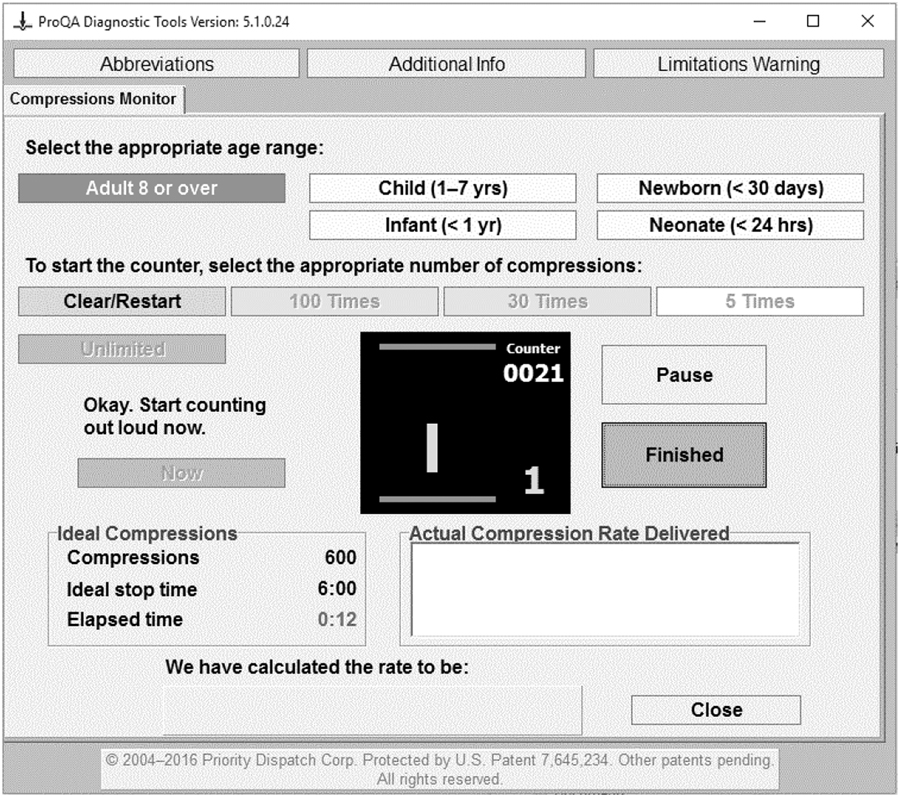
Figure 1 MPDS Version 13.0 Metronome – Compressions Monitor Diagnostic Tool. Note: Copyright International Academies of Emergency Dispatch—used with permission. Abbreviation: MPDS, Medical Priority Dispatch System.
Study Population and Procedures
Institutional Review Board approval was obtained from the International Academies of Emergency Dispatch (IAED) IRB (Salt Lake City, Utah USA). All participants aged 14 years and older were eligible to be enrolled into the study. Informed written consent was obtained from each participant (or a parent/guardian). Two EMDs actively employed in a 911 center and currently certified in the latest MPDS version (MPDS v13.0, 2015; IAED) and two CPR recording manikins were used to simulate 911 calls for cardiac arrest. Consenting participants were assigned in parallel to an experimental or control group in sequence based on separate pre-designed randomization lists for each EMD. Randomization lists were generated using STATA (STATA Statistical Software: releases 14.2; StataCorp; College Station, Texas USA). Approximately 50.0% allocations were used—50.0% of each EMD’s randomization list was control and 50.0% was experimental. Prior simulation studies on randomized, controlled, metronome-guided CPR quality suggested a 30.0% difference in the proportion of appropriate compression rates by study group,Reference Kern, Stickney and Gallison 20 - Reference Jantti, Silfvast and Turpeinen 22 with the most recent study finding a 27.0% difference.Reference Park, Hong and Shin 23 Thus, assuming 77.0% of the experimental group would have an appropriate compression rate compared to 50.0% in the control group, a sample size of 49 would be required in each group (98 total) using 80.0% power and a 5.0% Type I error (a 0.05 significance level cut-off).
