Introduction
Verrucous carcinoma is an uncommon variant of well differentiated squamous cell carcinoma which was first described by Ackerman in 1948.Reference Ackerman1 It is primarily a disease of caucasian males older than 50 years. Verrucous carcinoma has a predilection for the mucous membranes of the head and neck, and is most commonly found in the oral cavity.Reference McDonald, Crissman and Gluckman2 The second most common site is the larynx, where verrucous carcinoma has been reported only as a glottic or supraglottic lesion.Reference Lee3, Reference Koch, Trask and Hoffman4 Currently, verrucous carcinoma accounts for 1 to 3.4 per cent of all laryngeal carcinomas.Reference Lee3
Although cigarette smoking is highly correlated with laryngeal lesions, it has not been identified as an aetiological or risk factor for verrucous carcinoma of the larynx.Reference Spiro5 Alcohol consumption, however, has been shown to be correlated with this tumour.Reference Oliveira, de Moraes and Filho6
The diagnosis of verrucous carcinoma of the vocal folds is based on the following clinical and histopathological findings: a slow-growing, exophytic, grey, bulky lesion with a papillomatous appearance, which macroscopically comprises a broad-based and locally invasive tumour. Microscopically, the lesion is composed of highly differentiated squamous cells with acanthosis and hyperkeratosis, and large, blunt-ended rete ridges accompanied by an intact basement membrane.Reference Ferlito and Michaels7 An inflammatory reaction consisting of lymphocytes and plasma cells is often present in the stroma. Verrucous carcinoma has a characteristic morphological appearance and specific clinical behaviour, and should be differentiated from other epidermoid carcinomas. Genetic studies have isolated human papillomavirus 16 related DNA sequences from verrucous carcinoma of the larynx.Reference Brandsma, Steinberg, Abramson and Winkler8, Reference Dekmezian, Batsakis and Goepfert9
Treatment strategies for this tumour include surgery, radiotherapy or both.Reference Hagen, Lyons and Haindel10, Reference Burns, Van Nostrand and Bryce11 Surgery has been associated with an 80 per cent local control rate and is usually the preferred first-line treatment modality.Reference Remacle, Eckel and Endoscopic12 The use of radiotherapy is still controversial. Many clinicians do not offer radiotherapy for primary management, because it has been shown in several studies to cause malignant transformation of verrucous carcinoma to undifferentiated carcinoma, and to place patients at risk of regional metastases.Reference Hagen, Lyons and Haindel10, Reference Tharp and Shidnia13–Reference Edstrom, Johansson, Lindstrom and Sandin16 Other authors, however, have failed to find a direct relationship between radiotherapy and malignant transformation of verrucous carcinoma.Reference O'Sullivan, Warde, Keane, Irish, Cummings and Payne17
Surgery procedures can be performed via an open approach, and include laryngofissure, supraglottic laryngectomy, and total laryngectomy for transglottic lesions.Reference Hagen, Lyons and Haindel10 Endoscopic carbon dioxide laser surgery has been found to be an effective alternative to such procedures. This technique was introduced in 1972 by Strong and Jako for the resection of nodules, polyps, cysts, carcinoma in situ and papillomatosis.Reference Strong and Jako18 Its advantages over open surgery include quicker recovery, less morbidity, fewer side effects and greater cost-effectiveness.Reference Casiano, Cooper, Lundy and Chandler19–Reference Shvero, Koren, Stern, Segal, Feinmesser and Hadar22
The European Laryngological Society has classified laser cordectomy into four types: subepithelial (type I), involving resection of the epithelium, and used for carcinoma in situ; subligamental (type II), involving resection of the epithelium, vocal ligament and Reinke's space, and used for tumour (T)1a lesions; transmuscular (type III), involving resection through the vocalis muscle; and total and extended (type IV), which encompasses the contralateral vocal fold and the anterior commissure.Reference Remacle, Eckel and Endoscopic12
To date, most studies of verrucous carcinoma of the larynx have reported treatment with type III or IV cordectomy, or more radical procedures.Reference Damm, Eckel, Schneider and Arnold23–Reference McCaffrey, Witte and Ferguson25 However, although verrucous carcinoma is locally aggressive, it does not invade the basement membrane. Therefore, in our department, type I or II laser cordectomy is routinely used for treatment, without resection of the vocalis muscle, even when the lesion involves the anterior commissure or contralateral vocal fold.
