INTRODUCTION
As in other developed nations, the number of patients with cancer in Japan continues to increase with every year. One of every two people will be affected by cancer, it being the cause of death for one in every three (Ministry of Health, Labour, and Welfare, 2014). In 2008, the number of newly diagnosed patients with cancer in Japan was approximately 750,000, 153,000 (20.4%) of which were aged between 20 and 59 years, and thus likely to have minors living at home (Foundation for the Promotion of Cancer Research, 2013). The most prevalent cancer among women was breast cancer, which is rising in the 30–59 age bracket. The parent diagnosed with cancer and spouse experience personal stress and anxiety related to the illness and disruption of their normal roles, as well as the functioning of the entire family. Patients with cancer are faced not only with the real-life problem of managing a household during their illness but also with the issue of how to tell their children about the cancer and address the psychological impact of their cancer on their children (Barnes et al., Reference Barnes, Kroll and Burke2000; Semple & McCance, Reference Semple and McCance2010).
Many researchers have conducted descriptive studies on school-aged and adolescent children living with a parent who has cancer. These studies examined the emotional and behavioral problems and the psychological functioning of children following a mother's cancer diagnosis (Hoke, Reference Hoke2001; Thastum et al., Reference Thastum, Watson and Kienbacher2009; Visser et al., Reference Visser, Huizinga and Hoekstra2005; Watson et al., Reference Watson, St. James-Roberts and Ashley2006). According to a review by Osborn (Reference Osborn2007), no clear correlation was noted between the psychological functioning of children and most medical parameters related to mothers with cancer, such as the time elapsed since the diagnosis and the treatment regimen. As for school-aged children, boys showed more emotional problems following a parent being diagnosed with cancer (Visser et al., Reference Visser, Huizinga and Hoekstra2005), and boys of mothers with breast cancer were more socially sensitive and isolated than their comparable peers (Vannatta et al., Reference Vannatta, Grollman and Noll2008).
Cancer may cause posttraumatic stress symptoms in both patients and children. Foran-Tuller et al. (Reference Foran-Tuller, O'Hea and Moon2012) examined the impact of a mother's breast cancer diagnosis on her child's internal, external, and posttraumatic stress symptoms, based on maternal reports. They found that mothers with cancer perceived their children to have more symptoms of PTSD than the mothers without cancer, and they emphasized the importance of assessing PTSD in children whose mothers have cancer (Foran-Tuller et al., Reference Foran-Tuller, O'Hea and Moon2012). Furthermore, using a Japanese sample, Ozawa (Reference Ozawa2014) surveyed 138 children and found that 31% of those aged 6–14 years and 21% of adolescents aged 15–18 years reported having posttraumatic stress symptoms related to their parent's cancer.
Several interventional programs for children whose parents had cancer have been developed and evaluated but have not been empirically substantiated through research (Su & Ryan-Wenger, Reference Su and Ryan-Wenger2007). Niemela and colleagues (Reference Niemela, Hakko and Rasanen2010) examined five such studies and showed that only one program targeted both children and parents (Greening, Reference Greening1992). Family-centered interventions have been researched, most of them involving children and parents, but these did not offer peer group support, a critically important approach for school-aged children (Thastum et al., Reference Thastum, Munch-Hansen and Wiell2006; Schmitt et al., Reference Schmitt, Manninen and Santalahti2007; Romer et al., Reference Romer, Saha and Haagen2007; John et al., Reference John, Becker and Mattejat2013; Davey et al., Reference Davey, Kissi and Lynch2013). For example, Lewis and coworkers (Reference Lewis, Casey and Brandt2006) created the Enhancing Connections Program for mothers diagnosed with breast cancer to promote family adjustment and parenting. They tested the efficacy of this intervention in a randomized controlled trial and found that the program improved mothers' and children's depressed mood, mothers' parenting skills, and children's behavioral emotional adjustment by intervening with the mother only (Lewis et al., Reference Lewis, Brandt and Cochrane2015).
