Introduction
Inverted nasal papilloma is a benign tumour with variable biological behaviour. It is a unique neoplasm and is often difficult to manage, being characterised by a tendency to recur following excision, an association with malignancy and an ability to destroy bone. The impact of this tumour on patients' health relates to: (1) reduced quality of life due to compromised nasal function; (2) extension to the orbit (occurring in 1–8 per cent) or the brain, which, rarely, can lead to death; and (3) the association with neoplasia.Reference Karkos, Fyrmpas, Carrie and Swift1
Ideal management should aim for complete removal of diseased mucosa with creation of wide cavities, and long term follow up to detect recurrence or malignant transformation. The lack of a universally accepted staging system means that the need for detailed pre-operative planning is even greater; this is where imaging plays a pivotal role.
The aim of this review was to assess the evidence regarding the ideal imaging modality for pre-operative planning of surgery for patients with histologically proven inverted nasal papilloma. The advantages and disadvantages of magnetic resonance imaging (MRI) and computed tomography (CT) are also discussed, as are the controversies regarding the radiological diagnosis of inverted nasal papilloma.
Methods
Studies were located using systematic searches of the Medline, Embase, Cinahl and Cochrane library electronic databases, together with hand searching of key texts, references and reviews relevant to the field. References from relevant articles were also searched. Medical subject headings used for searching included the terms ‘inverted’, ‘inverting’, ‘papilloma’, ‘nose’, ‘sinuses’, ‘sinonasal’, ‘paranasal’, ‘computerised tomography’, ‘radiology’ and ‘diagnosis’.
Inclusion criteria
Our inclusion criteria were English language publication, and randomised and non-randomised, prospective and retrospective trials focusing on radiological assessment of inverted nasal papilloma.
Exclusion criteria
We excluded single case reports, case series and reviews of inverted nasal papilloma not focusing on pre-operative imaging. We also excluded studies on endoscopic surgery under image guidance, papers on positron emission tomography, and papers comparing CT with plain sinus X-rays and/or pluridirectional tomography.
Results
A formal metanalysis was prevented by selection bias, blinding of results, lack of common outcome measures and uncontrolled studies, amongst other problems. The literature review identified 16 articles, of which eight fulfilled our criteria. Table I summarises these eight articles in chronological order. All were retrospective, controlled, level three studies.
Table I Summary of studies on radiological assessment of inverted nasal papilloma

* Studies comparing computed tomography (CT) and magnetic resonance imaging (MRI). Yr = year; Pts = patients; Y = yes; N = no
In their study of 29 patients, Dammann et al. concluded that there were distinctive radiological features in the majority of CT scans of patients with primary inverted nasal papilloma.Reference Dammann, Pereira, Laniado, Plinkert, Lowenheim and Claussen2 Unilateral tumour localisation involving the lateral nasal wall and the middle meatus was the feature that best correlated with a diagnosis of primary inverted nasal papilloma. A unilateral mass with a lobulated pattern was another typical sign in 26 out of 28 scans of patients with tumour recurrence.
Savy et al. also conducted a 20-year retrospective study, and suggested that the main advantage of MRI is in defining the extent of inverted nasal papilloma and differentiating this from adjacent inflammatory tissue.Reference Savy, Lloyd, Lund and Howard3 These authors found no characteristic signal intensity or enhancement signs to help differentiate inverted nasal papilloma from sinus malignancy. However, they proposed that the combination of bone deformity and sclerosis on CT scanning together with the typical antro-meatal mass suggested a slow-growing tumour such as inverted papilloma.
A study performed by three blinded radiologists confirmed that the presence of convoluted, cerebriform morphology seen within a lesion on MRI was consistent with inverted nasal papilloma (eight of 10 cases). Ojiri et al. conducted a retrospective review of the MRI scans of 10 patients with a histologically proven diagnosis of inverted nasal papilloma who were awaiting treatment.Reference Ojiri, Ujita, Tada and Fukuda4 They concluded that a solid tumour occupying the middle meatus and maxillary sinus, with a convoluted, cerebriform appearance on T2-weighted images or enhanced T1-weighted images, strongly suggested inverted nasal papilloma. Deviation from this convoluted, cerebriform pattern suggested an alternative diagnosis or concomitant inverted nasal papilloma and squamous cell carcinoma.
