Introduction
Obstructive adenoid enlargement is commonly implicated as the major cause of chronic nasal obstruction in children. It may be assessed by various tools including history, physical examination, lateral nasopharyngeal X-ray, nasopharyngoscopy and rhinomanometry. Currently, there is little consensus on the best method of evaluating the adenoid size and the degree of nasopharyngeal airway obstruction, during pre-operative evaluation for adenoidectomy. Nasopharyngoscopy is invasive, expensive and not universally available. Rhinomanometry is poorly tolerated in children and it not applied in the routine ear, nose and throat clinic at present. Although clinical assessment has been considered essential in the pre-operative assessment for adenoidectomy,Reference Hibbert1 some investigatorsReference Hibbert and Tweedie2, Reference Hibbert, Stell and Wright3 have called into question the reliability of symptoms and physical signs in the assessment of adenoid size. On the other hand, several radiological parameters on the lateral soft tissue plain X-ray of the nasopharynx have been reported to reliably evaluate the adenoid size and the degree of nasopharynx airway obstruction.Reference Jean, Fernando and Maw4–Reference Cohen, Koltai and Scott9 A few investigatorsReference Paradise, Bernard, Colborn and Janosky10, Reference Bitar, Rahi, Khalifeh and Madanat11 have reported substantial correlation between clinical assessment and roentgenographic ratings of adenoidal obstruction of the nasopharynx.
The primary care physician is usually the first to see these patients, and often relies on clinical assessment when deciding whether to refer the patient for adenoidectomy. If such clinical assessment could be standardised so as to properly evaluate the degree of nasopharyngeal obstruction, compared with radiographic assessment, this might increase the appropriateness and accuracy of referral for surgery.
The present study aimed: (1) to show that the severity of adenoidal obstruction in children can be evaluated by a simple, standardised symptomatology score, and (2) to determine the correlation between clinical symptomatology and roentgenographic assessment of nasopharyngeal airway obstruction by adenoids.
Participants and methods
The study was conducted at the otolaryngology department of the University of Nigeria Teaching Hospital, Enugu, from April 2004 to March 2005. Consecutive paediatric patients referred to the otolaryngology clinics by primary care physicians and paediatricians on account of chronic nasal obstruction were prospectively recruited. Written, informed consent was obtained from the parents or legal guardians, after the research protocol had been reviewed and approved by the University of Nigeria Teaching Hospital ethical review committee.
Patients included in this study met the following criteria: (1) continuous nasal obstruction for at least three months; and (2) the presence of one or more of the following symptoms – snoring, mouth-breathing and obstructive breathing during sleep (obstructive sleep apnoea). Exclusion criteria included: history of previous adenoidectomy; craniofacial anomalies; and nasal septal deviation.
Clinical assessment
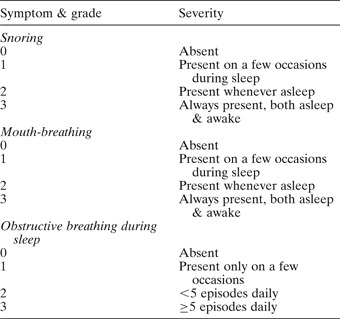
On attending the clinic, in conjunction with a detailed examination of the ears, nose and throat, each child underwent a standardised assessment of his or her symptom(s) by taking a detailed history from the parent(s) or legal guardian. When parents were unsure of their observations, they were asked to further observe their children in the daytime and during sleep over a period of one week, and the history was then retaken. The symptoms that were graded and scored were snoring, mouth-breathing and obstructive breathing during sleep. Each symptom was rated on a four-point scale (absent = zero, mild = one, moderate = two, severe = three), as shown in Table I. The total symptomatology score represented the sum of the scores for individual symptoms. The minimum possible symptomatology score was one and the maximum possible score was nine. The symptomatology score for each patient was rated into three grades, as follows: symptomatology score of one to three = ‘mild’, four to six = ‘moderate’ and seven to nine = ‘severe’.
