Introduction
The terrorist attacks of September 11, 2001 (9/11) resulted in the destruction of the World Trade Center (WTC) in New York City, the deaths of almost 3,000 individuals, and the exposure of thousands of responders to a complex mix of toxic chemicals and carcinogens (Boffetta et al., Reference Boffetta, Zeig-Owens and Wallenstein2016; Kuan et al., Reference Kuan, Mi and Georgopoulos2019). In addition to hazardous chemical and physical environmental exposures, responders were exposured to serious psychosocial stressors (Platner, Reference Platner2002; Landrigan et al., Reference Landrigan, Lioy and Thurston2004; Perrin et al., Reference Perrin, Digrande and Wheeler2007; Bills et al., Reference Bills, Levy and Sharma2008; Neria et al., Reference Neria, Digrande and Adams2011). These working conditions, including exposure to smoke, fumes, and highly alkaline dust, led to significantly elevated rates of cancer incidence among WTC responders, compared to those not exposed to the toxic cloud that bellowed out from Ground Zero (Zeig-Owens et al., Reference Zeig-Owens, Webber and Hall2011; Li et al., Reference Li, Cone and Kahn2012; Solan et al., Reference Solan, Wallenstein and Shapiro2013; Boffetta et al., Reference Boffetta, Zeig-Owens and Wallenstein2016; Kuan et al., Reference Kuan, Mi and Georgopoulos2019). To date, over 10,000 WTC responders have been diagnosed with cancer (World Trade Center Health Program, 2019), and the WTC Health Program has identified a link between nearly 70 types of cancer and WTC occupational exposure at Ground Zero — including cancers that are rare, aggressive, and difficult to treat (World Trade Center Health Program, 2019).
WTC responders patient population
The New York University School of Medicine, World Trade Center Health Program Clinical Center of Excellence (NYUSoM WTC CCE), one of five, CDC-funded clinical programs, provides treatment and support to responders who may have been affected physically or mentally by their service at the 9/11 disaster sites in New York City, the Pentagon, and the Shanksville, PA, crash site. The General Responder (GR) population includes police officers, employees of the Office of the Medical Examiner, Port Authority, vehicle maintenance workers, and anyone who worked or volunteered on-site in rescue, recovery, demolition, debris cleanup, and related support services. A significant proportion of patients carry a WTC-related mental health diagnosis, the most prevalent being PTSD, followed by other anxiety disorders and unipolar depressive disorders. Although patients diagnosed with an adjustment disorder to WTC-related cancer make up a relatively modest proportion of the GR population, since 2016, the frequency has doubled year after year. Thus, as the expected incidence of cancer in this population continues to increase, the rate of patients diagnosed with an adjustment disorder to WTC-related cancers can be expected to grow as well.
Stigma continues to be one of the most significant barriers to care in the GR community. Stigma can lead to delayed presentation for mental health care and, therefore, increased risk of chronicity of post-trauma psychopathology (Haugen et al., Reference Haugen, McCrillis and Smid2017). Despite large-scale efforts to mitigate the impact of stigma among responders (Crane et al., Reference Crane, Levy-Carrick and Crowley2014), rates of service utilization remain suboptimal (Jayasinghe et al., Reference Jayasinghe, Spielman and Cancellare2005). The occurrence of cancer introduces a medical stressor that may be experienced and perceived by WTC responders as markedly different from the occurrence of mental health problems. In fact, members of the NYU CCE Member Coordinating Committee (NYU CCE MCC) with WTC-certified cancers shared that despite pre-existing WTC-related mental health issues, all members entered mental health treatment only after they were diagnosed with cancer. Thus, among WTC responders, the occurrence of cancer appears to be an important catalyst in breaking down barriers to accessing mental health treatment and addressing symptoms that may have been deleteriously impacting their lives since 9/11. Thus, the availability of an intervention designed to support patients in the context of cancer may provide a unique opportunity to engage these previously resistant or ambivalent WTC responders in mental health treatment.