The aim of this study was to evaluate the long-term results of type I and II laser cordectomy for the treatment of verrucous carcinoma of the vocal folds.
Materials and methods
The study group consisted of 18 patients with histopathologically proven verrucous carcinoma of the vocal folds who were treated at the Rabin Medical Center between 1989 and 2006. All patients had undergone videostroboscopy, which detected asymmetrical movement of the vocal folds and a slightly decreased mucosal wave of the involved vocal fold. Diagnosis had been made by direct microlaryngoscopy and biopsy under general anaesthesia, prior to surgery for evaluation of tumour extension or stage. All patients had been classified as having T1 lesions of one or both vocal folds, without subglottic extension or involvement of the anterior commissure and/or arytenoids. Only those who had undergone first-line type I or II microlaryngoscopy with carbon dioxide laser were included. Patients' files were reviewed for clinical and outcome data.
Surgical technique
After induction of general anaesthesia by transoral intubation (using a latex Woodbridge tracheal tube), a rigid laryngoscope (an 18 cm, distending operating laryngoscope; Storz, Weerda, Germany) was introduced through the mouth. Adequate endoscopic visualisation of the larynx was ensured by widening the laryngoscope's spatulas, and by using a 0° Hopkins II endoscope (5 mm diameter, 24 mm length; Storz) to evaluate tumour extension (subglottically and in the sinus Morgagni). All safety precautions were applied. Adrenaline 0.3 cm3 together with saline 9 cm3 was injected laterally to the tumour, between the vocalis muscle and the vocal ligament, in two different sites (anterior and posterior). A carbon dioxide laser beam (SmartXide 8 W system in super-pulse mode with spot size 0.6–0.8 mm2; Deka, Firenze, Italy) coupled via a micromanipulator to a Zeiss microscope (Opmi 6; Zeiss, Thornwood, New York, USA) was used. The lesion was excised en bloc if possible, or piecemeal, with a safe margin of healthy tissue. The completeness of the excision was ensured by inserting and controlling the operating field with the same 0° endoscope.
After tumour excision, intra-operative frozen sections were taken from the excision margins (anteriorly, posteriorly, inferiorly and laterally). The tumour was always removed with an adequate margin of healthy tissue, well visualised through the microscope.
One patient who had initially been seen at another hospital presented with a large glottic mass which necessitated a laryngofissure. In this case, laser cordectomy (type II) was performed through the laryngofissure.
Post-operatively, patients were advised to resume their normal diet on the first day. They were invited for follow-up examination, commencing three weeks after the cordectomy procedure and continuing every month thereafter. After three months, a ‘second-look’ operation was performed to collect multiple biopsy samples, to monitor vocal fold status.
Results
The study group consisted of 14 men and four women, aged 36 to 82 years (mean age 58 years). All patients had T1 lesions. Their clinical data are shown in Table I.
Table I Clinical data for 18 patients with verrucous carcinoma of vocal folds

Pt no = patient number; y = years; completion Rx = completion radiotherapy; F = female; M = male; R = right; L = left; bilat = bilateral; T = tumour
A documented history of smoking was recorded for 15 patients, and of alcohol intake for two; one had a history of voice abuse. There were no data on signs of reflux for any of the patients. The right vocal fold was affected in 12 patients, the left in four and both in two.
Hoarseness was the most prevalent presenting symptom (occurring in all patients). Three patients had dyspnoea, and one patient complained of throat pain.
None of the patients had a neck lesion on presentation.
