Introduction
A congenital pre-auricular sinus is a common congenital ear deformity caused by the defective fusion of six hillocks in the first and second branchial arches during the embryonic stage.Reference Kumar Chowdary, Sateesh Chandra and Karthik Madesh1 The sinus is a kind of blind tube that can be ramified and appear tortuous. Its external pit is usually located in the anterior margin of the ascending portion of the helix. A few can be located in the cymba conchae or triangular fossa. Most pre-auricular sinuses are initially asymptomatic, but may develop local redness, swelling, pain, and pus discharge or abscess formation during subsequent infections.
Surgical intervention is the only feasible treatment option; however, traditional simple sinectomy has a high recurrence rate. In 1990, Prasad et al. used the supra-auricular approach for resecting the pre-auricular sinus,Reference Prasad, Grundfast and Milmoe2 which significantly reduced the recurrence rate.Reference Prasad, Grundfast and Milmoe2–Reference Baatenburg de Jong7 In this study, the incision of the supra-aural approach was modified, the extent of surgical resection was defined, and another surgical approach and resection range were proposed for one case of a rare-type of pre-auricular sinus.
Materials and methods
Clinical data
A total of 53 patients (20 male and 33 female) aged 2–72 years (median of 13 years) with congenital pre-auricular sinus, who had been admitted to hospital between January 2014 and December 2018, were selected for this study. All patients had a pre-auricular sinus with infection and underwent simple drainage.
Twenty-four patients had a pre-auricular sinus on the left side and 29 on the right side. The pit was located in the anterior portion of the helix in 51 patients and in the crus of the helix in 2 patients. All patients had different degrees of redness or granulation around the ear. The infection foci were located in the anterior portion of the helix in 41 patients, in the crus of the helix in 12 patients, in the retro-auricular groove in 1 patient, and in the crus and the anterior portion of the helix simultaneously in 1 patient.
All patients underwent incision and drainage of infection foci (31 in other hospitals and 22 in the hospital where the study was conducted) (Table 1).
Table 1. Basic information of patients
*The infection focus in one patient was located in the crus and the anterior portion of the helix simultaneously.
Peri-operative treatment
Treatment included incision and drainage, local daily replacement of the drainage gauze, administration of antibiotics against Gram-positive bacteria through intravenous (IV) drip or orally, and administration of dexamethasone (IV) for 2–5 days in patients with severe oedema.
For patients with infection in the front of the ear (including the anterior portion and the crus of the helix), the drainage incision should be parallel and as close as possible to the anterior margin of the helix so that subsequent surgical incisions can be extended on this basis without the need for additional incisions, which can achieve a better appearance effect. In the present group of 52 patients with infection in the front of the ear, 2 drainage incisions were made far from the anterior margin of the helix so that a small parallel incision could be used to remove the granules around the drainage incision. For those with an infection focus in the retro-auricular groove, an incision was made along the radius of the retro-auricular groove, in the posterior margin of the post-auricular infection focus.
Surgical interventions were performed after 3–10 days of drainage and when local acute congestion had completely subsided. Of all the patients, 25 underwent general anaesthesia and 28 received local infiltration anaesthesia. A mixed solution containing 1 per cent lidocaine with adrenaline 1:100 000 was used as a local anaesthetic.
Incision and dissection
According to the site of infection focus, the pre-auricular sinus can be classified as pre-auricular or post-auricular.
Pre-auricular type
From the upper margin of the retro-auricular groove, the skin was cut along the anterior margin of the helix to the supratragic notch (Figure 1b). According to the position of the scar, granulation or the position of the earlier drainage incision, the incision could be extended to the front of the tragus or a second parallel small incision was made in front of this incision (Figure 2b). The incision was made only to the subcutaneous tissues, and the subcutaneous tissue layer was extensively separated. The front and top boundaries were extended up to the hairline, the back boundary was extended up to the vertical projection line of the posterior wall of the external auditory canal, and the bottom boundary was extended up to the horizontal projection line of the apex of the tragus (Figure 3a). The pre-auricular sinus was cut off beneath the shin of the pit, without any further intervention in the pit on the skin. A large piece of the subcutaneous tissue between the pre-auricular superficial temporal fascia and the auricular perichondrium in this area was completely removed. If necessary, the dissection area was appropriately extended according to the scope of the infection focus.
