Introduction
Prostate cancer is the most common cancer diagnosed in males in the United States. In 2016, approximately 180,890 new prostate cancer cases were diagnosed and roughly 26,120 deaths will occur from this disease. It has been statistically demonstrated that one in seven men will be affected by prostate cancer in his lifetime.Reference Siegel, Miller and Jemal1 Though there are many treatment options for this disease, radical prostatectomy followed by external beam radiation therapy is commonly used in patients with positive surgical margins, rising prostate specific antigen or with extra prostatic extension. Randomised trials have shown that post-prostatectomy radiotherapy improves progression-free survival and/or overall survival in this group of patients.Reference Thompson, Tangen and Taradelo2–Reference Thompson, Valicenti and Albertsen6 Radiation dose escalation to the prostate bed also is sought to further enhance the tumoricidal effect of external beam radiation therapy, while minimising gastrointestinal and genitourinary toxicities.Reference Goldin, Sheets and Meyer7, Reference Zelefsky, Levin and Hunt8
Target accuracy is crucial, particularly when utilising high precision radiation therapy techniques such as intensity modulated radiation therapy (IMRT) and volumetric modulated arc therapy (VMAT). These techniques generate a steep dose fall off and deliver highly conformal radiation doses to the target, while minimising dose to normal, healthy tissues.Reference Palma, Vollans and James9, Reference Zhang, Happersett and Hunt10 The precision and effectiveness of post-prostatectomy radiotherapy require accurate localisation of the prostate bed. In addition, internal organ motion such as daily variations in rectal and bladder filling causes prostate bed motion; if left undetected, it may result in target underdosing and normal tissue overdosing. The traditional method of target localisation by aligning bony anatomy rather than visualising the target or its surrogate markers has been proven suboptimal.Reference Schiffner, Gottschalk and Lometti11 Various image-guided radiation therapy (IGRT) methods have been used to assess prostate bed motion such as ultrasound, cone beam CT (CBCT), electronic portal imaging, kilovoltage (KV) orthogonal imaging, surgical clips and gold seed fiducial markers.Reference Shakir, Udrescu and Enachescu12–Reference Bell, Cox, Eade, Rinks and Kneebone22
The use of fiducials specifically in post-prostatectomy patients has been uncommon due to the lack of an intact organ where they can be implanted.Reference Langenhuijsen, Donker, Mccoll, Kiemeney, Witjes and Lin23 The present study was undertaken to determine the feasibility of using gold seed fiducial markers for prostate bed localisation, determine the magnitude of prostate bed motion and provide recommendations regarding appropriate planning target volume (PTV) margins in post-prostatectomy radiation therapy.
Materials and Methods
Patients
Treatment records of prostatectomy patients treated between 2013 and 2016 with VMAT and gold seed fiducial markers were studied after obtaining approval by our Institutional Review Board. All patients were treated on a Varian Truebeam Linear Accelerator (Varian Medical Systems Inc., Palo Alto, CA, USA). The PTV was generated by placing a uniform expansion around the prostate bed of 8 mm except posteriorly where the margin was 5 mm (Figures 1a and 1b). The prescribed radiation dose to the PTV ranged from 64·8 to 72 Gy at 1·8 Gy per treatment fraction.
