Aneurysms of the aortic arch are rare. Medical follow-up is associated with poor prognosis, besides surgical treatment is still associated with serious mortality and morbidity.Reference Kawatou, Minakata and Sakamoto1 Operations may require cardiac arrest, hypothermia, and total circulatory arrest in order to achieve a comfortable, bloodless field. Not only the cerebral protection has utmost importance but also the myocardial and visceral protection are crucial for an uneventful post-operative course and survival.
In this report, we present our surgical technique providing isothermic, beating heart aortic arch replacement with complete body perfusion.
Case report
The technique was used for the treatment of five patients with various congenital cardiac disorders combined with the pathologies of the aortic arch. The features of the patients are presented in Table 1. In this report, we present an 18-month-old boy (case 3 in the table) who underwent Type A aortic interruption repair in the newborn period with a pericardial roll which was interposed between the ascending aorta and the descending aorta. He presented to the clinic with aortic arch aneurysm sizing 3.8 cm in diameter diagnosed with echocardiography. There was an additional insignificant apical muscular ventricular septal defect. Pathology was confirmed with computerised tomography and it revealed a dilated pericardial roll (4 cm in diameter) with stenosis at the anastomosis site of the pericardial roll with the ascending aorta (Fig 1a and b). The ascending and descending aorta calibers were normal. The pathology was explained to the family of the patient in details, and following their consent, we decided to repair the pathology surgically.
Table 1. Features of the patients


Figure 1. (a) Pericardial roll aneurysm detected by computerised tomography (3D reconstruction). (b) Pericardial roll aneurysm detected by computerised tomography (axial view).
Surgical technique
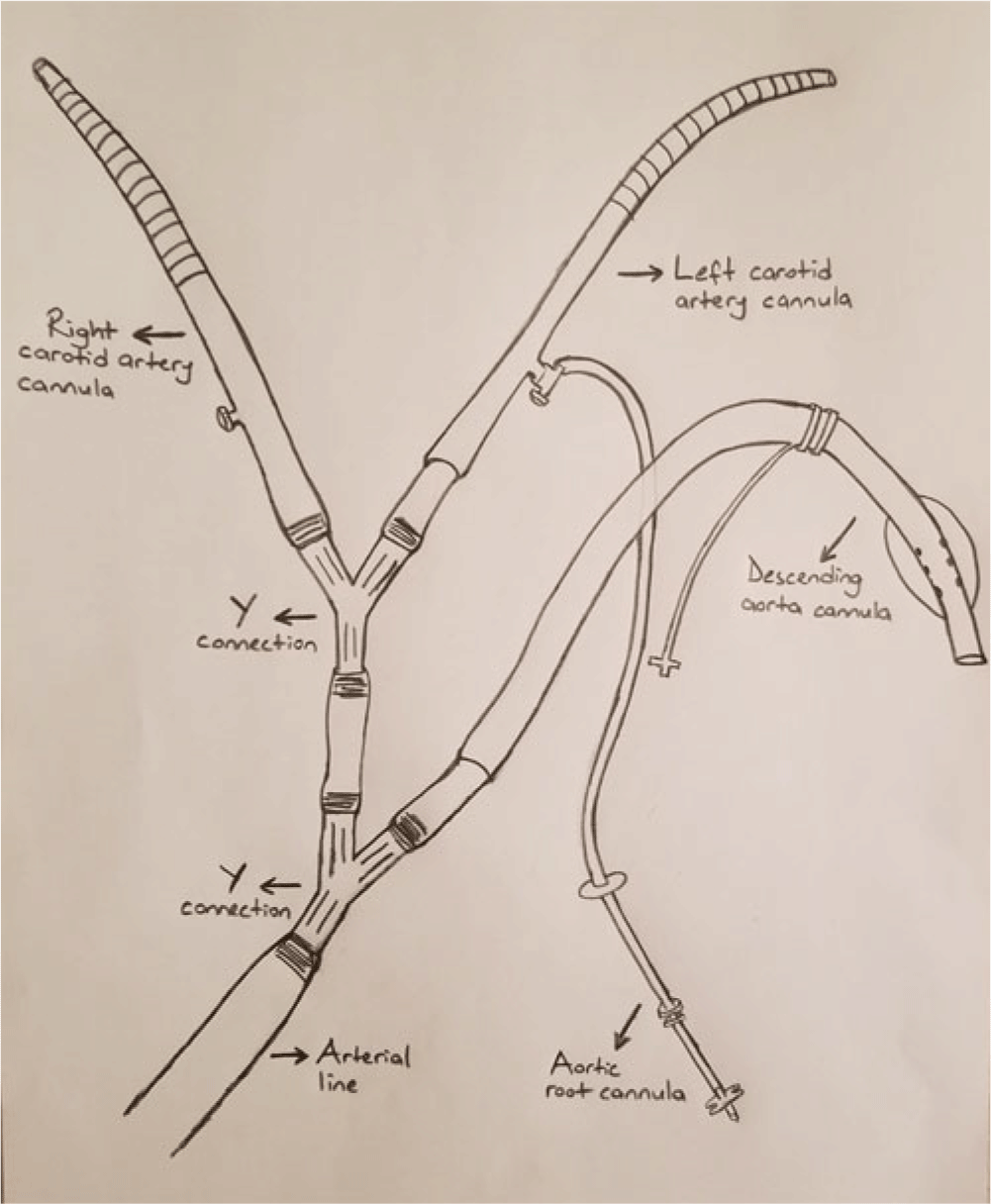
Anesthesia protocol included jugular venous catheterization for central venous line and right radial and femoral catheterization for invasive arterial pressure monitoring. Near-infrared spectroscopy probes were attached to the forehead and leg to evaluate the adequacy of the cardiopulmonary bypass flow. A quadruple cannulation system was prepared, connected to the arterial line of the cardiopulmonary bypass (Fig 2, Fig 3a and b), and de-aired carefully. The cannulas were for bilateral carotid arteries, descending aorta, and the proximal ascending aorta which was for the coronary perfusion during aortic clamp. The size of the main perfusion cannula, for example, the aortic cannula, which will be deployed into the right carotid artery during selective perfusion of the right side of the brain was adjusted according to the body surface area of the particular patient and the manufacturers’ (Medtronic Inc., Minneapolis, Minnesota, United States of America) recommendations depending on the flow