Meaning-centered psychotherapy background
Meaning-Centered Psychotherapy (MCP; Breitbart et al., Reference Breitbart, Rosenfeld and Gibson2010, Reference Breitbart, Poppito and Rosenfeld2012, Reference Breitbart and Poppito2014a, Reference Breitbart and Poppito2014b, Reference Breitbart, Rosenfeld and Pessin2015) was developed to address the existential issues of suffering, meaning, and purpose, faced by patients diagnosed with advanced cancer. MCP seeks to enhance patients’ sense of meaning by helping them to reflect on, understand, and use the various sources of meaning in their lives as resources for coping in challenging times. In turn, the resulting enhancement in meaning plays a role in improving psychosocial outcomes such as quality of life, psychological distress, and despair (Rosenfeld et al., Reference Rosenfeld, Saracino and Tobias2017). Randomized controlled trials of MCP have demonstrated its efficacy in significantly reducing anxiety, depression, and desire for hastened death, and improving quality of life, meaning, and spiritual well-being among advanced cancer patients (Breitbart et al., Reference Breitbart, Rosenfeld and Gibson2010, Reference Breitbart, Poppito and Rosenfeld2012, Reference Breitbart, Rosenfeld and Pessin2015, Reference Breitbart, Pessin and Rosenfeld2018; Rosenfeld et al., Reference Rosenfeld, Cham and Pessin2018). Furthermore, MCP has been adapted for the treatment of a diverse range of patient populations, including cancer survivors, informal caregivers, bereaved parents, inpatient palliative care and hospice patients, and oncology care providers (Fillion et al., Reference Fillion, Duval and Dumont2009; Applebaum et al., Reference Applebaum, Kulikowski and Breitbart2015; Lichtenthal et al., Reference Lichtenthal, Lacey, Roberts and Breitbart2017; Rosenfeld et al., Reference Rosenfeld, Saracino and Tobias2017; van der Spek et al., Reference van der Spek, Vos and van Uden-Krann2017). Similar to these patient populations, WTC responders are unique due to their membership in the responder culture, their experience of the attacks and aftermath of 9/11, and the subsequent occurrence of cancer in the context of their service. Therefore, while MCP provides an optimal foundation for a meaning-making intervention, it was critical to adapt MCP to meet the specific needs of WTC responders.
MCP for WTC responders
Finding meaning in life after a tragedy, loss, or illness is key to successful adaptation (Park, Reference Park2010). WTC responders diagnosed with WTC-related cancer face a unique crisis in meaning due to their occupational exposures and response to the attacks on 9/11. Generally, members of the GR community experience taxing work demands (Peñalba et al., Reference Peñalba, McGuire and Leite2008) and routine exposure and re-exposure to physical and psychological traumas (McCaslin et al., Reference McCaslin, Rogers and Metzler2006). These exposures place GRs at increased risk for the incidence of new mental health conditions and/or the exacerbation of pre-existing conditions (Marmar et al., Reference Marmar, McCaslin and Metzler2006; Stellman et al., Reference Stellman, Smith and Katz2008; Wang et al., Reference Wang, Inslicht and Metzler2010), as well as at-work productivity loss, early retirement, alcohol abuse, divorce, and increased rates of suicide (Dowling et al., Reference Dowling, Moynihan and Genet2006; O'Hara et al., Reference O'Hara, Violanti and Levenson2013). Research has shown that exposure to prior trauma plays an important role in predicting one's psychological response to the occurrence of cancer (Green et al., Reference Green, Krupnick and Rowland2000; Abbey et al., Reference Abbey, Thompson and Hickish2015; Swartzman et al., Reference Swartzman, Booth and Munro2017). Trauma has the potential to create significant distress by challenging one's global meaning (i.e., deeply held beliefs and goals such as predictability, controllability, and benevolence of others and the world) (Park, Reference Park2010). Thus, WTC responders are tasked with reconciling their pre-existing, fundamental worldviews and their experience of the extraordinary and horrific attacks on 9/11 (Park, Reference Park2010). Furthermore, as WTC responders attempt to reconcile their beliefs and their experience of 9/11, the occurrence of WTC-related cancer can catalyze the recapitulation of the WTC-related trauma, thrusting these patients into an existential crisis of shattered assumptions and the loss of meaning, value, and purpose. Feelings of vulnerability, anger, betrayal, self-blame, guilt, and lowered self-efficacy from previous traumas may be triggered by the occurrence of cancer, resulting in higher rates of psychological distress and increased difficulty making meaning of their illness. These qualities and experiences distinguish WTC responders from the general cancer population, thus justifying the need for a cultural adaptation of MCP designed specifically for these WTC responders.
