Introduction
Sphenoid sinus mucocele is a rare condition which represents only 1–2 per cent of all paranasal sinus mucoceles.Reference Kosling, Hinter, Brandt, Schulz and Bloching1 To date, only 140 cases have been reported.Reference Righini, Darouassi, Boubagra, Schmerber and Reyt2 The pathophysiology of this lesion is still uncertain, but it is generally thought to be caused by obstruction of the sinus ostium. Other hypotheses include cystic dilatation of glandular structures and cystic development from embryonic epithelial residues.Reference Kosling, Hinter, Brandt, Schulz and Bloching1
Patients may present with a myriad of symptoms, due to the presence of important contiguous neurological and vascular structures.Reference Stankiewicz3 They may also be asymptomatic.Reference Sethi, Lau and Chan4 Common symptoms include ocular manifestations (e.g. visual loss), cranial nerve palsies and headache.Reference Kosling, Hinter, Brandt, Schulz and Bloching1, Reference Sethi, Lau and Chan4
Advances in imaging techniques and the use of endoscopes have assisted the diagnosis of sphenoid sinus mucocele. Plain radiographs and examination with a headlight offer little diagnostic information regarding sphenoid pathology.
The treatment of choice is endoscopic sphenoidotomy and drainage of the mucocele.Reference Kosling, Hinter, Brandt, Schulz and Bloching1, Reference Har-El5, Reference Buckmuhl, Kratzsch, Benda and Draf6
Materials and methods
We undertook a retrospective review of the archives of Singapore General Hospital otolaryngology department, for the period 1999–2006, and identified 10 patients with sphenoid sinus mucocele. Patient demographics, presenting symptoms, investigations and management were evaluated.
Results and analysis
The 10 patients comprised three women and seven men, with a mean age of 54.5 years (range 24–70 years). Patient demographics, past medical history and presenting symptoms are shown in Table I. Three patients had a history of nasopharyngeal carcinoma treated with radiotherapy, two patients had chronic sinusitis and one patient had a history of Rosai–Dorfman disease with a left retro-orbital tumour.
Table I Patients' demographics, past medical history and presenting symptoms

Y = years; F = female; M = male; L = left; NPC = nasopharyngeal carcinoma; RT = radiotherapy; DM = diabetes mellitus; CRT = chemoradiotherapy
Patients presented with ocular symptoms (50 per cent), headaches (30 per cent), nasal discharge (30 per cent) and facial pain (10 per cent). All five patients with ocular symptoms experienced decreased visual acuity, and one patient had an associated visual field defect and proptosis. One patient was asymptomatic, and was detected by routine follow-up computed tomography (CT) scanning for nasopharyngeal cancer.
Examination with a headlight and rigid endoscope revealed no significant nasoendoscopic findings in 50 per cent of the patients. The remaining patients were observed to have varying degrees of nasal polyposis, deviated nasal septum and bilateral inferior turbinate hypertrophy.
Pre-operative imaging was conducted either by CT or/and magnetic resonance imaging (MRI). Of the eight patients undergoing CT scanning, five also underwent MRI scanning for further evaluation. The other two patients received only MRI. Four patients had an isolated sphenoid sinus mucocele, three had extension into the ethmoid sinus, two had extension into the maxillary sinus, and one had a large sphenoid sinus mucocele discharging into the left masticator–parapharyngeal space with compression of the trigeminal nerve. Twenty per cent of patients showed intracranial involvement, while 30 per cent had pan-sinusitis on imaging.
All patients underwent uncomplicated transnasal endoscopic sphenoidotomy and drainage of the mucocele. The ethmoid sinus and maxillary sinus were drained on the same occasion in affected patients. There were no reports of intra-operative injuries to the optic nerve or carotid artery, or of post-operative bleeding. The mean hospitalisation stay was 3.5 days (range 2–8 days), and the mean follow-up period was 29 months (range 4–90 months).
All patients reported an improvement in symptoms post-operatively. Direct nasoendoscopy revealed a patent ostium and clear sphenoid cavity in all patients. Reported improvement in visual acuity was at worst counting fingers pre-operatively to 6/60 post-operatively. Routine post-operative CT or MRI scanning were not conducted. In the four patients who received repeated imaging for follow up of nasopharyngeal carcinoma and left retro-orbital tumour, no recurrence of sphenoid sinus mucocele was reported.