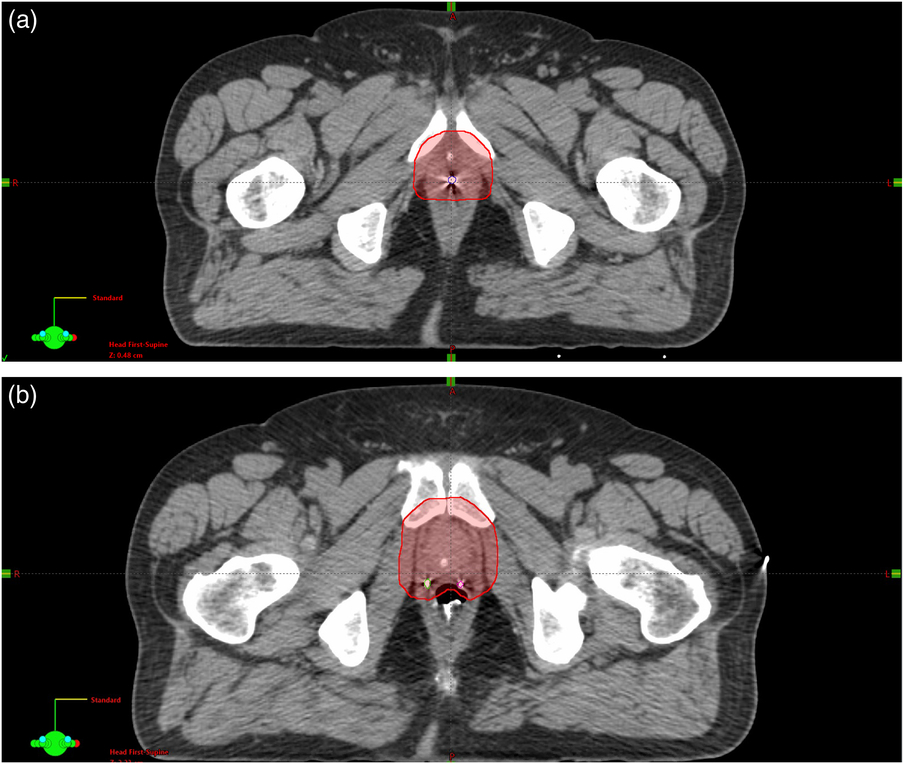
Figure 1. (a and b) Planning CT axial slices demonstrating the planning target volume and location of the fiducial markers.
Three gold seed fiducial markers were implanted in the prostate bed by the urologist in a triangulated fashion around the urethrovesical anastomosis; two fiducial markers were placed proximally to the urethrovesical anastomosis and laterally on each side of the prostate fossa and the third distally to the urethrovesical anastomosis. The specifications of the fiducial markers have been published elsewhere.Reference Shakir, Udrescu and Enachescu12 In summary, fiducial markers are cylindrical in shape and made of 24-carat gold. They measure 0·5–1·5 mm in diameter and 2–5 mm in length. They have cross-like markings on their surface to securely attach to soft tissue and minimise the possibility of migration. Their composition allows them to be visualised on magnetic resonance imaging (MRI) and CT with minimal artefact.
Prostate bed motion
Throughout the radiotherapy course, the patients were set up for treatment using the skin marks placed at the time of CT simulation and pretreatment KV orthogonal images were taken. The number of images obtained was based on the radiation oncologist’s orders and varied on a case-by-case basis. The shifts were made by the radiation therapists based on KV/KV matching and alignments were made in relation to the location of the gold seed fiducial markers from the digitally reconstructed radiographs from the planning CT. As a result, each shift incorporated the set-up error and was performed and recorded in centimeters. The orthogonal images were assessed offline for 386 pairs by the same radiation oncologist (PC) and the shifts that were made in the superior to inferior (S/I), left to right (L/R) and anterior to posterior (A/P) directions were recorded. By convention, negative values represented shifts in the inferior, left and posterior directions while positive values represented shifts in the superior, right and anterior directions.
Results
Eighteen post-prostatectomy patients treated with the VMAT and gold seed fiducial markers were included in the study and were de-identified. All patients except for one were Caucasian. Age ranged between 58 and 72 years. A total of 386 KV orthogonal pair images were reviewed for these 18 patients. The average number of KV pairs recorded per patient was 21.
The mean fiducial marker shifts were 0·34 cm (0·31 SD) in the S/I, 0·31 cm (0·29 SD) in the A/P and 0·28 cm (0·25 SD) in the lateral direction. As a result, the 95% probability of fiducial marker displacement was 0·96 cm in the S/I, 0·89 cm in the A/P and 0·78 cm in the R/L axes. Table 1 shows the mean, minimum and maximum prostate bed shifts in the S/I, A/P and lateral direction for each patient. The percentage of shifts more than 0·5 cm were 19·74% for the S/I, 21·56% for the A/P and 12·47% for the R/L axes. Zero shifts occurred in 56, 90 and 85 occasions for the S/I, A/P and R/L directions, respectively (Table 2). The most common direction for the motion of the prostate bed was inferior, left and posterior from the original position of the fiducial markers on the planning CT (Figures 2a, 2b and 2c). Figures 3a, 3b and 3c demonstrate the frequency of the fiducial marker shifts in each of the three directions.