Based on past studies, there is a paucity of research that documents the impact of peer group interventions for children whose parents have cancer while concurrently examining parental outcomes. The purpose of our exploratory pilot study conducted in Japan was to examine the feasibility of a group intervention for children and their parents with cancer, and the impact on the child's stress and the parent's quality of life (QoL) and psychosocial distress. The Japanese version of the CLIMB® Program, to be described below, is a group program that was designed for school-aged children whose parents have cancer. The specific aims of the current study were to: (1) examine the feasibility and acceptability of the Japanese version of the CLIMB® group intervention, and (2) evaluate the outcome of a program involving both children and their parents with cancer. To our knowledge, our study represents the first time that a group intervention for children and parents with cancer was conducted in Japan. It is therefore important to provide preliminary pilot data for future interventional research. This is especially critical for children in Japan who are faced with parental cancer, as many more Japanese families are impacted than families in other highly developed countries.
METHODS
Intervention Description
The group intervention, called the CLIMB® Program, an acronym for Children's Lives Include Moments of Bravery, was developed in the United States for use with school-aged children of patients with cancer (van Dernoot, Reference van Dernoot2015). Japanese psychosocial oncology professionals attended a two-day training workshop in the United States and offered additional CLIMB® training in Japan in cooperation with the Hope Tree.
The program follows a standard training manual modified from the U.S. manual (Heiney et al., Reference Heiney, Heiney and Peterson2006). The original English-language manual was translated into Japanese. In consultation with child-life specialists, we changed terms and concrete examples to ones that better reflect Japanese culture and school life. An overview of the Japanese version of the CLIMB® Program is described below (also see Kobayashi, Reference Kobayashi2014; Osawa, Reference Osawa2014). The children's program is grounded in the principles of mental health promotion. The goals of the program are to improve a child's ability to cope with a parent's cancer and to reduce the stress related to their parent's cancer. The program was designed for school-aged children who are aware that their parents have cancer. The six two-hour closed-group sessions were held weekly. During each session, the children worked on art activities as a group. The sessions followed a standard format beginning with a warm-up, proceeding to the “feeling of the day” activity, a goal activity, and, finally, closure. The goals and activities of each session for children are explained in Table 1. Throughout all sessions, children were encouraged to share their feelings about a parent's illness. The children's group intervention was led by professionals who had experience working with oncology or pediatric patients. The group leaders included a social worker, a psychologist, and a child-life specialist, all of whom had attended the CLIMB® training workshop. Each session included assistants who were experienced in working with children, such as child-life specialists, nurses, and graduate students of psychology.
Table 1. Content of the CLIMB® Program for the children's group

We held concurrent parent group sessions separate from those with the children. These were led by a psychologist facilitator and an assistant who was either a nurse or a graduate student of psychology. The goals for our parent group were to reduce parents' anxiety and distress related to their child's stress, and also to improve communications between parents and children. In the parental group, we explained the aims and content of the program. We emphasized that having conversations with their children about the artwork from each child session might improve communication with the children. During open discussion time, we encouraged parents to share their feelings about their and their children's situations. At the beginning of each subsequent session, the facilitator asked parents about how they and their children talked about the child's art activity. We also requested that the parents share about the children's emotional state at home or at school and regarding family experiences during the past week. As parents shared in open discussions, some of the issues that emerged were how to talk about cancer-related issues with their children and how to communicate with the personnel at the child's school.
Participants
We enrolled children and parents in six waves of replicate sets between August of 2010 and December of 2012. The study inclusion criteria were: (1) a parent diagnosed with cancer and undergoing treatment, and (2) school-aged children between the ages of 6 and 12 whose parents had cancer and who had been informed previously that the parent had cancer. The exclusion criteria were: (1) patients with terminal-stage cancer, (2) patients with cancer and concurrent serious mental health issues, and (3) school-aged children with severe mental health or mental retardation disorders.