Discussion
Mucoceles are benign, encapsulated lesions filled with mucus and lined by epithelium. They are expansile and locally destructive, with the ability to resorb bone, causing erosions of the bony walls of the sinus. They are commonly found in the frontal and ethmoidal sinuses.Reference Har-El5, Reference Buckmuhl, Kratzsch, Benda and Draf6
Sphenoid sinus mucocele was first identified by Rouge in 1872 and later described by Berg in 1889.Reference Stankiewicz3 To date, only 140 cases have been reported. This entity may present at any age from early adulthood to 70 years, and occurs in men and women with equal preponderance.Reference Stankiewicz3 Sphenoid sinus mucoceles have been mainly described in isolated case reports or within large sinus mucocele series. It is likely that cases are under-reported, as the presenting symptoms are non-specific and physical examination is suboptimal due to the inaccessibility of the sinus.
The aetiology of sphenoid sinus mucocele is still unknown, but three pathogenetic mechanisms have been postulated: submucosal oedema, secretory duct obstruction and ostia obstruction. Submucosal oedema may result from allergic rhinitis, causing ostia narrowing with obstruction; ostia obstruction may also be due to chronic sinusitis, polyposis or both.Reference Stankiewicz3 In the literature, sphenoid sinus mucocele formation has been reported as a possible late complication of radiotherapy to the head and neck.Reference Rejab, Said, Saim and Thim7 Radiation causes scarred mucosa which may occlude the sinus ostium. This apparent aetiological factor was highlighted in our study, as 30 per cent of our patients had a history of nasopharyngeal carcinoma treated by radiotherapy.
The clinical symptoms and signs of sphenoid sinus mucocele are directly related to the sinus anatomy and its contiguous neurological and vascular structures. Proetz described 13 important structures which are contiguous with the sphenoid sinus: cranial nerves II to VI, the cavernous sinus, the carotid artery, the sphenopalatine artery and nerve, the pterygoid canal and nerve, the dura, and the pituitary gland.Reference Stankiewicz3 Patients with sphenoid sinus mucocele become symptomatic when any of these structures are displaced or compressed; the mucocele commonly spreads along the path of least resistance, anteriorly into the nasopharynx or anterolaterally toward the orbit.Reference Yokoyama, Inoue, Imamura, Nagamitsu, Jimi and Katoh8 Sphenoid sinus mucocele is also more likely to present with visual changes compared than with inflammatory disease. Visual loss in sphenoid disease has been attributed to optic neuritis or compression.Reference Sethi9
Hejazi et al. reviewed 130 cases of symptomatic sphenoid sinus mucocele reported up to 2001.Reference Hejazi, Witzmann and Hassler10 Patients' presenting symptoms, in order of decreasing frequency, were: headache (87 per cent), ocular disorders (85 per cent), amaurosis (58 per cent), oculomotor palsies (55 per cent), nasal symptoms (38 per cent), endocrine disorders (four of 130) and panhypopituitarism (one of 130). A similar trend in presentation was seen in our patients, with ocular manifestations (50 per cent) and headache (30 per cent) being the two most common presenting symptoms.
Intracranial extension is unusual in sphenoid sinus mucocele. If extension occurs, it is commonly into the suprasellar region or anterior cranial fossa.Reference Yokoyama, Inoue, Imamura, Nagamitsu, Jimi and Katoh8 Twenty per cent of our patients were observed to have intracranial extension. One patient had extension into the frontal lobe, while another had a large sphenoid sinus mucocele discharging into the parapharyngeal space and into the middle cranial fossa. These cases emphasise the importance of early diagnosis and treatment of sphenoid sinus mucocele, as it is histologically benign but functionally aggressive.
Sphenoid sinus mucoceles represent only 1–2 per cent of all paranasal sinus mucoceles. Of the forty cases of paranasal sinus mucocele operated upon in our department from 1999 to 2006, 10 (25 per cent) involved the sphenoid sinus primarily. The advent of imaging techniques could have contributed to the higher incidence of sphenoid sinus mucoceles seen in our department. In the literature, the incidence of sphenoid sinus mucocele represent 1–2 percent of all paranasal sinus mucoceles. With the statistics from our department, sphenoid sinus mucoceles represented 25% (10/40) of all our paranasal sinus mucoceles, during the period 1999–2006. This higher incidence could be attributed to CT/MRI imaging which were performed for the patients. Computed tomography provides valuable information regarding bony erosion, while MRI enables more precise visualisation of the involvement of the optic nerve, dura, pituitary gland, cavernous sinus and carotid artery.Reference Sethi9 In our study, all patients who presented with ocular symptoms underwent MRI imaging.