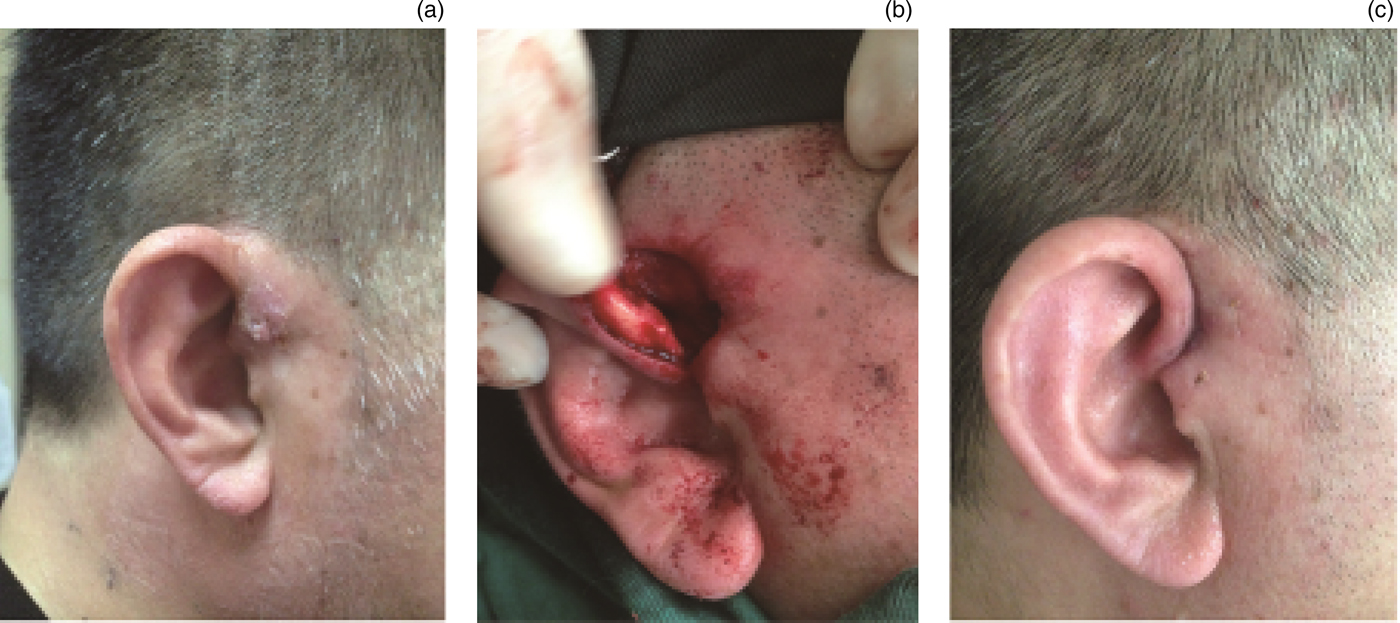
Fig. 1. Infection focus was located in the crus of the helix. The images show views (a) pre-operatively, (b) intra-operatively and (c) one week post-operatively.

Fig. 2. (a) Infection foci were located in the anterior portion and the crus of the helix. (b) A supra-auricular incision was made, and the second incision was made in front of and below the incision.
Fig. 3. Dissection areas for the (a) pre-auricular and (b) and post-auricular types.
