An elevated prothrombin time in a 6-year-old girl before catheter closure of a patent arterial duct identified liver dysfunction eventually leading to a diagnosis of an Abernethy malformation from the portal vein to the coronary sinus. CT confirmed the echocardiographic findings along with the presence of bilateral superior caval veins without any bridging vein between them (Fig 1). Angiography with balloon occlusion via left jugular venous access demonstrated small portal vein radicles and insignificant elevation of portal venous pressures. Thus, the malformation was occluded using a vascular plug. The arterial duct was also occluded using a coil (Fig 2, Supplementary video 1). She received oral anticoagulation to prevent portal vein thrombosis and propranolol to reduce portal venous pressures for 1 year. She remained well after 2 years with no residual flows.
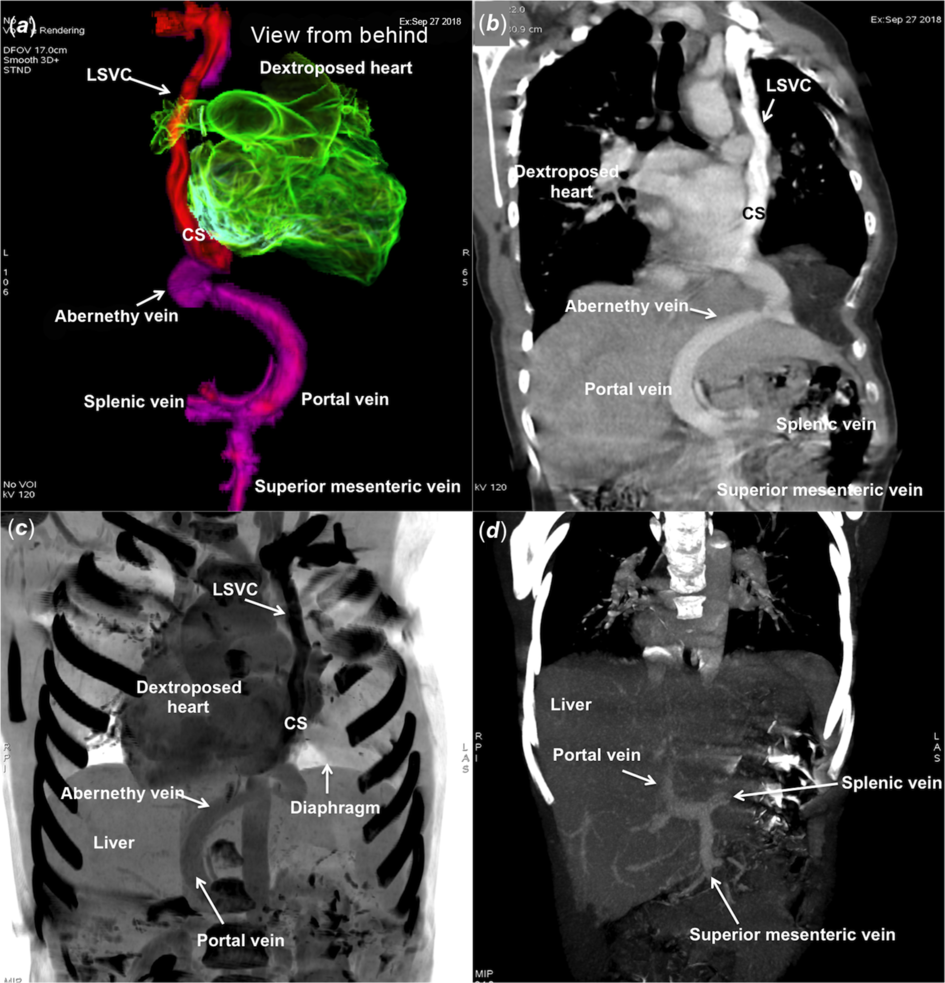
Figure 1. Volume rendered colour coded ( a ) and curved multiplanar reformatted ( b ) computed tomographic images show Abernethy malformation connecting portal vein to persistent left superior caval vein and coronary sinus. Postprocessed maximum intensity projection image ( c ) shows the supradiaphragmatic drainage of Abernethy vein. Normal portal vein radicals are seen on follow-up imaging ( d ) after 1 year.

Figure 2. Left superior caval vein angiogram ( a ) through left jugular venous access demonstrates its drainage through the coronary sinus to the right atrium. A femoral venous catheter is advanced through the patent arterial duct in to the descending aorta. Mild right lung hypoplasia causes a dextroposition. Abernethy vein angiogram shows splenic vein forming the portal vein ( b ) and its drainage into the coronary sinus. Superior mesenteric vein was seen on Balloon occlusion ( c ) fills superior mesenteric vein and demonstrates insignificant increase of pressures. Entry of Abernethy vein is closed ( d ) with a vascular plug.