In the experimental (metronome) group, the assigned EMD provided the bystander-callers with the most current MPDS-scripted, pre-arrival instructions for performing compression-only CPR with the use of the metronome tool, a software feature embedded into the dispatch protocol system, which included the EMD counting aloud for each compression (100 cpm) at a repeating cadence of “one, two, three, four” and instructing the caller to follow along. Participants delivered compressions on a manikin for two minutes and were instructed to stop once the total time was up. For the control group, bystander-callers were given exactly the same scripted pre-arrival instructions for compressions, eliminating only the “count out loud” instruction and the use of the Tool itself. Gender, age, CPR training (yes/no), compression rate (cpm), and compression depth (in millimeters [mm]) data were collected from all participants.
Outcome Measures
The primary endpoints of the study were the layperson-caller’s compression rate, the compression depth, and the number of layperson-callers who achieved the compression rate (100-120 cpm) and/or depth (50-60 mm), as recommended by the 2015 American Heart Association (AHA; Dallas, Texas USA) guidelines.Reference Neumar, Shuster and Callaway 2 All endpoints were assessed at the time of the simulation.
Data Analysis
R-3.3.3 for Windows (R Foundation for Statistical Computing; Vienna, Austria) language and environment for statistical computing was used for data analysis. 24 Descriptive statistics characterized participants’ categorical baseline measures: gender, age, location (study site), and CPR training status. Associations between categorical measures were assessed using Fisher’s exact test and an exact Cochran-Mantel Haenszel test. For continuous measures, the equality of median compression rates and depth by study group were assessed using a Median test and presented on boxplots. Kendall’s rank correlation coefficient quantified the association between compression rate and compression depth, stratified by study group. Overall, inter-group differences were assessed at the 0.05 significance level.
Results