Therefore, we developed MCP for WTC Responders (MCP-WTC) to address the struggle to make sense of one's life and purpose in the context of the WTC responder's service and subsequent occurrence of cancer. The goal of MCP-WTC is to help these patients to find and sustain a sense of meaning and purpose in life despite their diagnosis. MCP-WTC is a manualized treatment, which organizes sessions around reflection questions that allow important meaning-related content to be systematically uncovered, providing therapists with repeated opportunities to highlight and apply the MCP principles. MCP-WTC fosters meaning-making by helping patients to understand, bring to conscious awareness, and capitalize on the various sources of meaning in their lives, in an effort to find a deeper connection to meaning and to create a coherent narrative of their life.
Adapting MCP for WTC responders
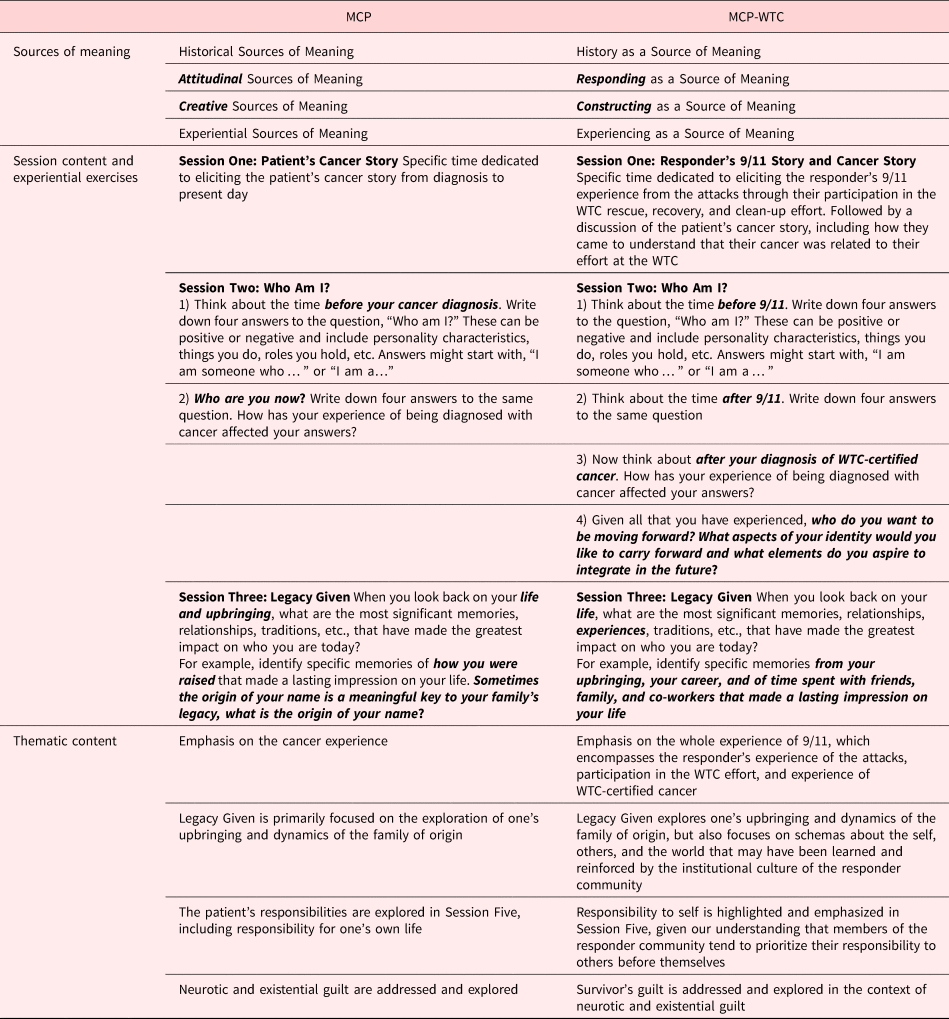
MCP was adapted for the treatment of WTC responders by members of the group that developed and tested MCP for advanced cancer patients and members of the NYUSoM WTC CCE. The authors reviewed the MCP manuals (Breitbart and Poppito, Reference Breitbart and Poppito2014a, Reference Breitbart and Poppito2014b) to identify the aspects of MCP believed to be most salient to the WTC responder population, as well as those that required adaptation. Changes to the MCP manual were made by drawing on the clinical expertise of the mental health professionals at the NYUSoM WTC CCE. The adapted MCP-WTC manuals were developed and distributed to a subgroup of the NYU CCE MCC with WTC-certified cancers for a review. The NYU CCE MCC is comprised of program members, who in partnership with clinical staff, engage in quality improvement initiatives, with the goal of sharing their unique perspective to better serve all NYU CCE members. These members provided their expert opinion on the MCP-WTC session topics, intervention structure, experiential exercises, and language as part of a focus group led by the first author (see Table 1 for thematic content from the focus group). Findings from this focus group were used to further refine the intervention and to finalize the MCP-WTC treatment manual (see Table 2 for key differences between MCP and MCP-WTC).