While most congenital extrahepatic portosystemic shunts connect to inferior caval vein or its tributary, a supradiaphragmatic venous connection is extremely unusual. During the 4th week of embryonic life, the drainage of the vitelline and left umbilical veins to the developing heart is interrupted by the septum transversum and liver parenchyma to form hepatic sinusoids (Fig 3). The distal left umbilical vein loses its connection to the left horn of the venous sinus and communicates with the vitelline vein to form the venous duct which connects to the left branch of portal vein. A persistent left umbilical vein in the embryo explains a supradiaphragmatic Abernethy vein connecting to the coronary sinus, left superior caval vein, or left brachiocephalic vein (Fig 4). Uncorrected connections may lead to liver dysfunction, hyperammonaemia, galactosaemia, hyperplastic liver nodules, portopulmonary syndrome, pulmonary hypertension, or hepatic encephalopathy. Reference Loomba, Telega and Gudausky1
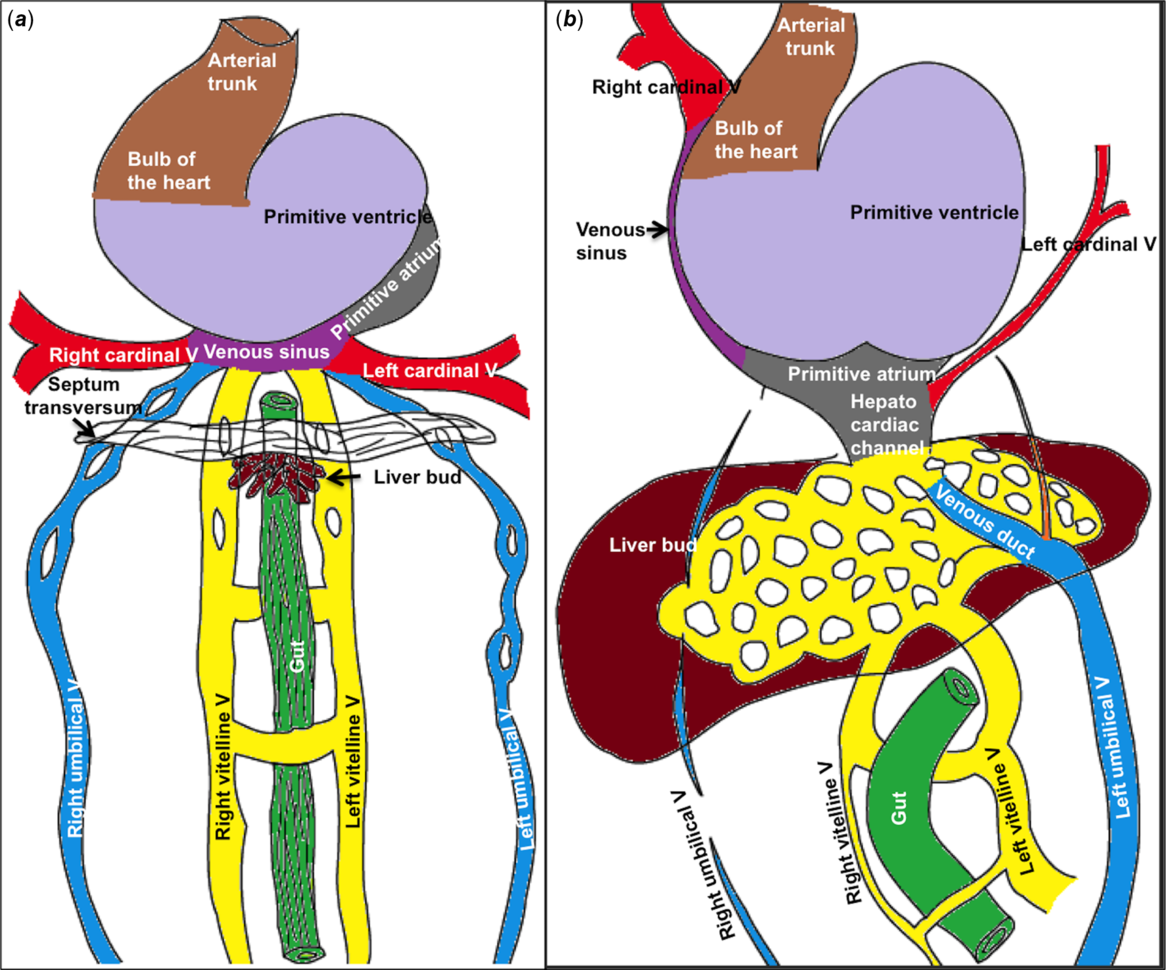
Figure 3. Vitelline and umbilical veins are interrupted by septum transversum and the developing liver bud and incorporated into the hepatic sinusoids in a 4-week embryo ( a ). In the next 2 weeks, progressive liver enlargement is associated with obliteration of the right umbilical vein and cranial part of left umbilical vein. The caudal part of left umbilical vein communicates to portal vein through portal sinus and hepato cardiac channel through the venous duct ( b ).