A total of 148 layperson-callers were included in the study (Figure 2). Of these, 57.4% (n=85) were assigned to the experimental group. Overall, the population studied was predominantly female (56.8%). In the control group, 65.1% were female, while the experimental group was equivalently distributed by gender (50.6% female and 49.4% male; Table 1). The median age was 19 years, with the population evenly distributed on the median. Of the four recruitment locations, the highest percentage of participants (36.5%) came from the state university, and the smallest percentage (10.1%) from the assisted-living facility. A majority (56.1%) of the participants reported as having prior CPR training: 63.5% in the control group and 50.6% in the experimental group.
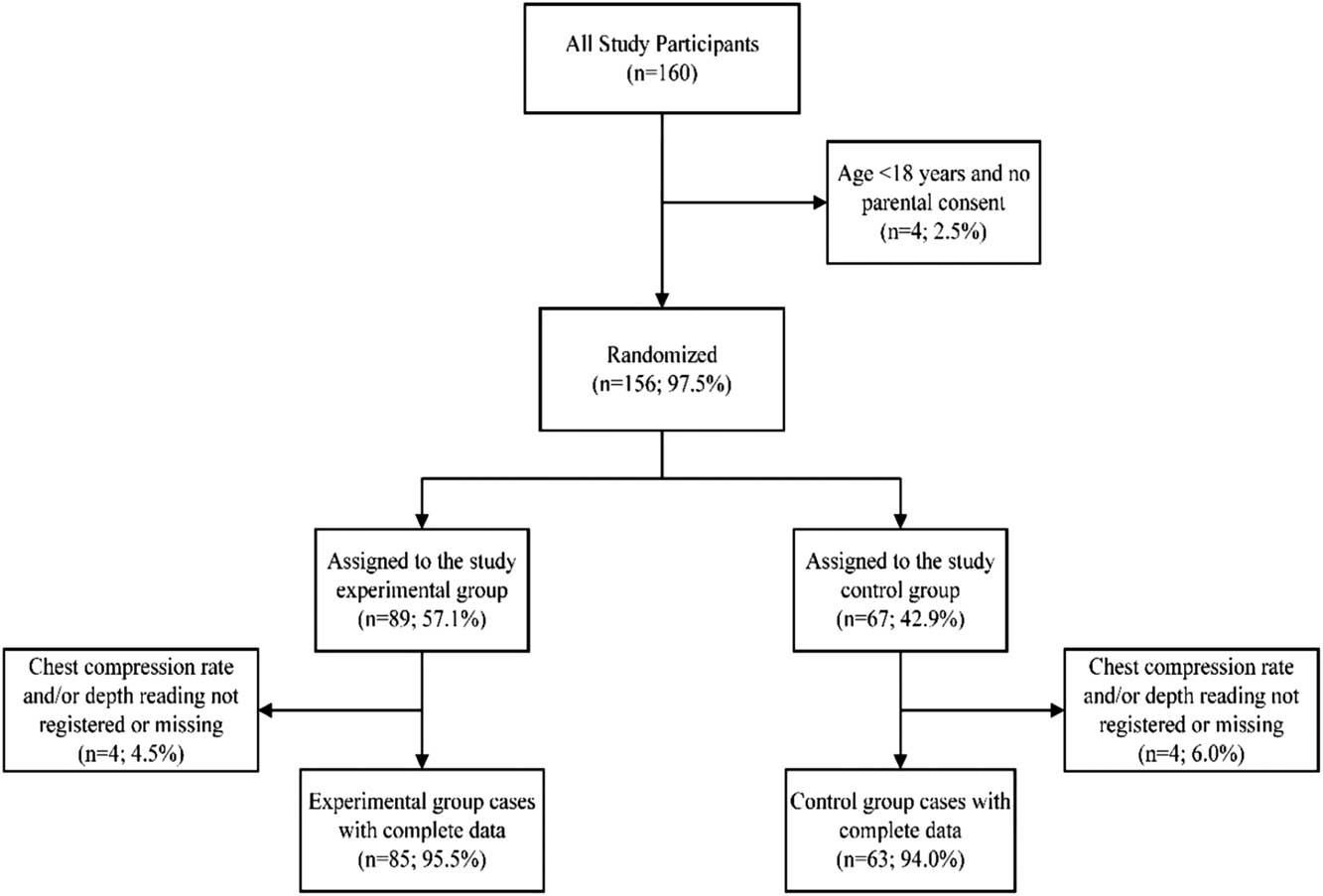
Figure 2 Randomization Flow Chart.
Table 1 Baseline Demographics

Abbreviation: CPR, cardiopulmonary resuscitation.
A considerable number of the participants achieved the target compression rate of 100 cpm, both overall (35.8%) and within each of the study groups (22.2% for the control group and 45.9% for the experimental; Table 2). However, very few participants performed within the AHA-recommended compression depth range of 50-60 mm,Reference Jimenez, Padro and Garcia 9 both overall (4.1%) and for each of the study groups (3.2% in the control group and 4.7% in the experimental group). The majority provided compressions shallower than the recommended minimum of 50 mm.
Table 2 Achievement of Target Compression Rate and Depth by Study Group
Overall, there was a statistically significant association in the number of participants who performed an AHA-recommended compression rate between the control and experimental groups (Fisher’s exact; P=.003).
Furthermore, the experimental group had a significantly higher median compression rate than the control group (100 cpm and 89 cpm, respectively; Median test: P=.013). In contrast, there was no significant difference in the median depth by group (Figure 3). Overall, a slight decrease in the compression depth was observed for the experimental group as compared to the control group. However, the compression rate and compression depth were not significantly correlated, nor was there a significant association between compression depth and study group by compression rate (100-120 cpm vs <100 cpm or >120 cpm; P=.765). Additionally, the proportion of participants who performed outside the AHA-recommended guidelines for compression rate (100-120 cpm) and compression depth (50-60mm) did not significantly differ by baseline demographic covariates (eg, gender, age, study site, and CPR training).