Table 1. Mean prostate bed shifts (in cm, minimum and maximum shifts in parenthesis) for each patient in the superior–inferior (S/I), anterior–posterior (A/P) and lateral (R/L) directions. Inferior, left and posterior shifts are preceded with the negative sign. Zero indicates no shift. The ± sign indicates equal magnitude of shifts in both directions. The last column demonstrates the number of observations per patient

Table 2. Cumulative prostate bed motion statistics for all patients

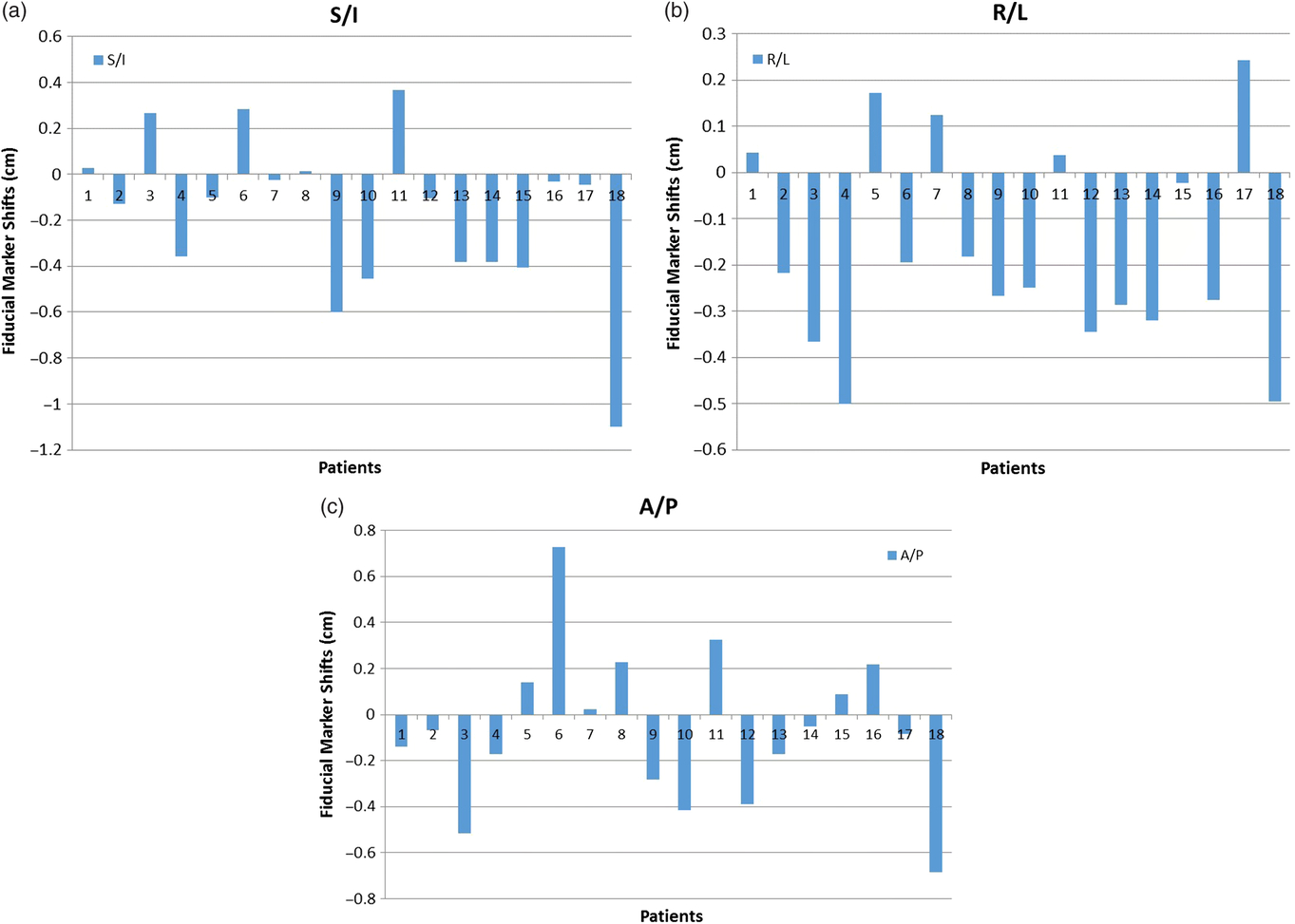
Figure 2. Prostate bed motion (cm) occurs predominantly in the inferior (a), left (b) and posterior (c) direction.