guidelines for each cannula size. Left carotid artery cannula was chosen depending on the diameter of the vessel. A balloon tip descending aortic cannula, an adult size retrograde cardioplegia cannula, was preferred for the perfusion of the lower body parts. An appropriate size pediatric antegrade cardioplegia cannula was preferred to perfuse the coronary arteries during aortic clamp. Appropriate sizes of Medtronic DLP (Medtronic Inc., Minneapolis, Minnesota, United States of America) cannulas were used during the surgical procedures. Except the venous and central aortic cannulas, the sizes of the remaining cannulas were approximately chosen depending on the size of the corresponding artery. The aortic root cannula was connected to the left carotid artery cannula. Connections of cannula were performed with an aim to provide optimal flow distribution to perfuse each system adequately.

Figure 2. Schematic drawing of the quadruple cannulation system.

Figure 3. (a) The quadruple cannulation system. (b) Deployment of the cannulas into the right and left carotid arteries, proximal ascending aorta and the descending aorta.
Following re-do median sternotomy ascending aorta, brachiocephalic trunk, left carotid and left subclavian arteries, pericardial roll, and the descending aorta were prepared. Cardiopulmonary bypass was initiated with ascending aortic and right atrial cannulations. Heart was emptied for a comfortable operating field. Descending aorta was cannulated distally through a purse string suture. After the insertion of the aortic root cannula, ascending aorta was cross-clamped proximally beyond the root cannula. The ascending aorta cannula was advanced into the right carotid artery and the descending aorta and the left subclavian artery were clamped. Left lateral side of the ascending aorta, anastomosis region of the ascending aorta-pericardial roll and the dilated pericardial roll itself were opened. The remaining cannula was deployed into the left carotid artery with open technique. The ascending aorta was enlarged with a xenograft pericardial patch (Edwards Lifesciences, Irvine, California, United States of America). The anterior portion of the dilated pericardial roll was resected leaving the posterior wall in place and aortic arch was reconstructed with a xenograft pericardial patch. Before the completion of the anastomosis, the left carotid artery cannula was removed. After de-aeration, the clamps were released and right carotid cannula was drawn back into the ascending aorta and the aortic root cannula was removed. Patient was de-cannulated when the optimal hemodynamics were achieved and operation was ended with standard measures.
The operation was performed with normothermic conditions. Heart rhythm abnormalities did not occur and NIRS values did not decrease significantly throughout the procedure indicating adequate perfusion of whole body. Total cardiopulmonary bypass time and operation time were 72 minutes and 228 minutes, respectively.