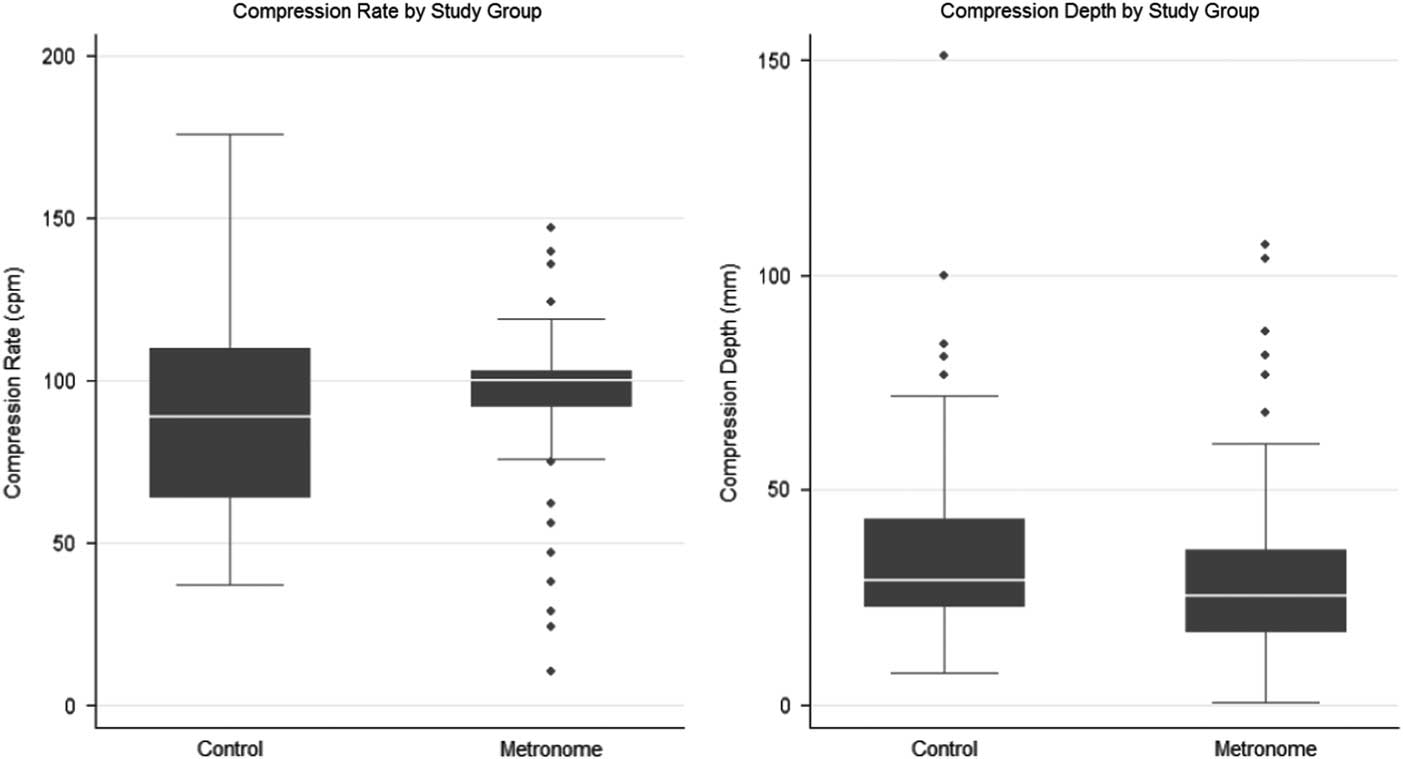
Figure 3 Compression Rate and Depth Classified by Study Group.
Discussion
In evaluating DA-CPR, measures of CPR quality (including compression rate and depth) provide information about the actual effectiveness of CPR interventions by layperson-callers on the scene—over and above the questions of whether CPR is performed at all and how long it takes to begin compressions. In this study, use of the Compressions Monitor Diagnostic Tool allowed trained EMDs to achieve a median compression rate of exactly the target 100 cpm among layperson-callers providing DA-CPR with no significant effect on compression depth.
Previous studies testing CPR quality using a metronome in DA-CPR found similar results. For example, RassmussenReference Rasmussen, Nebsbjerg and Krogh 17 demonstrated an overall improvement in meeting the target compression rate (110 cpm), while ParkReference Park, Hong, Shin, Lee and Hwang 18 performed a randomized, controlled simulation test with use of a metronome sound-producing device played to a rescuer on a cellphone speaker during a simulated DA-CPR phone call. Park’s findings showed significant improvement in compression rate in the experimental group. Park reported no significant mean change in compression depth between the two groups, but also found more individual subjects that failed to meet the minimum target depth of 38mm in the metronome group, at a level of significance (P=.035).