Table 1. NYU CCE member coordinating committee focus group themes

Table 2. Distinctions between MCP and MCP-WTC

MCP-WTC session content
MCP-WTC begins by orienting the patient to the three primary principles of MCP-WTC: (1) choosing one's response in the face of suffering, (2) sources of meaning, and (3) the ability to construct meaning in our lives. In the introduction to meaning, it is emphasized that meaning can be found in both positive and inspiring moments, as well as those that are horrific, such as 9/11. Patients are then prompted to reflect on the most meaningful events of their lives in order to identify personal sources of meaning. Our patients have shared that this exercise provided them with an opportunity to discuss their role during and after 9/11 and to identify the most meaningful aspects of their service. Throughout this exercise, Nietzsche's (Reference Nietzsche1984) words, “he who has a why to live for can bear with almost any how,” may be particularly salient, as the therapist works to help patients identify and connect to the why's of their service, as a means of coping with the how of their cancer diagnosis.
As the treatment continues, patients engage in a second exercise designed to help construct a coherent and meaningful narrative of their lives. Patients explore the concepts of meaning and identity and are prompted to answer the question, “Who am I?” Given the monumental impact that 9/11 had on WTC responders, MCP-WTC has adapted the original MCP exercise (Breitbart and Poppito, Reference Breitbart and Poppito2014a, Reference Breitbart and Poppito2014b), and prompts patients to think about the most important aspects of their identity before 9/11, following 9/11, and after WTC-certified cancer diagnosis. Finally, due to feedback from the NYU CCE MCC, MCP-WTC includes a future-oriented prompt, which invites patients to reflect on aspects of their identity that they would like to carry forward and elements that they aspire to integrate in the future.
