Introduction
Sleep nasendoscopy was first described by Croft, Pringle and colleagues in the 1990s as an assessment of the upper airway, performed using a flexible nasendoscope when the patient is in a pharmacologically induced sleep-like state.Reference Croft, Thomson, Samuels and Southall1,Reference Charakorn and Kezirian2
The main indications for performing sleep nasendoscopy in children are: persistent obstructive sleep apnoea (OSA) after adenotonsillectomy, OSA in those with small adenoids and tonsils, conditions with a high risk of multilevel obstruction (e.g. obesity, Trisomy 21, craniofacial abnormalities and neurological impairment), and suspected sleep-induced laryngomalacia.Reference Wilcox, Bergeron, Regunathan and Ishman3
Patients with late-onset or sleep-related laryngomalacia present at an older age with OSA-like symptoms.Reference Lin and Koltai4 Unlike typical laryngomalacia in infants where there are shortened aryepiglottic folds and stridor when awake and asleep, awake flexible nasendoscopy findings are usually normal in these patients, and it is collapsibility of redundant arytenoid mucosa that obstructs the airway.
Although hypertrophied adenoids and tonsils remain the most common cause of obstruction in paediatric OSA patients, there is a 15–20 per cent incidence of multilevel obstruction (i.e. palatal obstruction), tongue base collapse or a posterior epiglottis where obstructive symptoms fail to improve after adenotonsillectomy.Reference Ye, Liu, Zhang, Peng, Yang and Liu5
Sleep nasendoscopy is increasing in popularity as a diagnostic modality in the paediatric population.Reference Wilcox, Bergeron, Regunathan and Ishman3 This preliminary study describes the utility of sleep nasendoscopy compared to microlaryngotracheobronchoscopy in determining the site and level of upper airway obstruction.
Materials and methods
Regarding ethical considerations, this study was registered with the institutional audit department.
This paper describes a retrospective observational study conducted at a tertiary level paediatric hospital that includes patients who underwent sleep nasendoscopy and microlaryngotracheobronchoscopy.
Anaesthesia was induced either via inhalation of 8 per cent sevoflurane in oxygen and air, or intravenous propofol (2 mg/kg). After induction, anaesthesia was maintained via a face mask over the mouth and inspired sevoflurane of between 1 and 2 per cent.
Flexible nasendoscopy was performed by passing a 2.7 mm flexible nasendoscope down to the level of the supraglottis. The following findings were noted to be present or absent: palatal flutter or obstruction, tongue base collapse, oropharyngeal obstruction, retroposed epiglottis, prolapse of redundant arytenoid mucosa and shortened aryepiglottic folds. Manoeuvres such as jaw thrust could be performed to assess their effect upon the airway.
Boluses of propofol (1 mg/kg) were given during nasendoscopy if there was significant patient movement. No topical anaesthesia was applied to the airway. The depth of anaesthesia was therefore light (not surgical anaesthesia), to ensure active movements of the vocal folds and maintenance of some pharyngeal tone. This facilitated a more dynamic assessment of the airway than that provided during microlaryngotracheobronchoscopy where deeper anaesthesia may mask or obscure dynamic airway pathology.
Patients were subsequently fully anaesthetised and microlaryngotracheobronchoscopy was performed.
Statistical analysis was performed using SigmaPlot software, version 12 (Systat Software, San Jose, California, USA). A chi-square test was used to compare the frequency of positive findings for sleep nasendoscopy and microlaryngotracheobronchoscopy. The Fisher exact test was used when over 20 per cent of the expected values in the contingency table were less than 5. A p-value of less than 0.05 was considered statistically significant.
Results
Twenty-seven patients were included in the study. The median age of presentation was 23 months, ranging from 2 months to 10 years.
The most common indication was stridor, with 21 patients (77.7 per cent) presenting with this symptom (Table 1). In nine of these patients, stridor occurred following aryepiglottoplasty, and/or after normal findings on microlaryngotracheobronchoscopy. In six patients, stridor was suggestive of laryngomalacia but with a normal laryngeal appearance on awake flexible nasendoscopy, and/or stridor was associated with an inconclusive history. Three patients were suspected to have atypical or sleep-related laryngomalacia. Another three patients presented with OSA and additional stridor.
Table 1. Indications for sleep nasendoscopy
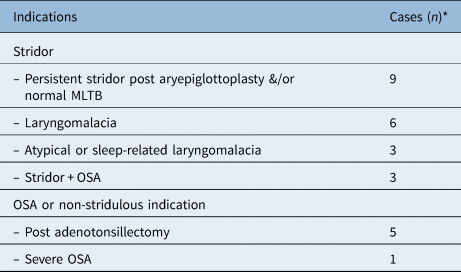
*Total n = 27. MLTB = microlaryngotracheobronchoscopy; OSA = obstructive sleep apnoea
The remaining non-stridulous patients had persistent OSA following adenotonsillectomy (five patients) and severe OSA (one patient). These patients underwent sleep nasendoscopy and microlaryngotracheobronchoscopy keeping in mind the possibility of multilevel obstruction in this cohort.Reference Ye, Liu, Zhang, Peng, Yang and Liu5 Interestingly, among the five patients with persistent OSA following adenotonsillectomy, three patients underwent aryepiglottoplasty for a shortened aryepiglottic fold, retroposed epiglottis and/or indrawing of arytenoids. The remaining two patients were found to have adenoidal regrowth and proceeded with revision adenoidectomy. The patient with severe OSA had large tonsils with oropharyngeal obstruction.