Setting and Procedures
Our study was conducted in Tokyo. The first group intervention was held at the Graduate School of the International University of Health and Welfare in Tokyo, and the remaining five group interventions were conducted at the Tokyo Kyosai Hospital. Before we began our research, the study was approved by the research ethics committee of the International University of Health and Welfare.
Study team members recruited parents and children from three hospitals in Tokyo where the authors have affiliations, and through information on the Hope Tree website (http://www.hope-tree.jp/). The Hope Tree is a volunteer organization of oncology professionals that was established in 2008 to disseminate information about supporting children whose parents have cancer. After potential participants were identified through team member referral or self-referral via the website, they were screened for study inclusion. We (first author M.K. and third author K.O.) interviewed parents directly or by telephone to explain the goals and details of the program and to describe what was entailed in research participation. During this interview, we completed a family assessment to ascertain the parent's diagnosis, treatment, and family situation. In addition, we assessed the children's situation and their understanding of their parent's cancer. After the interview, parents were mailed an information packet regarding the study that included a letter, a flyer about CLIMB®, and a copy of the informed consent form. Informed written consent to participate in our study was obtained from parents and children prior to the first intervention session.
We used several approaches to examine the feasibility of the intervention and assure intervention fidelity—that is, purity, participant satisfaction, and dosage. Purity establishes if the intervention is delivered consistently and as planned (Gearing et al., Reference Gearing, El-Bassel and Ghesquiere2011). The group facilitators followed the Japanese version of the script, manual, and time schedule for each session. After sessions, the group facilitators conducted meetings to identify any concerns or problems within the group, and strategies for handling these concerns were discussed and implemented. We gathered information about child and parent participants' perceptions of the value of the group to obtain participant satisfaction. In addition, we measured the dosage of the intervention by recording attendance data.
Children and parents were evaluated at two timepoints: (1) one week before the group intervention and (2) within three days after the group intervention. Parent participants provided demographic and medical information about themselves and their children at baseline.
Study Measures
Patient demographic data and treatment-related data were obtained through self-report. Standardized questionnaires were used to measure study outcomes. We used two measures for children and three for parents, as described below, pre- and post-intervention. In addition, we asked them to answer a questionnaire about their satisfaction with the program. We chose instruments for assessment of the children that focused on emotions associated with stress, particularly posttraumatic stress reactions, because of the documented association between parental cancer and these problems. Further, the CLIMB® Program was specifically designed to decrease stress and help children learn positive ways to cope with such negative emotions as anger. Similarly, our parental instruments were chosen to fit our outcomes.
Children's Assessment
The Public Health Research Foundation-Type Stress Inventory (PSI)
The PSI (Sakano et al., Reference Sakano, Okayasu and Shimada2007) is a self-report questionnaire for school-aged children that was developed and standardized in Japan. We used the stress response (SR) and social support (SS) scales to assess children's psychosocial stress. The SR has 12 items and is divided into 4 subscales: (1) physical (e.g., feel tired); (2) depression/anxiety (e.g., feel lonely); (3) irritation (e.g., become irritated); and (4) helplessness (e.g., cannot concentrate). Each scale score ranged from 0 to 12, with higher scores indicating worse physical and emotional outcomes. In addition, the SS subscale rates a child's perception of the support that they receive from their parents, teachers, and friends in their daily lives—for example, “When you are feeling down, [your father] will encourage you.” Scores range from 0 to 9, with higher scores indicating better relationships.
The Posttraumatic Stress Disorder–Reaction Index (PTSD–RI)
The PTSD–RI is a self-report questionnaire utilized to assess the frequency of PTSD symptoms in school-aged children and adolescents (Pynoos et al., Reference Pynoos, Frederick and Nader1987; Stuber et al., Reference Stuber, Nader and Yasuda1991). We employed the Japanese version of the PTSD–RI, which has 18 items, rated from 0 (“none of the time”) to 3 (“most of the time”). The children were asked to rate each item with respect to their parents' illness or cancer as the potentially traumatic event. Total scores ranged from 0 to 54, with higher scores indicating a more severe level of reaction. The standardization of the Japanese version of PTSD–RI was performed by Izumi (Reference Izumi and Izumi2008), who employed illustrations for each item so that younger children could more easily answer the PTSD–RI questions.