MCP-WTC sources of meaning
History as a source of meaning
History as a source of meaning refers to the concept of legacy, which is presented as having three interconnected components: (1) the Legacy Given, (2) the Living Legacy and, (3) the Legacy that One Will Give (Tables 3 and 4). The Legacy Given refers to the most formative and influential experiences of one's past, those that were given or inherited rather than freely chosen. Elements of one's Legacy Given often include family, geographical and cultural, religious, or spiritual practices that they were exposed to, and the way emotion, illness, and loss were experienced. For WTC responders, critical elements of the Legacy Given may extend beyond family values and include the values of the occupational culture. Such factors common to responder populations include the emphasis on honor, steadiness, emotional suppression, and solidarity with colleagues, often at the expense of social and family relationships (e.g., Woody, Reference Woody2005). Knowledge of these unique cultural components may be critical for understanding how WTC responders experience and make sense of themselves and the world (Lanza et al., Reference Lanza, Roysircar and Rodgers2018). Furthermore, the therapist should listen for experiences of illness and loss in the past, specifically the way in which emotions related to illness and loss were expressed in the responder's family of origin and in the workplace. This may help patients to understand their own illness experience and illuminate the root of their fears or concerns about the future. This exercise also provides the patient and therapist with the opportunity to explore the patient's schemas and the origin of those schemas. The meaning that responders make of the events of 9/11 and the occurrence of cancer are undoubtedly shaped by their previously held cognitive schemas. For example, for a responder who describes instability, insecurity, or abuse in the Legacy Given, the events of 9/11, and subsequent cancer diagnosis may be easily accommodated into existing schemas of the self as unworthy or defective and the world as unsafe and unpredictable, forming the basis for maladaptive meanings to be made. On the other hand, for responders who held positive schemas such as, “I am capable, effective, and in control” and “the world is a safe place,” they must grapple with shattered assumptions about how the world works and their ability to cope. Thus, it is important to uncover schemas that underlie meaning-making as the discussion of one's legacy continues.
Table 3. MCP-WTC sources of meaning

Table 4. MCP-WTC session structure

The Living Legacy refers to the legacy that the responder is currently living and creating. The Living Legacy is presented as dynamic and malleable, impacted not only by the Legacy Given but also by each moment, choice, and action taken. In feedback from WTC responders, we learned that the Living Legacy was one of the most important aspects of the intervention, as it related directly to the responders’ response to 9/11. The Legacy that One Will Give is the final evolution of the responder's legacy and refers to the impact he/she has on others, including how others see the responder, and most importantly, the ways in which the responder sets an example of how to face tragedy. The concept of the Legacy that One Will Give may be a particularly powerful for WTC responders, who have embraced and honored the slogan, “never forget.” In order to generate a moral of one's life story, it is necessary to integrate the pieces of the Legacy Given, the Living Legacy, and ultimately the Legacy that One Will Give. By virtue of this exercise, patients begin to view their service, their response to 9/11, their cancer diagnosis, and their lives as a cohesive narrative complete with lessons to be shared and powerful experiences to be witnessed.
Responding as a source of meaning
An important principle of MCP-WTC is rooted in Frankl's words, “the last vestige of human freedom is the ability to choose our attitude in the face of suffering” (Reference Frankl1963/1984). Based on the experience of the authors and feedback from the NYU CCE MCC, MCP-WTC has adopted “Responding as a Source of Meaning,” instead of “Attitudinal Sources of Meaning,” used in MCP. September 11th was a tragic reminder that we often do not have control of the events, losses, and storms of life. However, despite the darkness of pain, grief, and suffering, human beings never cease to have the ability to choose their response to suffering. Furthermore, the ability to choose one's response to the circumstances beyond his/her control can be a source of meaning in and of itself, and perhaps a way to transcend limitations.
MCP-WTC introduces mortality as the ultimate limitation of life. The experience of being diagnosed with cancer often catalyzes a confrontation with the unsettling reality of death. The finiteness of life is introduced using a metaphor of a sculptor, hammering away at a piece of unshaped stone, understanding that there is a deadline to complete the masterpiece, but unaware of when that deadline will strike. WTC responders are the sculptors, working to create a life that is meaningful, one that has value and purpose, unsure as to when that life will end. Although difficult to accept, the meaning of life is derived from its finiteness, it challenges us to make the most of today, which includes choosing how we respond to the most challenging limitations. In MCP-WTC, responders reflect on the obstacles, challenges, and limitations they experienced in the past and how they dealt with them at the time. The role of the therapist is to highlight the choices that the patient made in the past to respond to or choose his/her attitude in the face of suffering. This is particularly important when working with traditional first responders, who may believe, “I had no choice, I was just doing my job.” MCP-WTC helps patients recognize how they came to be a responder, and specifically how and to what extent they engaged in this role. Ultimately, patients are able to take ownership of the ways in which they responded to limitations in the past, identify opportunities to choose their response in the present, and recognize responding as a source of meaning and strength which can foster the development of new skills, clarified values, and resilience.
