Introduction
The standard technique for cochlear implantation involves a transmastoid facial recess approach. However, successful cochlear implantation can be prevented by anatomical variations limiting surgical exposure, as well as by pathological changes to the middle and inner ear. A poorly developed mastoid with an anterior sigmoid sinus may limit access to the facial recess. Access to the middle ear and round window niche via the facial recess may be limited by an aberrant facial nerve in the congenitally malformed ear. Cochlear dysplasia may obscure anatomical landmarks. Acquired pathologies, such as cochlear otosclerosis, chronic middle-ear disease and post-meningitic cochlear ossification, may prevent identification of the round window. Canal wall down mastoidectomy with total removal of the external auditory canal squamous epithelium and middle-ear mucosa and closure of the ear canal has been proposed in these challenging cases. We describe a canal wall down technique which extends the facial recess exposure while preserving the posterior canal wall skin, and report a series of three patients in whom standard cochlear implantation was either impossible or extremely difficult, who benefited from the alternative surgical technique described.
Surgical procedure
The surgical area is prepared and draped in the standard fashion for cochlear implant surgery. The external auditory canal is filled with povidone-iodine solution. A 5 cm postauricular incision is used, and a mastoidectomy and facial recess approach are performed. The posterior ear canal wall is thinned to a ‘paper thin’ thickness. If adequate exposure of the middle-ear space and round window niche via the facial recess is impossible or extremely difficult, then the decision is made to remove the bony posterior canal wall.
The posterior ear canal skin is carefully elevated off the bony ear canal wall from a lateral to medial direction. The dissection is continued until the tympanic annulus is elevated and the middle-ear space is visualised. Careful preservation of the intact posterior canal skin is imperative. The skin is elevated off the canal down to the level of the annulus. With the posterior canal wall skin lifted, the posterior bony canal is removed with an otological drill (Figure 1). This allows further identification of, and greater access to, the middle ear. Cochleostomy and electrode insertion is then performed, after identification of the round window niche. The electrodes are deeply seated within the mastoid cavity, and the posterior canal skin is returned to its original position. No further reconstruction of the posterior ear canal is attempted. The postauricular incision is then closed in layers.
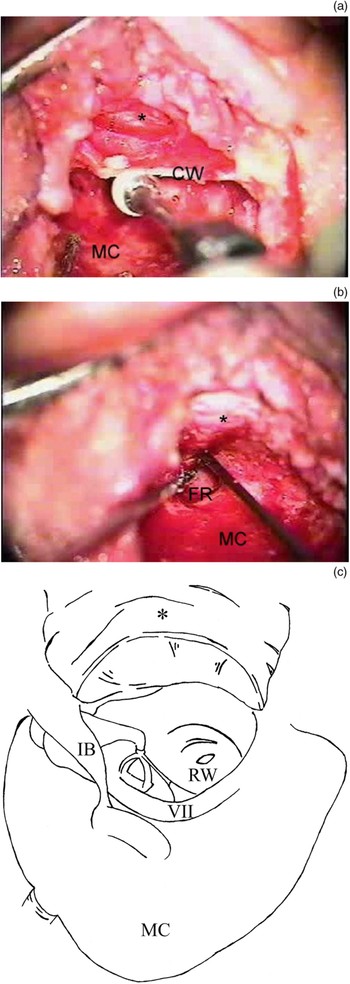
Fig. 1 (a), (b) Intra-operative view of the right ear of a patient with severe cochlear otosclerosis. The mastoid cavity (MC) has been developed and the facial recess (FR) completed. (a) The posterior meatal skin (*) has been elevated off the bony canal wall (CW), which has been partially drilled away. (b) The posterior bony canal wall has been removed completely. (c) Diagram of the surgical view, illustrating the additional exposure of the middle ear afforded by this technique. The mastoid cavity has been drilled out, the facial nerve (VII) identified, the facial recess opened and posterior canal wall removed with the incus buttress (IB) remaining in place. The intact posterior meatal canal wall skin (*), in continuity with the tympanic membrane, is shown retracted anteriorly. This allows for wide access to the middle ear and identification of the round window (RW).
Case reports
Case one
An 86-year-old woman with progressive hearing loss presented for evaluation of profound sensorineural hearing loss (SNHL).