Table I Four-point clinical rating scale for adenoidal symptoms
Roentgenographic assessment of adenoidal obstruction
Radiological assessment of the degree of nasopharyngeal airway obstruction was made using an adenoidal–nasopharyngeal ratio parameter derived from the lateral soft tissue X-ray of the postnasal space.Reference Fujioka, Young and Girdany6, Reference Elwany7 The X-rays were obtained at a tube-cassette distance of 180 cm, with patients erect. The beam was centred on the external auditory meatus with the head in true lateral position. The dimensions of the adenoid and nasopharynx were measured with a transparent rule, in millimetres, as shown in Figure 1. The adenoidal–nasopharyngeal ratio was obtained by dividing the adenoidal measurement by the nasopharyngeal measurement.Reference Fujioka, Young and Girdany6, Reference Elwany7 All the values obtained were approximated to two decimal points. The degree of nasopharyngeal airway obstruction obtained was classified as showing minimal (adenoidal–nasopharyngeal ratio 0.50–0.62), moderate (adenoidal–nasopharyngeal ratio 0.63–0.75) or gross (adenoidal–nasopharyngeal ratio 0.76–0.88) obstruction.
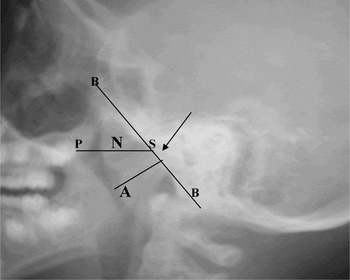
Fig. 1 Photograph of patient's postnasal X-ray, illustrating the measurements for calculation of the adenoidal–nasopharyngeal ratio. Line B runs tangential to the basi-occiput. The nasopharyngeal measurement N denotes the distance between the posterior border of the hard palate and the antero-inferior aspect (S) of the spheno-basi-occipital synchondrosis (arrowhead). When the synchondrosis is not visible, point S is determined as the point on the anterior edge of the basi-occiput which is closest to the intersection of lines A and B.7
Data analysis
Data were analysed using the Statistical Package for the Social Sciences version 11.5 software. The correlation between the symptomatology score and the roentgenographic rating was tested with Pearson's correlation. Pearson's chi-square was used to study the association between the various symptomatology score grades and the corresponding roentgenographic ratings.
Results
Sixty-four children (42 boys and 22 girls) aged one to 12 years met the inclusion criteria; 62.5 per cent were aged three years and below.
Table II shows the distribution of symptomatology scores among the various age groups. A severe symptomatology score grading was found in 62.5 per cent of children aged three years, versus 16.7 per cent of children older than three years. A symptomatology score grading of either moderate or severe was observed in 95 percent of children aged three years. Symptomatology score was significantly correlated with age (r = −0.657; p < 0.01). Younger children were observed to have more severe symptoms. Symptoms became increasingly less severe as the children's ages increased. The oldest child in the series showed the lowest grade of symptomatology score, with a value of two, representing mild snoring and mild mouth-breathing.
Table II Symptomatology scores by patient age

Y = years
Patients' adenoidal–nasopharyngeal ratios ranged from 0.50 to 0.88, with an overall mean of 0.718. Out of the 64 patients, 54.8 per cent had a roentgenographic rating of gross nasopharyngeal airway obstruction, and 23.4 and 21.8 per cent were rated as having mild and moderate obstruction, respectively. There was significant correlation between adenoidal–nasopharyngeal ratio and age (r = −0.340; p < 0.01). The mean adenoidal–nasopharyngeal ratio for boys did not differ significantly from that for girls (t = 0.275; p > 0.05).
Table III shows the children's clinically rated symptomatology scores alongside their corresponding roentgenographic ratings. It was observed that 78.6 per cent of cases with a severe symptomatology score grading were significantly associated with a roentgenographic rating of gross obstruction (χ2 = 14.13; p < 0.01). It was also observed that 50 per cent of cases with a mild symptomatology score grading were associated with a roentgenographic rating of minimal airway obstruction. Only 35.7 per cent of cases with a moderate symptomatology score grading were found to be associated with a corresponding roentgenographic rating of moderate obstruction. A highly significant correlation was found between the symptomatology score and the roentgenographic rating of nasopharyngeal airway obstruction by the adenoids (r = 0.419; p = 0.001). This correlation was significant both in the younger (one to three years) and in the older (older than three years) age groups (r = 0.314, p = 0.049 and r = 0.534, p = 0.007, respectively). Correlations were significant for roentgenographic grades of minimal and gross obstruction (p < 0.05 and p < 0.001, respectively), but not significant for the roentgenographic grade of moderate obstruction (p > 0.05).