However, previous studies of metronome use for DA-CPR have taken the CPR instruction sequence out of the context in which such tools are meant to be used. Providing callers with prewritten scripts, providing a CPR instruction sequence as a stand-alone test, and writing special instruction sets for the test that have never been used in a live emergency dispatch environment—all of these tend to divorce these tests from the complex, sometimes chaotic, and often emotional reality of a 911 call made following the discovery of a collapsed person in cardiac arrest. Moreover, and perhaps most importantly, not one of them used actual emergency dispatchers to provide instructions; instead, they relied on clinical professionals (such as doctors) who may perform or provide instructions very differently during a call than a trained and experienced emergency dispatcher would. Any tool for the provision of instructions in the dispatch environment must work not only in “sterile” or controlled conditions, but also in the context of a real call. Although it is not possible in most cases to conduct prospective tests of instruction sequences during real live calls, this study did create a realistic, complete 911 calling simulation, with working emergency dispatchers and the requirement that the participant check the manikin, call 911, and work through the entire sequence of questions and instructions without scripts, training, or assistance from the researchers, just like a caller in a true emergency situation. The simulation was successful enough that many participants reported feeling anxiety and fear, being afraid that they would “hurt” the manikin, and other indications that the simulation was realistic enough to provide an effective test. The fact that the instructions provided are part of a protocol already in wide use in live emergency dispatch centers, and were effectively provided by working emergency dispatchers, also ensures that these instructions were realistic and the metronome actually capable of integration into the flow of a live 911 call.
In both the studies described above, the metronomes were set to a rate of 110 cpm—the midpoint of the AHA’s suggested range of 100-120 cpm.Reference Conway, McDavid, Emert, Kudenchuk, Stubbs and Rea 10 Other studies of metronomes to improve CPR quality have instead applied a rate of 100 cpm,Reference Kim, Lee, Lee, Lim and Kim 19 , Reference Kim, Hwang and Cha 25 - Reference Hafner, Jou, Wang, Bleess and Tham 27 as was done in this study. In the non-dispatch environment, studies examining rescuer fatigue and the effect of higher per-minute compression target rates such as 110, 120, or higher on overall CPR quality have shown differing results, and there is some indication that higher rates may be associated with less-effective depth.Reference Monsieurs, DeMelissa and Vansteelandt 28 Given the relative scarcity of research in this area and the consensus that effective depth is critical to CPR quality,Reference Bae, Chung and Je 29 , Reference Stiell, Brown and Nichol 30 future research should further examine whether increasing the rate of an automated metronome above 100 cpm in the DA-CPR environment could have a detrimental effect on compression depth. Achieving recommended compression depth during DA-CPR remains a challenge, and the metronome device tested in this study did nothing to improve the sub-optimal performance for that metric.
Limitations
Some limitations were identified in conducting this study. Since three of the four study sites were educational institutions, the majority of the population were young adults (minimum age 15), and a smaller percentage were elderly. These groups may not perform similarly to one another and are not interchangeable. Further, they are not a proportional representation of age in the general population. Two manikins were used at two of the four test sites, and it is possible that the manikins were not calibrated exactly the same. Participants with missing data were those who were unable to perform CPR such that the manikin could capture the data. These participants’ data (n=8) were discarded. Finally, the effect of the metronome was not tested on another key CPR metric: release (also known as recoil). This was left out due to some missing data and the lack of an effective quantitative measure (ie, the manikin data could indicate only whether or not the release was complete or incomplete, which did not lend itself well to useful analysis).
Conclusion
Emergency medical dispatchers using a software-based metronome tool embedded into their protocols can improve bystander compression rate during DA-CPR with no significant change in compression depth. Moreover, they can do so in a realistic scenario that mimics the complexities of a true emergency call to 911. These finding suggest that such a metronome should be a standard and required element of DA-CPR protocols.