Petit et al. conducted another radiological follow-up study, of 42 patients with inverted nasal papilloma, and found that MRI appeared to be more efficient than CT for detection of recurrences.Reference Petit, Vivarrat-Perrin, Champsaur, Juhan, Chagnaud and Vidal5 On MRI, recurrences were always visible. However, on CT the masses presented an intermediate T1-weighted signal (identical or higher than the signal for muscle) but were not distinguishable from surrounding hyperplastic mucosa. After gadolinium administration, the contrast enhancement was slightly heterogeneous and lower than that of normal or hyperplastic mucosa. On T2-weighted sequences, the tumoural signal intensity was low to intermediate, and recurrences were easily distinguishable from fluid and mucosa.
Oikawa et al. retrospectively reviewed 21 cases investigated with MRI, while being unaware of the surgical and pathological findings.Reference Oikawa, Furuta, Oridate, Nagahashi, Homma and Ryu6 They found the positive predictive value of MRI for the diagnosis of tumour involvement to be 68 per cent (89 per cent in each sinus), while the negative predictive value was greater than 93 per cent. These authors concluded that MRI could accurately predict the extent of inverted nasal papilloma involvement of the paranasal sinuses. Furthermore, MRI T2-weighted images and T1-weighted, gadolinium-enhanced images were able to successfully differentiate tumours from inflammatory tissue, and may therefore be useful for planning an appropriate surgical approach. However, according to Oikawa et al., there was a risk of overestimation of tumour involvement and over-treatment, leading potentially to increased morbidity.Reference Oikawa, Furuta, Oridate, Nagahashi, Homma and Ryu6
Maroldi et al. attempted to identify distinguishing features of inverted nasal papilloma on MRI scans, and found a columnar pattern in all their 23 cases when using enhanced spin-echo T1 images, and in 16 of the 23 cases when using spin-echo T2.Reference Maroldi, Farina, Palvarini, Lombardi, Tomenzoli and Nicolai7 These authors concluded that such a columnar pattern was a reliable MRI indicator of inverted nasal papilloma (having a positive predictive value of 95.8 per cent) and reflected its histological architecture. The combination of this finding with the absence of extended bone erosion allowed confident discrimination of inverted nasal papilloma from other malignant tumours.
Head et al. conducted a more recent, retrospective study of 77 cases of biopsy-proven inverted nasal papilloma in which they were not blinded to patients' diagnoses. They concluded that both CT and MRI defined the extent of histologically proven, recurrent disease, although it was impossible to distinguish recurrent disease from post-operative scarring or mucoperiosteal thickening. Computed tomography was more helpful for evaluation of primary, non-recurrent inverted nasal papilloma.Reference Head, Sercarz, Luu, Collins and Blackwell8
Yousuf and Wright reported a recent, bipartite study with retrospective and prospective arms.Reference Yousuf and Wright9 Osteitis was seen in 25 out of 28 patients with inverted nasal papilloma. The authors concluded that, in patients in whom osteitis was detectable on the pre-operative CT scan, the site of origin of the inverted nasal papilloma could be predicted with a high degree of accuracy.