Seven patients were observed to have stridor or stertor during sleep nasendoscopy that had resolved by the time the suspension laryngoscope was placed for microlaryngotracheobronchoscopy (Table 2). Similar observations were noted for palatal and oropharyngeal obstruction, tongue base collapse, and retroposed epiglottis, but these observations were not statistically significant (p > 0.05). Only 47 per cent of patients (8 out of 17) who had prolapse or indrawing of the arytenoids on sleep nasendoscopy had similar findings on microlaryngotracheobronchoscopy. This was statistically significant, with a p-value of 0.017. However, microlaryngotracheobronchoscopy was better for evaluating the aryepiglottic folds: 16 patients were found to have shortened folds on microlaryngotracheobronchoscopy but only 9 (56.2 per cent) had similar findings on sleep nasendoscopy, although this was not statistically significant (p = 0.10).
Table 2. Comparison of sleep nasendoscopy versus MLTB findings

Data represent numbers of cases. MLTB = microlaryngotracheobronchoscopy
Discussion
To our best knowledge, this is the first study comparing sleep nasendoscopy and microlaryngotracheobronchoscopy in the diagnosis of upper airway obstruction in paediatric patients. In the UK, sleep nasendoscopy is not included in the guidelines for upper airway obstruction assessment in the paediatric population.Reference Powell, Watkinson and Clarke6
Our data show that sleep nasendoscopy has the advantage in diagnosing obstruction at the levels of the palate, tongue base, oropharyngeal wall, epiglottis and arytenoids, with statistical significance for the latter. This is because sleep nasendoscopy provides a dynamic representation of obstruction under anaesthesia. During microlaryngotracheobronchoscopy, which utilises a suspension laryngoscope, the tongue base is held forwards as the laryngoscope sits in the vallecula under the hyoid bone, placing the epiglottis in tension. Extension of the neck contributes to stretching of pharyngeal muscles. However, our data also show that shortened aryepiglottic folds are better assessed with microlaryngotracheobronchoscopy, probably because it provides a more detailed assessment with the Hopkin's rod and telescope, and has the added advantage of physical manipulation.
It is common practice during a microlaryngotracheobronchoscopy to lighten anaesthesia in order to dynamically assess vocal fold movement and supraglottic collapse. This is particularly relevant in cases of supraglottic collapse where the level of anaesthesia has to be deepened again in order to undertake aryepiglottoplasty. Moreover, the transition from anaesthesia to an almost awake state can be very rapid, especially in very small children. Sleep nasendoscopy is advantageous in this respect as such changes in anaesthesia levels are unnecessary.
Our anaesthesia technique involved using sevoflurane with or without propofol. In adults, either propofol alone (using a target-controlled infusion technique) or a combination of propofol and midazolam is recommended.Reference Vito, Llatas, Ravesloot, Kotecha, De Vries and Hamans7 Propofol causes muscle relaxation, but midazolam provides more stability and is effective in mimicking natural sleep. Studies have shown that propofol is better at inducing non-rapid eye movement (non-REM) sleep compared to REM sleep. In paediatric patients, the use of sevoflurane for gas induction is the norm, followed by maintenance with dexmedetomidine and ketamine. This combination has been shown to cause less respiratory depression and mimics non-REM sleep.Reference Wilcox, Bergeron, Regunathan and Ishman3
Although the current study was performed by two observers (i.e. senior author and a trainee), we did not account for inter-observer variation. Multiple previous studies, however, have shown satisfactory correlation and agreement between observers, including validation of drug-induced sleep endoscopy with multiple observers.Reference Carrasco-Llatas, Zerpa-Zerpa and Dalmau-Galofre8,Reference Rodriguez-Bruno, Goldberg, McCulloch and Kezirian9 Nevertheless, there is scope to develop a checklist or proforma for sleep nasendoscopy based on this pilot study, to ensure a standardised approach to the procedure (Table 3).
• A retrospective observational study was conducted of 27 upper airway obstruction patients, comparing sleep nasendoscopy with microlaryngotracheobronchoscopy
• Sleep nasendoscopy induced stridor and stertor, and detected obstruction at palate, tongue base, oropharyngeal wall, epiglottis and arytenoid levels
• Microlaryngotracheobronchoscopy was better in diagnosing shortened aryepiglottic folds
• These preliminary data show the utility of sleep nasendoscopy in diagnosing upper airway obstruction
• However, the findings do not negate the role of microlaryngotracheobronchoscopy
Table 3. Proposed proforma for sleep nasendoscopy

N/A = not applicable
Although this is a preliminary study, our data show the advantages of performing sleep nasendoscopy in patients with upper airway obstruction. As it is conducted in the anaesthetic room, provided there is good co-operation with the anaesthetist, sleep nasendoscopy is a simple procedure that only takes a few minutes and does not require advanced surgical skills. Its clinical value, as described above, enables an assessment of the airway in a dynamic but asleep state that is not affected by the anatomical changes which occur as a result of inserting a rigid suspension laryngoscope. This does not negate the role of microlaryngotracheobronchoscopy, which is useful for assessment below the level of the vocal folds and is better for examining the aryepiglottic folds.
Future studies should include a larger cohort. Additionally, further studies should evaluate patient outcome following microlaryngotracheobronchoscopy, with or without prior sleep nasendoscopy, to determine its significance.
Conclusion
Sleep nasendoscopy is not universally supported, as it requires additional resources (i.e. operating theatre space and anaesthetic support), and there is an opinion that anaesthesia does not reproduce a state comparable to natural sleep. Our preliminary data show that there is a discrepancy in the appearance of the upper airway on sleep nasendoscopy versus suspension laryngoscopy and microlaryngotracheobronchoscopy. This demonstrates the utility of sleep nasendoscopy in determining the level and severity of obstruction by mimicking the physiological sleep dynamics of the upper airway.
Competing interests
None declared