Accurate pre-operative imaging is required to define the precise extension and boundaries of the mucocele, and also assists diagnosis. Mucoceles may show various imaging features, depending on their contents. They often have low attenuation on CT (Figure 1), a low signal on T1-weighted MRI and a high signal on T2-weighted MRI (Figure 2), due to their high water content. There is usually no enhancement, or at most marginal enhancement, on CT and T1-weighted MRI, whereas many of the lesions in the differential diagnosis show contrast enhancement. Thus, the diagnosis of mucocele can be suspected pre-operatively and differentiated from craniopharyngioma, pituitary tumour, dermoid, chordoma, epidermoid, aneurysm, metastatic lesions and, in rare cases, an arachnoid cyst.Reference Yokoyama, Inoue, Imamura, Nagamitsu, Jimi and Katoh8, Reference Hejazi, Witzmann and Hassler10 In mucoceles with a high protein content, T1-weighted MRI shows a lesion which is homogeneously hyperintense centrally (Figure 3) with a surrounding rim of hypointense mucosa.Reference Yokoyama, Inoue, Imamura, Nagamitsu, Jimi and Katoh8
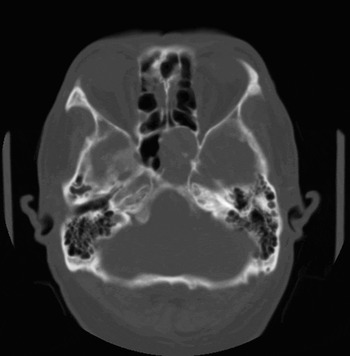
Fig. 1 Axial computed tomography scan of the brain (bone window setting), showing expansion of the left sphenoid sinus and thinning of the bony clivus secondary to bony erosion.
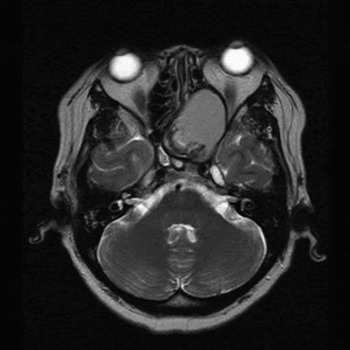
Fig. 2 Axial, T2-weighted magnetic resonance imaging scan, showing a mildly hyperdense left sphenoid sinus with expansion and a mass effect. The T2-weighted signal is lower than expected, indicating the presence of protein within the mucocele. There is extension into the left ethmoid sinus and compression of the left optic nerve.
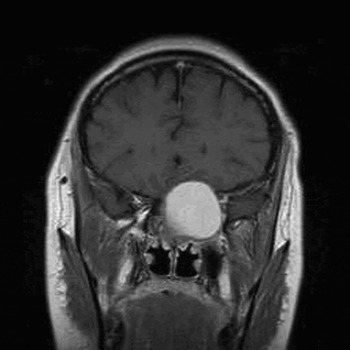
Fig. 3 Coronal, T1-weighted, contrast-enhanced magnetic resonance imaging scan, showing a hyperintense (i.e. high protein content) left sphenoid sinus mucocele expanding into the anterior cranial fossa. Note enhancement of the adjacent dura.
• Sphenoid sinus mucocele is a rare entity
• Although representing only 1–2 per cent of paranasal sinus mucoceles, this lesion has a high prevalence in post-irradiated patients
• Presenting symptoms are non-specific, and patients may be asymptomatic
• Imaging is crucial to diagnosis
• Endoscopic drainage is safe and effective in eradication of disease
The treatment for sphenoid sinus mucocele is surgical drainage, which may be performed either by the transnasal-transphenoidal approach (via endonasal endoscopy or microsurgery) or by craniotomy. The current trend is towards endoscopic drainage. Post-operative complications of transphenoidal decompression are rare, and long term recurrence rates are at or close to 0 per cent.Reference Har-El5 All patients in our study underwent uncomplicated endoscopic sinus sphenoidotomy. They all reported an improvement in symptoms post-operatively, and showed no recurrence.
Conclusion
Sphenoid sinus mucocele is a rare entity. Although uncommon, it has a high prevalence (30 per cent) in post-irradiated patients. Clinicians should have a high index of suspicion of this condition, especially if a patient presents with chronic, non-specific symptoms and/or with visual symptoms. The clinical examination may be normal. Imaging is crucial to diagnosis. Treatment is by endoscopic drainage, which is safe and effective in eradication of disease.