Figure 3. Frequency of prostate bed shifts above 0·2 and 0·5 cm in the superior–inferior (a), lateral (b) and anterior–posterior (c) direction.
Discussion
The goal of high-precision radiotherapy techniques such as IMRT and VMAT is to deliver highly conformal doses to the target, while sparing healthy, surrounding tissues. In post-prostatectomy patients, the prostate bed corresponds to the anatomical volume of the removed prostate gland where subsequently bladder and rectal tissue shift. It is therefore of paramount importance to develop IGRT techniques that accurately and reproducibly localise the prostate bed and ensure optimal radiation coverage of the subclinical disease while avoiding unnecessary radiation exposure of the uninvolved bladder and rectum. Since an intact organ is lacking in post-prostatectomy radiotherapy, fiducial markers and surgical clips have been used as surrogates for the localisation of the prostate bed.
The technique and complication rate for ultrasound guided transrectal implantation of gold fiducial markers has been described in detail by Langenhuiujsen et al.Reference Langenhuijsen, Donker, Mccoll, Kiemeney, Witjes and Lin23 In this study of 77 patients, failure of marker implantation or marker migration was observed in 6 cases. The incidence of rectal bleeding, urinary urgency and macroscopic hematuria more than 3 days were 13, 0 and 1%, respectively. The authors concluded that the use of fiducial markers was a feasible and safe approach for prostate bed localisation.
Shakir et al. evaluated the positional stability of fiducial markers in seven patients who underwent prostate bed salvage radiotherapy due to the presence of macroscopic recurrence.Reference Shakir, Udrescu and Enachescu12 The radiotherapy dose was 60 Gy to the prostate bed and 72 Gy to the recurrent nodule. The distance variation between the fiducial markers was found to be ≤1 mm in 72% and ≤2 mm in 94·3%. The Shakir et al. study concluded that fiducial markers migrate minimally and can be reliably used as surrogates for prostate bed localisation.
Using fiducial markers, Alander et al. reported prostate bed positioning error of 1·2 mm (1·8 SD), 0·3 mm (2·9 SD) and 0·4 mm (2·7 SD) in the L/R, S/I and A/P axes, respectively.Reference Ålander, Visapää, Kouri, Keyriläinen, Saarilahti and Tenhunen13 Similar results were reported by other investigators using surgical clips rather than fiducial markers for prostate localisation. In a study of 17 patients, Song et al. reported prostate bed shifts of −0·1 mm (1·7 SD) in the L/R, 0·6 mm (2·4 SD) in the S/I and −2·1 mm (2·6 SD) in the A/P directions. The authors concluded that without fiducial markers or other forms of IGRT, non-uniform PTV margins of 6, 9 and 8 mm are required in the L/R, S/I and A/P axes to achieve 95% probability of adequate prostate bed coverage during radiotherapy.Reference Song, Yenice, Kopec and Liauw19 This finding is very similar to the current analysis. Fiducial markers have been compared and found to be advantageous compared to surgical clips. Fortin et al., reported less inter-observer variability with fiducial markers. Moreover, surgical clip mismatching of ≥2 mm was seen in 68% of treatments. The authors concluded that the fiducial markers may be proven beneficial in reducing PTV margins.Reference Fortin, Carrier, Beauchemin, Béliveau-Nadeau, Delouya and Taussky14
CT on rails has also been used to assess prostate bed motion.Reference Cavalieri, Gay and Liu15 In a study of 17 patients treated to the prostate bed with IMRT, 661 images were analysed and demonstrated significant prostate bed motion. Specifically, 11·5, 20·9 and 31·2% required a shift of 6–10 mm while 1·7, 3·8 and 5·5% required a shift greater than 10 mm in the R/L, S/I and A/P axes, respectively.