Parents' Assessment
Functional Assessment of Chronic Illness Therapy–Spiritual Well-Being (FACIT–Sp)
The FACIT–Sp (Cella et al., Reference Cella, Tulsky and Gray1993; Webster et al., Reference Webster, Odom and Peterman1999) is a self-rating questionnaire for any type of patient with cancer, which includes an additional spirituality scale. This measure was developed and standardized by Cella et al. (Reference Cella, Tulsky and Gray1993). It consists of general questions divided into four primary QoL domains: (1) physical well-being (7 items); (2) social/family well-being (9 items); (3) emotional well-being (6 items); and (4) functional well-being (7 items); as well as spirituality (12 items). Higher scores indicate better quality of life. This questionnaire can measure the comprehensive and spiritual quality of life of a patient with cancer. The reliability and validity of the Japanese version of the FACIT–Sp for patients with cancer were confirmed by Noguchi et al. (Reference Noguchi, Ohno and Morita2004).
The Hospital Anxiety and Depression Scale (HADS)
The HADS (Zigmond & Snaith, Reference Zigmond and Snaith1983) is a 4-point, 14-item, self-report questionnaire used to assess psychological distress. It includes two subscales: anxiety and depression. Each subscale has 7 items, and total scores range from 0 to 42, with higher scores indicating higher levels of psychological distress. The reliability and validity of the Japanese version of the HADS were confirmed by Kugaya and coworkers (Reference Kugaya, Akechi and Okuyama1998).
The Impact of Event Scale–Revised (IES–R)
The IES–R (Weiss & Marmar, Reference Weiss, Marmar, Wilson and Keane1997) is a 22-item self-report measure that assesses subjective distress caused by traumatic events. In our study, participants were asked to rate each item in relation to their cancer and its treatment, referring to their condition during the past seven days. IES–R assesses three dimensions of PTSD symptoms: intrusion, avoidance, and hyperarousal. Total scores range from 0 to 88, with higher scores indicating more severe levels of reaction. The reliability and validity of the Japanese version of the IES–R were confirmed by Asukai et al. (Reference Asukai, Kato and Kawamura2002).
Feasibility and Intervention Fidelity Measurement
A member of the study team kept an attendance log for the child and parent programs. Children and their parents completed the program evaluation questionnaire assessing their satisfaction with the CLIMB® Program after the group intervention. The questionnaires were originally developed by Heiney (Reference Heiney, Heiney and Peterson2006) in English, which we translated and modified slightly when creating the Japanese version. The children's questionnaire includes 10 items, and the parent's questionnaire includes 20 items with space for free-form descriptions. These questionnaires assess the satisfaction and acceptability of the intervention. The items are rated on a Likert-type scale from 0 (never/not at all) to 4 (exactly/very much).
Analyses
The impact of the group program was analyzed using a quasiexperimental within-subject design that compared pre- and posttest assessments of children and parents in separate exploratory analyses to determine changes in the children's stress and the parents' QoL and psychosocial distress.
Descriptive statistics were utilized to summarize all demographic and medical characteristics of the parents and children. Pre- and post-intervention differences were examined using dependent-samples t tests on children's stress and parents' QoL and psychosocial distress. Additional analyses included Pearson's chi-squared tests and independent-samples t tests. All tests were two-tailed, and the threshold for statistical significance was set at a value of p ≤ 0.05. All data were analyzed using the Statistical Package for Social Sciences software (v. 22.0, SPSS Inc., Chicago, IL).
RESULTS
Sample
Our study enrolled 32 parents (25 patients and 7 spouses) and 39 children as group participants. Among these participants, the study sample for the evaluation was composed of 24 parent/patients (23 mothers and 1 father) who were diagnosed with cancer and 38 of their school-aged children (27 girls and 11 boys). We excluded 7 spouses and 1 sister (older than 12 years old) from the questionnaire study, and 1 mother failed to submit her questionnaire.