At the end of the operation, the flows from each cannula which were selected according to the body surface area of this patient were measured ex vivo and recorded (Coronary perfusion 35 cc, descending aorta 95 cc, left carotid artery 108 cc, right carotid artery 240 cc, accordingly; Table 2). The patient was extubated 2 hours after the operation without any neurologic deficit. Abnormalities in renal or liver functions did not occur and troponin levels did not increase significantly in the post-operative blood analysis. Intensive care unit stay was 1 day and he was discharged from the hospital on the 4th post-operative day. He has been followed active and event free for more than 6 months.
Table 2. Ex vivo flow measurements*

* The measurements were obtained from the cardiopulmonary bypass circuit when the flow was adjusted at a rate of 2.4 L/minute/m2, which was 1032 ml for the particular patient (Length: 78 cm, weight: 9200 g, body surface areas: 0.43 m2)
Discussion
Aneurysms comprising the aortic arch are challenging pathologies despite advances in surgical and interventional techniques. Conventional surgical reconstruction is the gold standard method of treatment in the current era of endovascular therapeutics. Surgery usually requires aortic cross-clamping, cardiac arrest and even deep hypothermia for a bloodless comfortable field for the critically important anastomosis of the arch vessel and the distal aorta.Reference Matsuura, Tsutsumi and Monta2 Meanwhile cerebral protection has utmost importance during the procedure and various attempts including total circulatory arrest, antegrade, or retrograde cerebral perfusion methods have been defined and well-studied in the literature.Reference Nardi and Avrahami3
Advantages of continuous cerebral perfusion over hypothermic deep circulatory arrest have been shown in the literature. Although retrograde cerebral perfusion is one of the methods for this aim, it has nearly been abandoned and has only historical evidence.Reference Uchino, Yunoki, Sakoda, Saiki, Hisamochi and Yoshida4,Reference Kanda, Kunisawa and Iida5 Cerebral flow through carotid arteries is the most physiological perfusion method; however, perfusion through femoral cannulation may be required when it is inevitable due to the conditions of the carotid or axillary arteries; however, still it is not ideal.Reference Kanda, Kunisawa and Iida5 Cerebral flow provided by single vessel blood supply may be adequate in most instances. Better outcomes have been obtained in patients when bilateral carotid arteries and even axillary arteriesReference Kasama, Uchida, Karube, Takebayashi, Imoto and Masuda6 are perfused. Moreover, there are case series in the literatureReference Fernandes, Walsh, Walsh, O’Neil, Gelinas and Chu7 providing excellent results with short intensive care unit and hospital stays and low visceral dysfunction rates with total body perfusion using double oxygenator systems. We added myocardial perfusion to bilateral carotid and antegrade distal aortic perfusion with a coronary perfusion cannula and performed the operation with normothermic conditions, uneventfully utilizing the various advantages of normothermia and whole body perfusion.
There are certain limitations of our study. The number of the patients who underwent arch replacement with this technique is small. Although one case was presented here, five patients underwent surgical treatment utilizing the same measures. The long-term results of these patients will be documented in the future when the follow-up duration and cohort size are increased. However, so far all the children are alive, active, free of symptoms, and devoid of any neurologic or growth retardation. Second limitation is the use of the method only in the pediatric population with various congenital cardiovascular pathologies including the aortic arch. Hence, we lack experience on adult patient population as it is very seldom to see non-dilated proximal ascending aorta and pathology solely confined to the distal ascending aorta, aortic arch, and proximal descending aorta. However, our promising results with pediatric cases may propose the technique for adult patients with aforementioned aortic pathologies. Another limitation may be regarded to the configuration of the cannulas and their connections with each other. We aimed to perfuse the upper and lower parts of the body separately by dividing the central line of the cardiopulmonary bypass circuit into two in order to perfuse upper and the lower parts of the body. The cerebral line of the circuit was further divided into two for the individual perfusion of the right and left carotid systems. An additional line was connected to the left carotid artery cannula for coronary perfusion. Cannula configurations were adjusted accordingly so that perfusion of the main trunks would not be interrupted even during negligible clamping periods for insertion or removal of the cannulas. Various other configurations may be applied; however, our aforementioned configuration has been adequate in all our cases so far.
In conclusion, in this report, we present our surgical technique providing normothermic ascending aorta, aortic arch, and proximal descending aorta replacement with selective cannulation of the whole body. Our preliminary results with limited cohort size children showed promising early and midterm follow-up results. Multi-center high-volume studies including adult patient population are warranted in order to establish a more strict cannulation and surgical protocol in this particular patient population.
Acknowledgements
Multi-cannulation system patent application has been made and transactions are being processed.
Conflicts of interest
None.