Huang et al. studied interfraction and intrafraction uncertainty utilising CBCT in post-prostatectomy patients. CBCT was obtained at initial patient set-up, after correction shifting and at the end of the treatment. The study concluded that a margin of at least 3–5 mm with IGRT and 4–7 mm without IGRT should be used to ensure that 95% of the prescribed dose be delivered to the target volume in 90% of patients.Reference Huang, Palma and Scott16
Using the Calypso 4D localisation System (Varian Medical Systems Inc.), Klayton et al. reported on 20 post-prostatectomy patients who had three implanted radiofrequency transponders for prostate bed localisation and real-time tracking during the course of radiation therapy. Prostate bed displacement in excess of 5 mm occurred in 9 and 21% of fractions in A/P and S/I axes, respectively. Moreover, intrafraction motion of more than 5 mm for at least 30 seconds was noted in 11% of treatment fractions and treatment interruption for patient repositioning occurred in 15% of all treatments.Reference Klayton, Price and Buyyounouski17
Gill et al. studied prostate bed deformation by analysing 477 CBCTs in 50 post-prostatectomy patients planned using two different prostate bed to PTV expansions: (1) 10 mm isometric expansion (PTV10) and (2) 5 mm posterior expansion and 10 mm in all other directions (PTV5). Irrespective of the PTV size, 43 of 477 CBCTs had anterior geometric misses. Posterior geometric misses were also seen in 26 CBCTs for PTV10 and 46 CBCTs for PTV5. Moreover, the magnitude and direction of shifts differed for the superior versus the inferior part of the prostate bed. The authors concluded that adaptive radiotherapy may prove useful in accounting for prostate bed deformation and should be studied further.Reference Gill, Isiah and Adams24
In our study, the average fiducial marker shifts were 0·34 cm (0·31 SD) in the S/I, 0·31 cm (0·29 SD) in the A/P and 0·28 cm (0·25 SD) in the R/L axes. As a result, the 95% probability of fiducial marker displacement was 0·96 cm in the S/I, 0·89 cm in the A/P and 0·78 cm in the R/L axes. In addition, the percentage of shifts more than 5 mm were 19·74% for the S/I, 21·56% for the A/P and 12·47% for the R/L axes. These results indicate that without fiducial markers, non-uniform minimum PTV margins of 1 cm for S/I, 9 mm for A/P and 8 mm for the lateral direction are necessary to achieve adequate prostate bed dose coverage. Wider margins may be necessary to account for intrafraction motion and prostate bed deformation which were not addressed in the present study.Reference Klayton, Price and Buyyounouski17, Reference Gill, Isiah and Adams24 Moreover, strict bladder and rectal filling protocols may prove beneficial in minimising prostate bed motion and deformation.
Conclusion
Gold seed fiducial marker shifts function as surrogates for prostate bed motion and can improve prostate bed localisation in post-prostatectomy radiotherapy. In the absence of fiducial markers, minimum PTV margins of 0·8–1 cm are required for target localisation. Their use can result in decreased PTV margins especially when using high-precision radiotherapy techniques such as VMAT. Additional IGRT studies using real-time tracking and improved prostate bed/normal tissue definition such as MRI may further assist in determining prostate bed deformation and defining the magnitude of inter- and intrafraction prostate bed motion.Reference Klayton, Price and Buyyounouski17, Reference Gill, Isiah and Adams24
This has the potential of improving the risk benefit ratio of post-prostatectomy radiotherapy and allow for dose-escalated and/or hypofractionated clinical regimens to be considered.
Acknowledgements
None.
Conflict of Interest
The authors have no conflicts of interest to disclose.