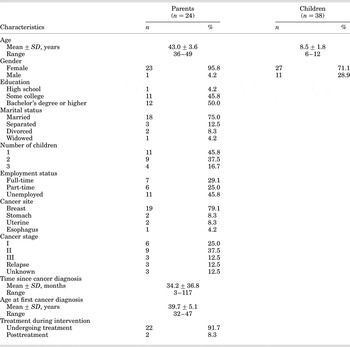
Parents were aged 36–49 years (mean ± SD = 43.0 ± 3.6), and the children were 6–12 years old (mean ± SD = 8.5 ± 1.8). Table 2 describes the study participants at baseline. Some 75% of the adult participants were married and lived together, and the rest were either single or separated. A total of 11 parents reported having a single child, 9 had 2 children, and 4 had 3 children. Some 13 of the 24 parents revealed that they were employed full- or part-time. Most parents were diagnosed with breast cancer (n = 19), while the remaining 5 parents were diagnosed with cancer of the stomach (n = 2), uterus (n = 2), and esophagus (n = 1). A total of 15 parents (62.5%) were diagnosed with stage I or stage II cancer, 3 each were diagnosed with stage III cancer or a relapse, and 3 were diagnosed with a cancer of unknown stage. Some 22 parents (91.7%) were undergoing treatment at the time of the group intervention, and 2 had finished their treatment.
Table 2. Participant descriptive characteristics
Exploratory Outcomes
Feasibility, Acceptability, and Intervention Fidelity
Child participant attendance (n = 38) at the six total group sessions ranged from 3 to 6 sessions, with a mean ± SD attendance of 5.34 ± 0.85 sessions and a median of 6. Similarly, patient/parent participants (n = 25) attended 5.44 ± 0.82 sessions, with a median of 6. Attendance records indicated that the majority of children (89.5%) and their parents (91.7%) attended 5 or more program sessions.
According to the program evaluation, both children and parents experienced high levels of satisfaction on all the items except one (29 of 30 items). The mean scores for each item for children ranged from 3.43 to 3.95 (10 items, selected from 0 to 4)—for example, “Making crafts helped me express feelings” (3.43) and “I'm glad I attended group” (3.84). The mean parent scores were 3.49–3.97 (19 items)—for example, “It helped my child cope better” (3.73) and “Staff were compassionate and caring” (3.97). Only “Location of services was convenient” (2.78) received a low evaluation.
Some of the verbatim feedback on program evaluation from parents included the following: “The children's anxiety are cleared, and they can deal with their feelings in their own ways”; “The bond between us deepened, and I feel my child grew up in many aspects”; “Learning about cancer and knowing it's not only my child whose parent has cancer helped my child most”; “Thanks to staff, I was able to get back to my everyday life”; and “All my children attended as siblings, and they became closer. I am feeling much lighter now as a parent.”
Comparison of Scores on Measures of Pre- and Post-Intervention
Our aim was to evaluate the impact of the Japanese version of the CLIMB® Program on selected child and parent variables. These data should be interpreted cautiously, as all analyses were exploratory in nature. Tables 3 and 4 present the mean ± SD values for each study measure for children and parents at baseline and post-intervention, as well as the results of comparative t tests.
Table 3. Comparison of pre- and post-intervention scores for assessment measures among children

N = 38; SD = standard deviation; CI 95% = 95% confidence interval; PSI = Public Health Research Foundation Type Stress Inventory; PTSD–RI = Posttraumatic Stress Disorder Reaction Index.
a Change in mean score between the pre- and post-intervention assessments; dependent-samples t test, two-tailed significance.
Table 4. Comparison of pre- and post-intervention scores for assessment measures among parents

N = 24; SD = standard deviation; CI 95% = 95% confidence interval; FACIT–Sp = Functional Assessment of Chronic Illness Therapy–Spiritual Well-Being; FACT–G = Functional Assessment of Cancer Therapy–General; HADS = Hospital Anxiety and Depression Scale; IES–R = Impact of Event Scale–Revised.
a Change in mean score between the pre- and post-intervention assessments; dependent-samples t test, two-tailed significance.