Post-auricular type
A post-auricular arc incision was made at the posterior margin of the infection focus, and an elliptical incision was made around the pit in the crus of the helix. The back boundary was extended up to the posterior margin of the infection focus, the bottom boundary was extended up to the horizontal projection line of the inferior wall of the external auditory canal, the top boundary was extended up to the horizontal projection line of the upper margin of the retro-auricular groove, and the front boundary was extended up to the vertical projection line of the pit (Figure 3b). In this area, a large piece of soft tissue between the auricular perichondrium and the mastoid periosteum was removed, together with some of the cartilage along the sinus course.
The incision was sutured with a size 5-0 absorbable suture. A drainage rubber was placed initially and then removed on the 2nd day after the surgery. After 5–7 days of anti-infective therapy, all patients achieved primary intention healing of the incision.
Results
All patients were followed up one week, one month and six months after discharge from hospital, to observe any sign of recurrence, such as infection, a subcutaneous mass and so on. Patient satisfaction regarding the aesthetic result of surgical intervention was also assessed.
All the patients were followed up for six months to five years; no recurrence was found. All patients were fully satisfied with the incision scar concealment and the aesthetic result.
Discussion
Repeated infection of the congenital pre-auricular sinus may require surgical treatment to ensure radical dissection and minimise its impact on appearance as far as possible. The traditional operation (simple sinectomy) involves making an elliptical incision around the skin of the pit, followed by resection along the sinus course. The sinus course is established through pre-operative radiography or methylene blue injection, and probes are used during surgical procedures.
The post-operative recurrence rate is very high (up to 19–40 per cent).Reference Prasad, Grundfast and Milmoe2–Reference Currie, King, Vlantis and Li6 The reasons for the high recurrence rate could be the nature of the sinus, which can be tortuous, narrower and ramified, making it difficult to determine the sinus course adequately using contrast agent or methylene blue dye. Meanwhile, the diffusion of methylene blue during surgical procedures might make it difficult for operators to distinguish the sinus. The probe may not reach the full length of the sinus because of small multi-ramification, leading to the possibility of forming a false course.Reference Leopardi, Chiarella, Conti and Cassandro4,Reference Baatenburg de Jong7
In 1990, Prasad et al. first proposed the supra-auricular approach for resecting a pre-auricular sinus. All the subcutaneous tissues between the pre-auricular superficial temporal fascia and the auricular perichondrium, including the sacs and branches of the sinus, were successfully removed surgically given the good surgical exposition and anatomical markers.Reference Prasad, Grundfast and Milmoe2 In 2001, Lam et al. reported the results of a study comparing the standard conventional technique (simple sinectomy) with the supra-auricular approach (wide local excision) for the surgical management of pre-auricular sinus. They found reported recurrence rates of 32 per cent (n = 25) and 3.7 per cent (n = 27), respectively.Reference Lam, Soo, Wormald and Van Hasselt5
In order to further standardise the range of surgery, reduce the recurrence rate and achieve an optimal aesthetic result, the supra-auricular approach has been modified in the past five years. It is suggested that a congenital pre-auricular sinus should be identified and classified initially; based on its identified nature, specific approaches should then be adopted for the radical dissection of tissues in different areas (regional dissection).
The supra-auricular approach involves making a vertical elliptical incision on the skin around the pit; the incision is then extended upward along the crus of the helix and turned backward. Because the incision is limited by the position of the pit, it may be difficult to achieve better concealment. Moreover, the resection of the skin around the pit may increase the suture tension. Considerable improvements have been made in the radical dissection technique, as follows. The position of the pit is not considered while making the incision. From the upper margin of the retro-auricular groove, the skin is cut along the anterior margin of the helix to the supratragic notch, and the end of the incision is slightly changed according to the position of the scar, granulation or earlier drainage incision. The incision is extended to the front of the tragus, or a second parallel small incision is made in front of this previous incision. The incision is made only to the subcutaneous tissue, and extensive subcutaneous separation is performed. The pre-auricular sinus is cut off beneath the shin of the pit, leaving the pit on the skin as it is. Procedures performed with such incisions have the characteristics of better concealment, minimal skin defects and less suture tension (Figures 1b and 2b).