Pre-operative high resolution computed tomography (CT) showed opacification of both mastoid and middle-ear cavities.
On examination, the tympanic membranes were without evidence of retraction bilaterally.
At the time of left-sided cochlear implantation, granulation tissue was found throughout the mastoid cavity and middle ear. The facial recess was opened without difficulty and was noted to be of normal dimensions. Due to the extensive granulation tissue, almost no normal middle-ear anatomical landmarks could be visualised. Dissection of the granulation tissue through the facial recess was extremely difficult, despite otherwise normal facial recess anatomy. At this point, the posterior canal wall was removed, while preserving the posterior canal skin. This created a much larger exposure for dissection of the middle-ear contents. The stapes superstructure was identified, encased in thick granulation tissue. This enabled identification of the round window niche and successful implantation with a Clarion II® implant (Advanced Bionics Corporation, Sylmar, CA, USA).
The patient had an unremarkable post-operative course. At the time of writing, she had been followed for six years post-operatively without evidence of retraction, wound complication or electrode extrusion.
Case two
A 76-year-old man with progressive, bilateral, profound SNHL was evaluated for cochlear implantation.
A high resolution CT showed the sigmoid sinus with significant anterior displacement in the left mastoid (Figure 2). The patient insisted on a left ear implant in order to protect his other, ‘better’ ear.

Fig. 2 Pre-operative axial, high resolution computed tomography scan of patient with anteriorly displaced sigmoid sinuses (SS).
At the time of left-sided implantation, the sigmoid sinus was found to be in contact with the bony posterior canal wall. The sigmoid sinus was completely skeletonised and compressed. Despite aggressive retraction of the sinus, adequate visualisation of the facial recess could not be obtained. The posterior canal wall was carefully drilled down with a cutting burr until the fossa incudis was identified, and the facial recess was developed. The cochleostomy was drilled and full insertion of a Nucleus 24® implant (Cochlear Corporation, Englewood, CO, USA) was accomplished. A small, iatrogenic fenestrum was identified in the posterior canal wall skin. A temporalis fascia graft was harvested and placed posteriorly over the fenestrum, and buttressed with a temporalis muscle graft.
The patient had an unremarkable post-operative course, with no evidence of external auditory canal fistula. At four and one-half years' follow up, the patient's otoscopic examination was unremarkable.
Case three
A 58-year-old man presented with progressive SNHL due to advanced otosclerosis.
An audiogram showed profound SNHL. High resolution CT showed evidence of severe cochlear otosclerosis.
Exploration of the middle ear revealed a dysmorphic promontory, without an identifiable round window niche. The posterior canal wall was removed, which aided identification of a small depression on the promontory in the usual location of the round window. During the cochleostomy, a significant amount of chalky bone was encountered, requiring a basal turn drill-out. Full insertion of a Nucleus 24® cochlear implant electrode (Cochlear Corporation, Englewood, CO, USA) was accomplished.
The patient's post-operative course was uneventful, except for a small dehiscence of the superior postauricular incision two months after surgery, which required reclosure. This dehiscence was unrelated to the canal wall down procedure. The incision healed completely without further complication. The patient stimulated fully and became an active implant user. At the time of writing, he had been followed for four years, with no long-term complications.
Discussion
The facial recess is a surgical window into the middle-ear space which allows visualisation of the round window niche for proper cochleostomy placement and electrode insertion. The round window niche is usually easily visualised through the facial recess. If visualisation of the niche is difficult, the posterior ear canal wall can be further thinned and the patient's head rotated until the desired anatomical landmarks are identified. If middle-ear landmarks still cannot be identified, or if the anatomy is not favourable for easy round window niche visualisation, the bony posterior ear canal wall can be completely removed. This allows the surgeon to further rotate the angle and field of view through the recess.
Meticulous elevation and preservation of the posterior canal skin and uninterrupted blood supply of the vascular strip are imperative for the success and safety of this technique. If the posterior ear canal skin is compromised and does not heal properly, then an ear canal to mastoid fistula may develop. This would essentially create an exteriorised implant with the possibility of infection and extrusion. A small defect in the skin flap was easily repaired with temporalis fascia in one of the cases presented. This patient recovered without further sequelae.