On the PTSD–RI, we found a significant decline from a mean ± SD of 18.22 ± 7.67 at pre-intervention to 14.76 ± 8.72 at post-intervention for posttraumatic stress symptoms (t = −2.72, p = 0.010). In particular, we noted significant declines in the following items (p < 0.01): “feeling it's my fault the event happened” and “remember the event suddenly and feel terrible,” in relation to their parents' cancer as the potentially traumatic event. However, as for children's stress response and social support, no significant differences were found on the PSI.
Parental QoL measured by the FACIT–Sp significantly improved after the group intervention (p < 0.05) on four of five QoL dimensions. Improvement occurred in social/family well-being (SWB: t = 2.31, p = 0.030); emotional well-being (EWB: t = 2.21, p = 0.037); functional well-being (FWB: t = 2.47, p = 0.021); and spiritual well-being (SP: t = 2.21, p = 0.038). No significant changes were identified on the physical well-being subscale. Examples of the items that significantly improved (p < 0.05) are as follows: “I am satisfied with family communication about my illness” (SWB); “My work (including work at home) is fulfilling” (FWB); and “My illness has strengthened my faith or spiritual beliefs” (SP). An example for reduction was “I am losing hope in the fight against my illness” (EWB). No significant difference was found between pre- and posttest HADS scores (total: t = −0.40, p = 0.690). Similarly, IES–R scores did not change significantly (total: t = −0.19, p = 0.849).
Factors Related to Children's Posttraumatic Stress Symptoms
As mentioned above, the mean PTSD–RI scores for children declined significantly after the intervention, but some remained with a higher level. Therefore, after primary analysis, we identified the children's post-intervention PTSD–RI scores as the main outcome and examined which factors were related to them. We divided the child participants into two groups—“the high group” and “the low group”—based on the cutoff point for post-intervention PTSD–RI scores. A total of 13 children were placed in “the high group,” with scores of 17 or higher, subdivided into “moderate” (17–26), “severe” (27–39), and “most severe” (>40) levels; 24 children were placed in “the low group,” with scores of 16 or lower, subdivided into “slight” (8–16) and “normal” (0–7) levels of posttraumatic stress symptoms. Independent-samples t test and Pearson's chi-squared tests were performed to explore the relevant factors prior to the intervention (Table 5). According to these results, we have not found significant differences between the two groups among most demographic items (e.g., child's age, child's gender, having brothers/sisters or not, afflicted parent's age, and education), except among parents' marital status (married, living together or not) (p = 0.012), and among PTSD–RI scores before the intervention (p = 0.012).
Table 5. Comparison between PTSD–RI high and low group post-intervention scores among children

N = 37; PTSD–RI = Posttraumatic Stress Disorder–Reaction Index; cutoff scores = 16/17.
a High group is 17 or higher in moderate/severe/most severe levels.
b Low group is 16 or lower in slight or normal level.
The data were analyzed using an independent-samples t test or Pearson's chi-squared test, two-tailed significance.
* Parental data were double-counted when more than one child participated in the intervention.
DISCUSSION
The purpose of this pilot study was to examine the feasibility and acceptability and evaluate the outcome of the Japanese version of the CLIMB® group intervention on children's stress and parents' psychosocial distress. Our results should be considered tentative, as all of our analyses were exploratory in nature.
Our findings suggest that the intervention was well-received. Both children and parents were very satisfied with the program, as indicated by their evaluation questionnaires and also by their consistent attendance. The intervention seems to be highly acceptable for participants, and its feasibility has been confirmed.
The children's posttraumatic stress symptoms related to their parents' illness measured by the PTSD–RI decreased after the intervention. Through the group activities, we provided an opportunity for children to express and cope with their feelings about their parents' cancer and thus reduce stress. Our results suggest that the program had a positive impact on decreasing children's stress.
