Isolated chylopericardium is a rare clinical entity. It may be caused by surgical trauma, irradiation, tuberculosis, vena caval obstruction, and primary or metastatic mediastinal tumours. Congenital lymphangiomatosis and lymphangiectasia may also cause chylopericardium. Primary idiopathic chylopericardium is a very rare disease with an unknown aetiology. Only a few reports exist regarding children with primary idiopathic chylopericardium.Reference Lin, Sun, Yu, Yang, Lin and Wang 1 – Reference Musemeche, Riveron, Backer, Zales and Idriss 9 We therefore present the case of a child diagnosed with a chylopericardium who was successfully managed in our department.
Case report
A 5-year-old boy presented to our hospital on 24 March, 2011, with a 10-day history of cough and mild dyspnoea over the previous 1 day. He had no fever, chest pain, cyanosis, weight loss, or oedema of the hands and feet. On admission, physical examination findings revealed bulging of the chest wall with distant heart sounds. His heart rate was 105 bpm, and his blood pressure was 95/75 mmHg. Further investigations were performed. Chest radiography showed an enlarged cardiac silhouette (Fig 1), while a computed tomography scan of the chest showed an enlarged heart with signs of a massive pericardial effusion (Fig 2). Echocardiography confirmed a massive pericardial effusion. Laboratory tests showed negative blood cultures, negative urine cultures, normal serum electrolytes, normal blood glucose levels, and normal renal and hepatic function. Serological tests were negative for hepatitis B, hepatitis C, and tuberculosis. The Mantoux and Myco pneumoniae immunoglobulin M tests were negative.

Figure 1 Anteroposterior chest X-ray showing a severely enlarged cardiac silhouette.
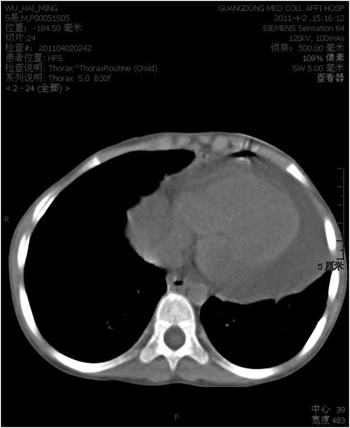
Figure 2 Chest computed tomography confirmed that the pericardial sac was filled with an effusion and excluded the presence of a neoplasm or congenital malformation.
Pericardiocentesis was performed, and a 4-F pigtail catheter was left in the pericardial space. A milky fluid was drained via the pigtail catheter. The cholesterol level of the pericardial fluid was 1.65 mol/l. No organisms were seen, and Gram staining and cultures were both negative. The leucocyte cell count was 13.50 × 103/mm3, of which 95% were lymphocytes.
On the 1st day, 150 ml of chylous fluid was drained, but pericardial fluid continued to reaccumulate. Over the following 2 weeks, an average of 200–300 ml chylous fluid was drained each day. The patient was placed on a low-fat diet with nutritional support. However, repeated echocardiography showed the continued presence of a pericardial effusion. Surgery was performed and the chyle was identified to be leaking from the thoracic duct at a point close to the left subclavian artery (Fig 3). The site of the leak was doubly ligated. The pericardium was full of chylous fluid, and this was evacuated. In order to drain the pericardial sac effectively and to prevent a later constrictive pericarditis, a pericardial window was created. A repeated echocardiogram 1 week post-operatively showed only the trace of a pericardial effusion. The patient was discharged on the 7th day after surgery.

Figure 3 The forceps show the thoracic duct 2 cm above the aortic hiatus of the diaphragm under thoracoscopy.
Discussion
Idiopathic chylopericardium occurs in all age groups, and the confirmed youngest case to date was suspected by echocardiography in a foetus and confirmed after birth.Reference Lin, Sun, Yu, Yang, Lin and Wang 1 Primary idiopathic chylopericardium develops very slowly over a long time period. Huang et alReference Huang, Wang, Li, Chen and Wang 2 reported a case that had developed over 70 months. Affected patients usually present with cough, dyspnoea, and wheeze on admission. Up to 40% of cases are asymptomatic, and cardiac tamponade is rare (6%).Reference Martinez-Pajares, Rosa-Camacho, Camacho-Alonso, Zabala-Arguelles, Gil-Jaurena and Milano-Manso 6 This current case presented with a cough that had been present for only 10 days and mild dyspnoea for 1 day, and was initially diagnosed with bronchitis on admission. However, cardiac effusion was suggested because of the bulging chest wall and distant heart sounds with liver enlargement. The true onset of his illness remains unknown. Chest radiographs demonstrated cardiomegaly, and the diagnosis was confirmed by echocardiography, chest computed tomography, and pericardiocentesis.
When the diagnosis of chylopericardium has been established, a search for the underlying cause should be made. Investigations that specifically look for bacteria, tuberculosis, and lymphoma should be performed in children. Our patient had no specific history suggestive of a specific pathology, and there was no evidence of infection with tuberculosis or other pathogens. Therefore, the diagnosis of primary idiopathic chylopericardium was established.
The cause of primary idiopathic chylopericardium remains unknown. The possible modes of pathogenesis include damage of the valves in the thoracic duct or the branches that connect the thoracic duct and lymphatic system in the pericardium; high pressures within the thoracic duct (>15 cmH2O); or a communication between the lymphatic system and the pericardial sac.Reference Huang, Wang, Li, Chen and Wang 2
Treatments for primary idiopathic chylopericardium include conservative treatment by continuous pericardial drainage and low-fat total parenteral nutrition, and surgical procedures that consist of ligation of the thoracic duct and pleuropericardial window. Lin et alReference Lin, Sun, Yu, Yang, Lin and Wang 1 reported a case of congenital idiopathic chylopericardium that was diagnosed at birth and cured by conservative treatment with catheter drainage alone. Another 2-month-old infant reported by López-Castilla et alReference López-Castilla, Soult and Falcón 8 was also cured by catheter drainage, which suggests that conservative treatment is effective in infants. However, most cases will fail conservative treatment, and surgery is then needed. Many reports have shown that the ligation of the thoracic duct and the establishment of a pleuropericardial window via a left thoracotomy are effective surgical interventions. In this case, we performed both by thoracoscopy.
The purpose of surgery is to reduce the inflow of lymphoid liquid from the thoracic duct into the pericardial cavity, but it is unknown whether thoracic duct ligation impacts the prognosis.Reference Attias, Ou, Souillard, Boudjemline, Sidi and Bonnet 10 Chylopericardium can relapse or develop into constrictive pericarditis, and therefore a long duration of follow-up is necessary.
To conclude, primary idiopathic chylopericardium is a rare condition in children, and its treatment includes a low-fat diet enriched with medium-chain triglycerides. If this conservative approach fails, surgical ligation of the thoracic duct and the creation of a pericardial window are required, as described in this patient. Thoracoscopy is a convenient and effective surgical method for these procedures.