Constructing as a source of meaning
Previously referred to as “Creative Sources of Meaning” in MCP, MCP-WTC uses the word “constructing” to represent the construction of the Freedom Tower after 9/11 and MCP-WTC's focus on the reconstruction of meaning. “Constructing as a Source of Meaning” refers to the important existential concepts of creativity, courage, and responsibility. Our responsibility as human beings is to live life to its fullest potential, to construct a life of meaning, identity, direction, growth, connection, purpose, and fulfillment. Again, we construct our lives, from a piece of unshaped stone to a life of richness, fulfillment, and meaning. This source of meaning underscores the empowering understanding that every moment of life provides an opportunity to rebuild, to forge new paths, to traverse uncharted territories, and to push limits. The challenge, however, is that constructing a meaningful life requires both courage and commitment. The concepts of commitment and responsibility often resonate powerfully among GRs who respect and honor values such as commitment, loyalty, and duty. The ability to help our patients identify and take ownership of how hard it has been to make the choices they have made empowers them to continue to build and rebuild. With this in mind, we invite responders to consider what unfinished business exists in their lives and why. For some, unfinished business includes returning to the WTC site, memorial, or museum, while for others, it may be related to personal and professional ambitions, travel, broken relationships, and plans for retirement and the future. Patients are encouraged to consider taking responsibility for the unfinished aspects of life by creating a “Legacy Project.”
Experiencing as a source of meaning
Experiencing as a source of meaning refers to one's ability to remain mindfully open to the meaningful experiences of life. Patients are reminded that meaning can be found in both the most powerful and the most seemingly mundane of moments. The experiences of love, beauty, and humor have the ability to capture our attention and take us to a place where we experience awe and admiration. Hence, experiencing life in this way can help us feel as though we are a part of something greater than ourselves and connected in a way that feels powerful and important. Rather than conceptualized as everyday occurrences, such experiences of love, beauty, and humor are conceptualized as important sources of meaning in the patient's life that remain accessible despite the limitations of illness. For WTC responders, experiences of humor and laughter are often regarded as the most important sources of meaning and critical to coping with tragedies experienced over the course of their careers. Helping these patients to recognize that making a joke or sharing a laugh, even with a stranger, is more than a pleasant moment, but a critical and powerful source of meaning in their lives is an important task for the MCP-WTC therapist. In our experience, when patients are introduced to this source of meaning, they may soon find that meaning is truly all around them.
Discussion
To date, over 10,000 WTC responders have been diagnosed with cancer, and nearly 650 have died of the disease (CDC, 2019). In fact, in 2019, the number of deaths from WTC-related illnesses surpassed the number of deaths from the attacks on 9/11 themselves (CDC, 2019). Despite the growing incidences of cancer in the WTC responder population, to date, to the best of our knowledge, no specific interventions have been adapted or developed that focus on improving the quality of life of these responders at any point on the cancer trajectory. Prior adaptation of MCP-WTC, the empirical literature regarding the treatment of mental health conditions in WTC responders focused almost entirely on the treatment of PTSD (e.g., Difede et al., Reference Difede, Malta and Best2007; Litz et al., Reference Litz, Engel and Bryant2007; Haugen et al., Reference Haugen, Werth and Foster2016; Gonzalez et al., Reference Gonzalez, Mackin and Mahaffey2018). However, even in trauma-focused psychotherapies for PTSD, meaning-making is considered a vital active ingredient of change (Schnyder et al., Reference Schnyder, Ehlers and Elbert2015). In the context of trauma treatment, meaning-making is associated with changing problematic appraisals of the trauma about the self and the world, which, in turn, mediates a reduction in PTSD. The fact that meaning-making has been a critical component of existing treatment approaches for WTC responders underscores the potential utility of this approach in treating WTC responders with WTC-related cancers.