Following the incision, the pre-auricular soft tissues are separated subcutaneously, the superficial temporal fascia is exposed, and all the subcutaneous tissues between the pre-auricular superficial temporal fascia and the auricular perichondrium are removed. A number of studies have emphasised that, if necessary, part of the tightly adhered cartilage or perichondrium can be removed.Reference Kumar Chowdary, Sateesh Chandra and Karthik Madesh1–Reference Shim, Kim, Kim, Lim and Han8 However, the area of soft tissue resection has not been clearly defined, resulting in non-radical dissection and subsequent recurrence. To further standardise the procedure, it is suggested that the boundary of the removable area (in the front and top) should be extended up to the hairline, the back boundary should be extended up to the vertical projection line of the posterior margin of the external auditory canal, and the bottom boundary should be extended up to the horizontal projection line of the apex of the tragus. If the focus of infection is seen extended further than this area, more resection should be performed to include the infection focus completely. In this study, all 52 patients achieved primary intention healing of the incision (see below for another case), and there were no recurrences.
Most of the previous studies showed that the pit of all reported cases was located in the upper crus or the anterior portion of the helix, and the sac was also located in the front of the ear.Reference Kumar Chowdary, Sateesh Chandra and Karthik Madesh1–Reference Shim, Kim, Kim, Lim and Han8 However, in the present case series, the pit was located in the crus of the helix in only one patient (Figure 4b), and the infection focus was found behind the ear (Figure 4a). A large number of epithelial-like drainage materials were found after post-auricular incision and drainage. The subsequent sinus dissection also confirmed that the sinus penetrated the auricle cartilage to the inner surface of the auricle (Figure 4d). For such a sinus course, the supra-auricular approach and the aforementioned dissection area are naturally inappropriate. Therefore, it is necessary to classify the pre-auricular sinus before surgical correction. The sinus should be defined as pre-auricular or post-auricular type based on whether the sinus penetrates the auricle cartilage up to the craniofacial side. The supra-auricular approach is suitable for the pre-auricular type, while the post-auricular incision should be made for the post-auricular type.