Discussion
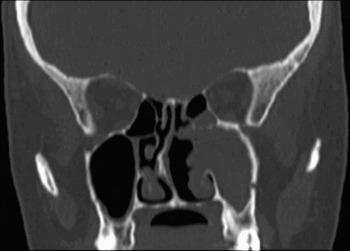
Computed tomography has traditionally been used as the standard pre-operative examination to evaluate the degree of sinus involvement in cases of inverted nasal papilloma, and to determine the extent of surgery.Reference Oikawa, Furuta, Oridate, Nagahashi, Homma and Ryu6 Both axial and coronal CT scans should be obtained; however, these images are not completely diagnostic and will not differentiate inverted nasal papilloma from inflammatory changes within the sinus. Even experienced head and neck radiologists have difficulty in diagnosing inverted nasal papilloma without a histological report, and this diagnostic difficulty is well reflected in the literature.Reference Dammann, Pereira, Laniado, Plinkert, Lowenheim and Claussen2–Reference Yousuf and Wright9 Inverted nasal papilloma usually presents with symptoms of unilateral nasal obstruction or sinus disease. A CT scan is usually performed, which generally shows a pattern consistent with sinus disease with obstruction of the middle meatus; occasionally, there are signs of a mass with bone destruction or, more likely, sclerosis. These findings necessitate MRI, which is perhaps better at showing a mass and differentiating inverted nasal papilloma from adjacent inflammatory disease (Figure 1).Reference Ojiri, Ujita, Tada and Fukuda4–Reference Yousuf and Wright9 Imaging scans are helpful if they do show a mass due to inverted nasal papilloma, but accurate staging is much more difficult.Reference Karkos, Fyrmpas, Carrie and Swift1 The advantage of CT scanning in the pre-operative planning of inverted nasal papilloma surgery lies in identifying the presence of tumour invasion of adjacent bony structures, and any bony sclerosis secondary to this (Figures 2 and 3). Unfortunately, it is often impossible to differentiate between inverted papillomas and polyps with entrapped debris.Reference Karkos, Fyrmpas, Carrie and Swift1 The morphology of lesions shown on CT scans is often non-specific. Thus, CT cannot distinguish tumour from adjacent inflammatory mucosa or retained secretions, often resulting in overestimation of the size and extent of an inverted papilloma and misleading the surgeon to consider a more invasive operation. The operation itself can range from less invasive endoscopic procedures to invasive open surgery with increased post-operative morbidity rates.

Fig. 1 (a) T2-weighted, coronal magnetic resonance imaging (MRI) scan showing a mass in the left ethmoid region with retained secretions in the left maxillary antrum, due to obstruction of the middle meatus. Loss of bony anatomy, due to the destructive process, is also shown. (b) Axial MRI view of the same patient.

Fig. 2 Coronal computed tomography scan showing nodular mass lesion at the left osteomeatal complex, with bone erosion and opacification of the left maxillary antrum.

Fig. 3 Coronal computed tomography scan showing inverted papilloma of the left ethmoid and antrum, and displaying associated hyperostosis.
Magnetic resonance imaging, including T2-weighted images and T1-weighted, gadolinium-enhanced images, has more recently been advocated as being more capable of assessing tumour involvement.Reference Lane and Bolger10 Inverted nasal papillomas usually show intermediate signal intensity on T2-weighted images (as indeed do most sinonasal tumours). In contrast, T2-weighted images of inflammatory processes predominantly show bright signal intensities, often equalling those of mucosa or cerebrospinal fluid, which reflects a high water content due to interstitial oedema, serous fluid or mucous secretions.Reference Lane and Bolger10 On the other hand, acute sinusitis is often hypodense relative to tumour. Peripheral mucosal enhancement and lack of central enhancement may distinguish sinusitis from heterogeneously enhancing tumour.
In the most recent publications included in our review, MRI is obviously favoured as part of the pre-operative investigation of inverted nasal papilloma. However, there is currently not enough evidence to prove that MRI is better than CT in identifying inverted papilloma pre-operatively.
Conclusion
Accurate tumour delineation is critical in planning appropriate surgical extirpation of inverted papillomas. This is mainly because endoscopic surgery may not be suitable when the tumour is detected in endoscopically inaccessible regions (e.g. the periorbital region, lacrimal sac, supraorbital ethmoidal air cells or frontal sinus). Pre-operative radiological planning plays an important role in determining the extent of the lesion and invasion of adjacent structures. Therefore, choosing the appropriate imaging modality, without wasting healthcare resources, is pivotal. There is an obvious trend – apparent from the current review – towards MRI as the first investigation for inverted nasal papilloma. Its capability in separating soft tissue from secretions and in further characterising the features of the lesion is the main reason for its increased diagnostic sensitivity, as observed by Maroldi et al. Reference Maroldi, Farina, Palvarini, Lombardi, Tomenzoli and Nicolai7 Nevertheless, there is currently insufficient evidence to support this assertion (the existing evidence is of levels three to four). There is a need for a well designed, prospective, blinded study comparing CT with MRI for histologically proven inverted nasal papilloma. Until then, a combination of the two imaging modalities is perhaps the ideal – although, admittedly, not always the most cost-effective choice.