Follow up ranged from three to 228 months (mean, 48 months). Thirteen patients had no evidence of recurrent disease throughout follow up (Figure 1). The remaining five patients had persistent disease after cordectomy and therefore underwent radiotherapy. Two of these patients had histological evidence of squamous cell carcinoma in addition to verrucous carcinoma of the larynx. The other three had multiple recurrences involving both vocal folds and the anterior commissure. Four of the patients with primary cordectomy failure underwent repeated cordectomy (two required several surgical procedures). In no case was chemotherapy administered as second-line treatment.
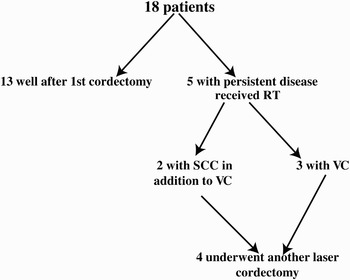
Fig. 1 Long-term outcome of type I and II cordectomy for treatment of verrucous carcinoma (VC) of the vocal folds. RT = radiotherapy; SCC = squamous cell carcinoma
None of the patients suffered any of the reported complications of laser cordectomy, such as dysphagia, aspiration or glottic-supraglottic stenosis.Reference Ellies and Steiner26 Laryngeal oedema developed in one patient and was treated medically with good results.
All patients were alive and well after the minimum follow-up period of three months. No patient died of their disease.
Discussion
The benefits of carbon dioxide laser excision are well known: precise application; minimal tissue damage and surgical trauma; almost bloodless resection; and rapid tissue healing. In cases of laryngeal verrucous carcinoma, this technology has several advantages over standard therapy, including less morbidity, fewer side effects, shorter hospital stay and greater cost-effectiveness. Its disadvantages include problems manoeuvring the endoscope in patients with a short neck or cervical pathology, and the risk that the surgeon will not be able to visualise the anterior commissure and that surgery will therefore not be as radical as it should be (in such cases we suggest piecemeal tumour removal). All our patients underwent a second look operation after three months.
To the best of our knowledge, this report describes the largest series of patients with verrucous carcinoma of the vocal folds treated by type I or II laser cordectomy. Other studies have described more extensive procedures, such as cordectomy beyond the vocalis muscle (i.e. type III or IV), or partial or total laryngectomy.Reference Damm, Eckel, Schneider and Arnold23
• Verrucous carcinoma occurs infrequently in the vocal folds
• This tumour has an excellent prognosis with proper treatment; management strategies include surgery, radiotherapy or both
• This study assessed the use of CO2 laser cordectomy in treating 18 patients with verrucous carcinoma of the vocal folds
• Type I or II laser cordectomy is a safe, feasible and secure method of treating this tumour
• Most recurrent disease can be managed locally with repeated surgery
In type I or II laser cordectomy, the mucosa of the vocal folds is resected, leaving the vocal muscle intact. Therefore, morbidity is lower, the subjective vocal quality is better, and there are fewer complications in terms of local oedema or impaired vocal fold mobility. In our series, the only complication was mild laryngeal oedema, which resolved after local treatment. The majority of our patients (72 per cent) had a good outcome, including satisfactory objective voice quality, and needed no further treatment. Only five patients required adjunctive radiotherapy, to control multiple recurrence of the disease in three patients and concomitant squamous cell carcinoma in two. Four of these five patients underwent repeated laser cordectomy.
Conclusion
Overall, our findings indicate that type I or II laser cordectomy is a feasible and safe procedure for the treatment of selected patients with verrucous carcinoma of the larynx. Prerequisites include a normal neck and the absence of subglottic extension, stridor or extensive lesions. Repeated laser cordectomy is also appropriate in cases of recurrence. We suggest that radiotherapy be reserved for severe cases of multiple recurrence, persistent disease or concomitant squamous cell carcinoma. In patients with a short neck or anterior commissure involvement, we suggest a laryngofissure procedure followed by laser cordectomy. Larger, multicentre studies are needed to confirm these findings and to standardise an appropriate approach to the treatment of laryngeal verrucous carcinoma.