MCP-WTC is a novel, cultural adaptation of MCP, designed to target existential distress and help responders find and sustain meaning in life despite the limitations of their illness. In our work adapting and delivering MCP-WTC, we have identified several critical themes of the WTC responder's cancer experience and how those can be addressed by the principles of MCP-WTC. Through the exploration of the existential topics most relevant to the experiences of WTC responders with cancer, MCP-WTC provides patients with the tools to process difficult emotions, to construct a life of meaning, and to connect with sources of meaning in order to navigate life after 9/11 and cancer.
MCP-WTC is conceptualized as a transdiagnostic and strengths-based intervention, most well-suited for those patients diagnosed with an adjustment disorder to cancer. Hence, specific psychiatric diagnoses are not addressed directly, but symptoms of these disorders are conceptualized to result from the patient's disconnection from sources of meaning. By virtue of helping patients to identify, connect to, and perhaps reconnect to the most important sources of meaning in their lives, the impact of depression and anxiety can be mitigated. Furthermore, the MCP-WTC principle of choosing one's response to challenges provides patients with a new skill that can be utilized to respond to the symptoms of depression and anxiety, while constructing a richer and more meaningful existence.
Conclusions and future directions
MCP-WTC is currently being delivered at the NYUSoM WTC CCE to WTC responders with WTC-related cancers. Given the efficacy of MCP in improving the quality of life among groups of patients with advanced cancer (Breitbart et al., Reference Breitbart, Rosenfeld and Gibson2010, Reference Breitbart, Rosenfeld and Pessin2015), we have formed groups of patients at similar stages of the cancer experience (i.e., survivorship, advanced disease) to foster group cohesion and address the needs of our patients at all stages of illness. Furthermore, while the prevalence of cancer in this population of WTC responders is wide-spread and growing, WTC responders face many chronic conditions, including rhinosinusitis, gastroesophageal reflux disease (GERD), asthma, chronic obstructive pulmonary disease, and respiratory disease. Thus, MCP-WTC is being further developed to address the limitations presented by the chronic medical conditions faced by this population. WTC responders helped to unite and inspire the nation in the aftermath of one of the most horrific tragedies in American history. However, despite growing incidents of WTC-related illness and the increasing need for care, MCP-WTC is the first cultural adaptation of an existing treatment designed to improve the quality of life of medically ill WTC responders with cancer. Our hope is that MCP-WTC proves to be an adaptation, well-suited to help WTC responders find and sustain meaning in life in the wake of the tragedy of 9/11, their experience responding to 9/11, and their subsequent encounter with cancer.
Acknowledgments
We acknowledge the contributions of all collaborators at the New York University School of Medicine World Trade Center Health Program Clinical Center of Excellence (NYU WTCHP), Memorial Sloan Kettering Cancer Center (MSKCC), and the Mount Sinai World Trade Center Health Program Clinical Center of Excellence (Mt. Sinai WTCHP). We acknowledge the efforts of the Mt. Sinai WTCHP to organize and participate in clinician focus groups critical to the conceptualizations leading to this paper. We would also like to recognize the contributions of MSKCC staff who assisted with facilitation of the MCP training and the Mt. Sinai WTCHP clinician focus groups, Katherine Lynch, Stephanie Benvengo, Sally Reisch, Natalie Cereseto, and Ashley Tigershtrom; as well as all of the Mt. Sinai WTCHP providers who participated and generously shared their feedback. Finally, we would like to acknowledge the ongoing clinical contributions of Mt. Sinai WTCHP providers Giselle Martinez, LCSW and Aleksandra Rayska, Ph.D. Ongoing support for efforts for Meaning-Centered Psychotherapy training and research at MSKCC have been provided by NIH (R25 CA190169, PI: Breitbart; T32 CA00946, PI: Ostroff; CA008748, PI: Thompson). Finally, and most importantly, we wish to express our deepest appreciation for the World Trade Center responders, who we have the privilege of working with and learning from. Without the insights of these responders and their participation, this work would not be possible.
Disclosures
The contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control.