However, when we looked at the results in more detail, a third of the children remained with a high level of posttraumatic stress symptoms (higher than the cutoff of 16 points by the PTSD–RI) after the intervention. After dividing participants into two groups (high and low) and analyzing the related factors, we found that parents' marital status and the baseline PTSD score were related. Being a single parent and having a high PTSD score at baseline may be related to children's stress. Thus, some special care for these children may be needed, or perhaps supplemental follow-up sessions might be effective. Foran-Tuller et al. (Reference Foran-Tuller, O'Hea and Moon2012) emphasized the importance of PTSD assessment in children whose mothers had cancer and stated that the PTSD variable was the strongest explanatory outcome. Our findings are in line with that study, although the sources of the reports were different. They employed mothers' reports to assess children's posttraumatic stress symptoms, and their results were based on mothers' perceptions. Our approach may yield a stronger assessment, having been obtained from the children themselves using the PTSD–RI for children.
In contrast, no significant differences were found in the children's stress response (SR) and social support (SS) scores measured by the PSI between baseline and post-intervention. When baseline SR scores were compared with general data for elementary school children, the child participants had higher scores, but the scores did not exceed the normal range (Sakano et al., Reference Sakano, Okayasu and Shimada2007). The children's SS scores were high enough even at baseline. Social support may increase when a parent is diagnosed with cancer; but this may not be the case over the longer period of treatment. The timing of our assessment may have captured this increased attention but may not measure the long-term support needs of the children of cancer survivors.
As for parents, the FACIT–Sp results show that their QoL was improved after the intervention for all except the physical domain (i.e., social/family, emotional, functional, and spiritual well-being). The lack of change in physical well-being is not surprising, since most parents were undergoing treatment (chemotherapy, radiation therapy, or hormone therapy) during their study participation. This fact may explain why parents' QoL improvement was regarded as an outcome of the group intervention.
In contrast, parents' psychological distress (anxiety and depression) measured using the HADS did not show a significant decrease. In fact, half of the sample had reported high levels on the HADS at both the beginning and end of the intervention. Davey et al. (Reference Davey, Kissi and Lynch2013) reported similar results on depressive symptoms from their intervention study. One possible reason for the lack of decline is that the intervention period was too short to improve depression. In addition, it is possible that the intervention did not adequately target the depressive symptoms (Davey et al., Reference Davey, Kissi and Lynch2013). In the future, longer sessions or sessions specifically designed to address depression might better address this symptom. We also did not see a decrease in parental posttraumatic stress symptoms measured by the IES–R.
Overall, parental psychological distress did not significantly change after the group intervention; however, their QoL, which focused on emotional and social well-being in daily life, improved greatly. Thus, group intervention can help participants as parents but may not counter the personal suffering that results from a diagnosis of and treatment for cancer. Semple and McCance (Reference Semple and McCance2010) found three predominant themes from a literature review pertaining to a parent's experience with cancer: (1) being a good parent, (2) telling the children, and (3) maintaining normal routines at home. We suppose that group participation allows the parent to maintain his/her identity as a parent by talking and sharing with others about their parenting concerns in a peer group.