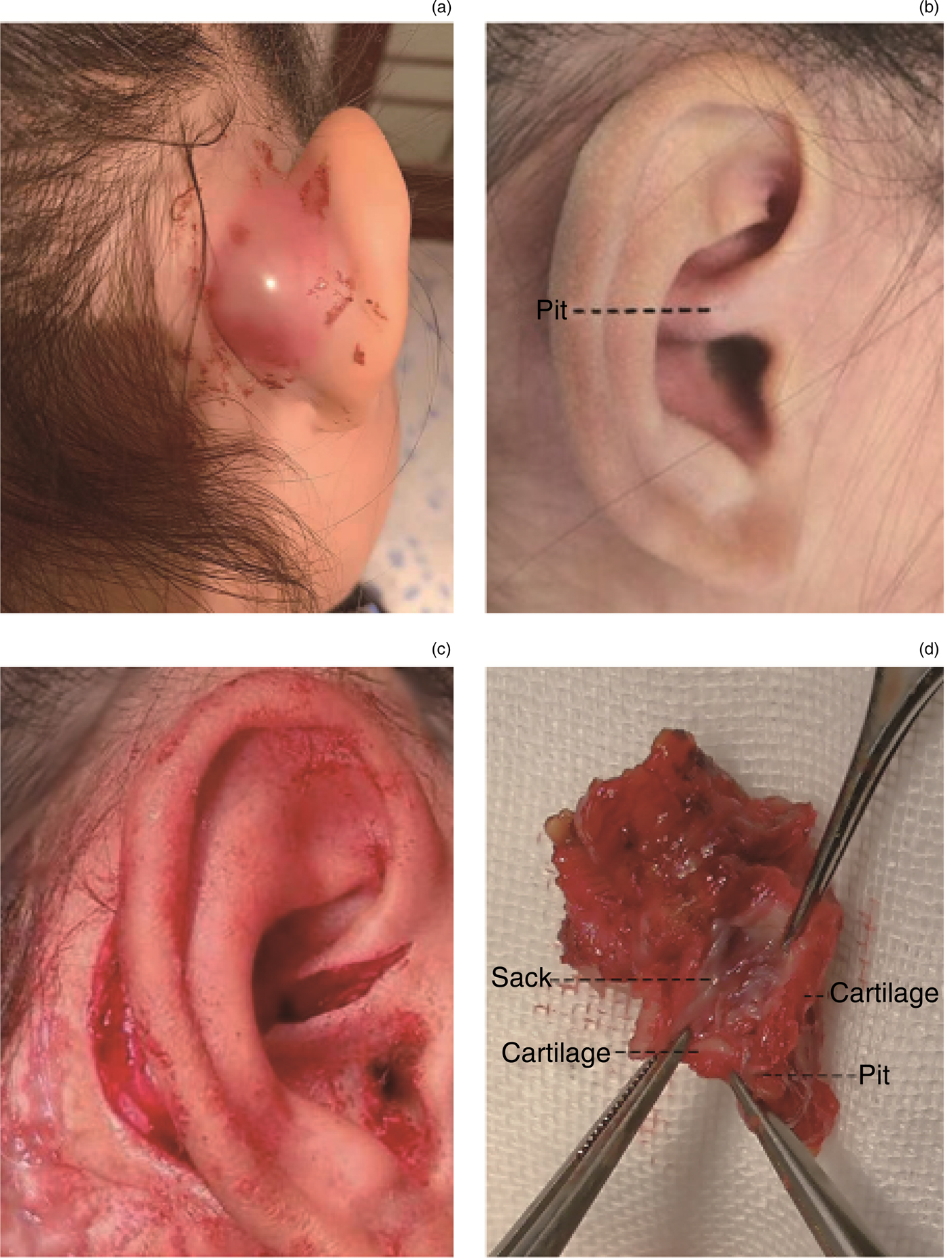
Fig. 4. (a) Post-auricular abscess. (b) Sinus orifice in the crus of the helix. (c) Intra-operative incision. (d) Section view of the sinus, showing the sinus penetrating the auricle cartilage to the craniofacial side.
The incision of cavum conchae was used to manage the pit in the crus of the helix (Figure 4c). Before operating, the dissection area was set. The back boundary was at the posterior margin of the infection focus, the bottom boundary was at the horizontal projection line of the inferior wall of the external auditory canal, the top boundary was at the horizontal projection line of the superior margin of the retro-auricular groove, and the front boundary was at the vertical projection line of the pit. In this area, large pieces of soft tissue between the auricular perichondrium and the mastoid periosteum were completely removed. The management of the pit may require removal of some of the cartilage along the sinus course. If the skin cannot be sutured, it can be directly sutured with the soft tissue of the wound base as long as the cartilage is not exposed.
The present study had no control group, but the results of 53 patients, with no recurrences of infection, are quite convincing, compared with the various surgical outcomes previously reported.Reference Prasad, Grundfast and Milmoe2,Reference Lam, Soo, Wormald and Van Hasselt5,Reference Currie, King, Vlantis and Li6
• Traditional simple sinectomy has a high recurrence rate
• Specific surgical approaches for regional dissection might be adopted based on pre-auricular sinus type
• Further radical dissection might be performed to achieve optimal aesthetic results
In summary, the pre-auricular sinus should be classified as pre-auricular or post-auricular type depending on whether the sinus penetrates the auricle cartilage to the craniofacial side. Surgery should be performed to remove the large pieces of soft tissue within a defined area (regional dissection). The supra-auricular approach is suitable for the pre-auricular type, while the post-auricular incision should be made for the post-auricular type. Simultaneously, another incision of the cavum conchae should be performed, so that satisfactory surgical results with an optimal aesthetic effect can be achieved.
Competing interests
None declared