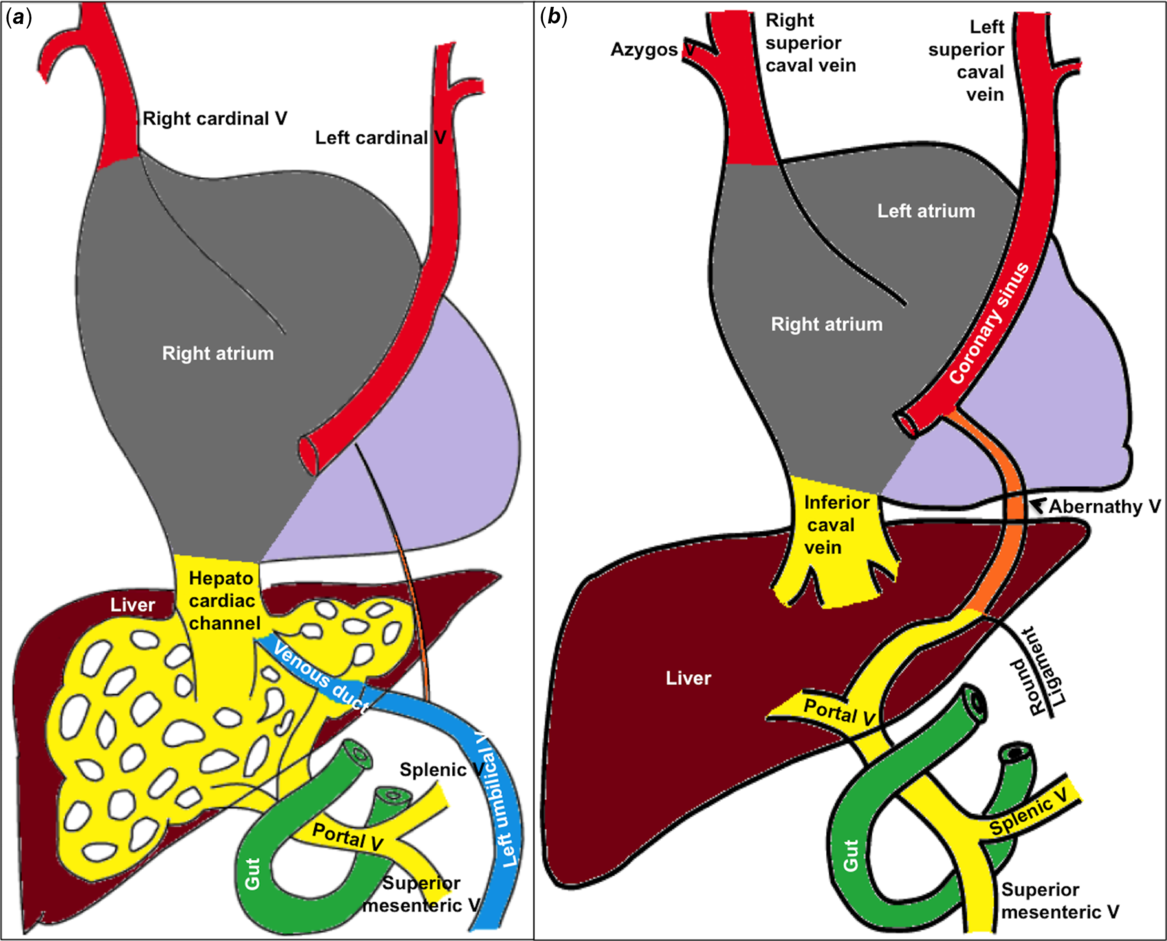
Figure 4. The hepatocardiac channel derived from cranial part of fused vitelline veins forms the inferior caval vein that also receives left umbilical venous blood through the venous duct. Variable absorption of caudal part of vitelline veins ( a ) explains the relation of different parts of portal vein to the duodenum. Non-obliteration of cranial part of left umbilical vein ( b ) creates an Abernethy connection from portal vein to left horn of venous sinus.
Acknowledgements
None.
Financial Support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the Indian Council of Medical Research and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional committees of Madras Medical Mission, Chennai, India.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951120003571