Finally, we considered the significance of the intervention for both children and parents. The CLIMB® Program is a peer group intervention for school-aged children (aged 6–12 years). During this developmental stage, children begin to seek more independence from their parents and want to spend more time with their peers (Heiney & Hermann, Reference Heiney and Hermann2013). The children in the CLIMB® intervention may have felt less isolated, since they could share their experiences and emotions about their parents' cancer with peers within a secure setting. As a result, their posttraumatic stress symptoms related to their parents' cancer declined. A major concern that parents expressed after a cancer diagnosis is “parenting” (Semple & McCance, Reference Semple and McCance2010). Worrying about their children's reactions also adds to parents' emotional stress (John et al., Reference John, Becker and Mattejat2013). Our findings suggest that children's stress concerning their parents' illness decreased after participation in the CLIMB® Program, which may have enhanced parents' well-being. Anecdotal observations of group facilitators for parent groups indicated that talking about their cancer-related problems was a difficult obstacle to overcome before program participation even though their children knew about their diagnosis. However, parents found that it was much easier to communicate about their cancer within the family after participating in the program. Interventions focused on family communications may benefit children and, through improved relationships, enhance parent/patients' QoL (Watson et al., Reference Watson, St. James-Roberts and Ashley2006). Niemela et al. (Reference Niemela, Repo and Wahlberg2012) suggested that peer group interventions impact the psychological well-being of patients, even when the purpose is to support parenting and children. The strength of our group intervention, the Japanese version of the CLIMB® Program, was that we provided concurrent groups for both children and parents. Further objective study will be necessary on this point.
The group intervention we provided for children experiencing parental cancer was the first of this type to be offered in Japan. Moreover, to participate in this program, children had to know that their parents had been diagnosed with cancer. In Japan, parents have a good deal of difficulty in telling their school-aged children about a cancer diagnosis. Therefore, recruiting participants was difficult and a control-group design could not be adopted. However, our pilot study provides important insights and information regarding the changes seen in participants from pre- to post-intervention assessments. As the results of our study suggest, the children who experienced parental cancer have concerns focused on their parents' illness (posttraumatic stress symptoms), even though they might not manifest distress in daily life. The CLIMB® group intervention can provide an effective opportunity for them to overcome their concerns. As for the parents, they may improve their quality of life (psychosocial and spiritual well-being) by means of the intervention.
LIMITATIONS OF THE STUDY
The main limitations of this pilot study are the small sample size and the lack of a control group. Due to the small sample size and examination of multiple outcomes, type I and type II errors are possible. Thus, effects may be over- or underestimated. Without randomized controls, we cannot provide sufficient evidence for the effects of the intervention. Additional research with larger samples is required to be able to generalize these results. Moreover, because of the small sample size, we did not assess the impact of the intervention with respect to sex differences. It is certainly very important that sex differences be considered in future research.
Second, we did not assess the long-term effects of the intervention, so our findings are only relevant to the possible short-term impact of the group intervention. Third, the instruments we chose to employ may not have been the best tools for measuring the effects of the group intervention. For example, we did not examine children's QoL, coping styles, or family communication styles. Fourth, children may not be able to adequately self-report their symptoms and situations. Better instrumentation and assessment methods are required to be applied in future research. Finally, our study only performed quantitative analyses. Qualitative methods may have provided further enlightenment regarding how to improve clinical practice. However, this interventional study was the first such trial in Japan, so we believe that our work is a valuable step toward improved child support.
CLINICAL IMPLICATIONS
There is an increasing awareness of the importance of providing support for the children of patients with cancer by medical professionals in Japan. It is thought that group intervention for both parents and children using the CLIMB® Program is an effective approach to supporting children after they have learned of their parents' cancer diagnosis. This is a structured program, so that any medical professional can easily learn how to administer it using the training workshop and manualized materials. Moreover, special facilities are unnecessary, and the costs are minimal. We will continue our advocacy to increase hospital presentations of the CLIMB® Program by helping them launch the program so that more children and patients will be able to attend.
ACKNOWLEDGMENTS
We wish to express our appreciation to Emi Inoue, Eriko Miura, and Yukiko Murase, child-life specialists who provided valuable guidance in adapting the program for Japanese children. We would like to deeply thank all the children and parents who participated and the group facilitators from the Hope Tree for their contributions to our study. We are grateful for the support of Peter van Dernoot from the Children's Treehouse Foundation, who allowed us to adapt the CLIMB® Program. We also thank Sachiko Ohde from the Center for Clinical Epidemiology at St. Luke's International University for her professional advice.
FUNDING
This study was supported by a research grant, “Child Support in Clinical Cancer Practice,” from the Japanese Ministry of Health, Labour, and Welfare (2010–2012).