The otological surgeon may face numerous surgical challenges at the time of cochlear implantation. These challenges may be due to anatomical variations resulting in poor access, or to acquired disease processes that complicate implantation. A number of approaches have been described for cochlear implantation of the surgically challenging ear, in particular for the ossified cochlea, with good results.Reference Balkany, Gantz, Steenerson and Cohen1–Reference Balkany, Gantz and Nadol4 A cochlear drill-out procedure and partial insertion may be necessary for successful implantation. Congenital middle-ear and inner-ear dysplasia also presents challenges for cochlear implantation. Such patients are at greater risk of obscure middle-ear landmarks, facial nerve injury and development of a cerebrospinal fluid ‘gusher’.
A canal wall down approach may be necessary in order to prevent facial nerve injury and to identify middle- and inner-ear anatomy. Total removal of middle-ear mucosa and closure of the external auditory canal has been recommended in such cases.Reference Slattery and Luxford5, Reference Tucci, Telian, Zimmerman-Phillips, Zwolan and Kileny6 However, failure to completely remove the squamous epithelium may lead to cholesteatoma formation.
Several procedures, less extensive than closure of the external auditory canal, have been described for cochlear implantation of the anatomically challenging ear. Ito et al. described cochlear implantation in patients with common cavity malformation, using a canal wall down approach.Reference Ito, Sakota, Kato, Hazama and Enomoto7 The posterior canal was rebuilt with a temporal bone plate, bone dust and fibrin glue and covered posteriorly with temporalis muscle. Temporary dislocation of the posterior canal has also been described.Reference McElveen, Carrasco, Miyamoto and Linthicum8–Reference Sennaroglu and Aydin11 Sennaroglu and Aydin described a less extensive, anteroposterior approach involving a split ear canal for cochlear implantation in cases of severe congenital malformation.Reference Sennaroglu and Aydin11 The approach described in this paper avoids a more complicated procedure involving either closure of the external auditory canal or reconstruction of the posterior canal wall. It also avoids any additional, albeit small, risk of secondary cholesteatoma development (seen with external auditory canal closure) or foreign body reaction to potential alloplastic reconstructive materials.
Alternatives to transmastoid approaches for cochlear implantation have also been proposed. Transcanal approaches have been described which avoid mastoidectomy and facial recess development.Reference Kiratzidis12–Reference Kronenberg, Migirov and Dagan16 Middle fossa access for cochlear implantation has also been reported.Reference Colletti and Giorino17, Reference Colletti, Fiorino, Carner, Sacchetto, Miorelli and Carner18 However, both these procedures would ideally require pre-operative planning, rather than serving as a solution to intra-operative challenges. Additionally, surgeons less familiar with these alternative approaches for implantation may be more likely to have complications. Thus, for most otological surgeons, canal wall down, transmastoid procedures are likely to yield more favourable results when greater surgical access is needed.
Soft wall reconstruction of the posterior canal after canal wall down mastoidectomy (a similar technique to the current approach) has been previously reported in both inflammatory and noninflammatory conditions.Reference Bennett19–Reference Hosoi, Murata, Kimura and Tsuta25 Takahashi et al. reported using this approach on non-inflamed ears with normal mastoid mucosa function and with no evidence of eustachian tube dysfunction or chronic ear disease.Reference Takahashi, Honjo, Hasebe, Sudo and Tanabe22 In their series of 20 patients, one had slight retraction of the posterior external auditory canal, and 19 had no evidence of retraction post-operatively, despite the lack of a bony posterior canal wall. In addition, three of these subjects underwent mastoidectomy with soft wall reconstruction for cochlear implantation.
Conclusion
The intact skin, canal wall down technique for difficult cochlear implantation provides further access to the middle ear for cochleostomy in cases of obscured middle-ear landmarks and limited facial recess access. In this procedure, careful preservation of the posterior canal wall skin obviates the need for obliteration of the middle-ear mucosa and closure of the external auditory canal. In the three cases presented, no patient experienced post-operative wound complications related to the canal wall down procedure. The integrity of the intact posterior canal wall skin proved sufficient in these cases to prevent electrode extrusion within the external auditory canal. The theoretical complications of this approach include canal stenosis, retraction pocket development and electrode extrusion. However, long-term follow up of our three patients (albeit a limited number), without pre-operative evidence of eustachian tube dysfunction, showed that the intact vascular supply of the posterior canal wall skin was sufficient to prevent such complications.