Table III Roentgenographic rating of adenoidal nasopharyngeal airway obstruction, by symptomatology score

Separate analysis of the relationship between individual symptoms and roentgenographic ratings showed that the clinical ratings of snoring and mouth-breathing had a significant correlation with roentgenographic ratings (r =0.042, p < 0.001 and r = 0.359, p < 0.01, respectively). The clinical rating of obstructive breathing during sleep showed a somewhat less significant correlation with roentgenographic ratings (r = 0.294; p < 0.05), compared with ratings for snoring and mouth-breathing.
Discussion
The reliability of clinical assessment in predicting the severity of nasopharyngeal obstruction has long been the subject of debate among researchers. Some investigators have reported poor correlation between clinical ratings of mouth-breathing and the volume of adenoid subsequently removed at adenoidectomy,Reference Hibbert and Tweedie2 and between clinical ratings of mouth-breathing and the degree of symptomatic improvement following receipt or non-receipt of adenoidectomy.Reference Hibbert and Stell12 Other researchers have reported limited correlation between clinical and roentgenographic ratings of adenoidal obstruction.Reference Crepeau, Patriquin, Poliquin and Tetreault13, Reference Sorensen, Solow and Greve14 These less favourable results are probably due to the fact that the symptoms and/or physical signs assessed in those studies were either not graded or not standardised. In one of the studies,Reference Hibbert and Tweedie2 symptoms and signs were evaluated against the volume of adenoid removed at adenoidectomy. The degree of nasopharyngeal airway obstruction was shown to be a more reliable parameter than the actual size or volume of resected adenoids in the evaluation of adenoidal obstruction severity.Reference Goldman and Bachman8, Reference Crepeau, Patriquin, Poliquin and Tetreault13, Reference Tankel and Cheeseman15 On the other hand, some researchers have reported substantial correlation between clinical and roentgenographic ratings of the degree of nasopharyngeal obstruction, similar to the current findings.Reference Elwany7, Reference Paradise, Bernard, Colborn and Janosky10, Reference Bitar, Rahi, Khalifeh and Madanat11, Reference Maw, Jeans and Fernando16 However, the methods used in these studies for clinical assessment of adenoidal obstruction were different from those adopted in the current study. In one study,Reference Maw, Jeans and Fernando16 non-specific signs of adenoidal obstruction (such as granular pharyngitis) were included in the clinical assessment. In other series,Reference Elwany7, Reference Bitar, Rahi, Khalifeh and Madanat11 symptoms were not graded. In the only other study that adopted grading of physical signs, the clinical assessment disregarded the nocturnal symptoms of adenoidal obstruction, such as snoring and obstructive breathing during sleep.Reference Paradise, Bernard, Colborn and Janosky10
The clinical ratings used in this study assessed the more common and relatively specific symptoms encountered in patients with adenoidal obstruction in the absence of other contributory nasal pathologies. The grading of the symptoms reflected a progressive increase in the clinical severity of adenoidal obstruction. For instance, when considering snoring, adenoidal obstruction that caused patients to breathe noisily both during the daytime and during sleep was considered more severe than obstruction that caused noisy breathing only during sleep. The same consideration was similarly applied in the case of mouth-breathing.
The scores assigned were based on the history obtained from the parents or legal guardian. When parents were unsure of their observations, they were asked to observe their children at intermittent intervals during the daytime and during sleep, over a period of one week, and the history was then retaken.
• Obstructive adenoidal enlargement is commonly implicated as the major cause of chronic nasal obstruction in children. Although clinical assessment is considered essential, there is little consensus on its reliability
• This study aimed to determine the correlation between graded symptomatology assessment and roentgenographic assessment of adenoidal obstruction, in a group of 64 children
• Correlation between symptomatology assessment and roentgenographic assessment was significant for roentgenographic ratings of minimal obstruction (p < 0.05) and gross obstruction (p < 0.001)
• Clinical ratings of adenoidal symptoms in children provide reasonably reliable assessment of the presence and severity of nasopharyngeal airway obstruction
Roentgenographic assessment was used as the ‘gold standard’ for validating the symptomatology score, because it constituted the only generally available, acceptable, objective, noninvasive means of assessing the extent of adenoidal obstruction of the nasopharyngeal airway. Also, roentgenographic assessments have been found to correlate well with the size and volume of adenoid tissue removed or observed at surgery.Reference Fujioka, Young and Girdany6, Reference Cohen, Koltai and Scott9
The advantage of the adenoidal–nasopharyngeal ratio parameter used in this study was that it reflected both adenoidal size and nasopharyngeal capacity.Reference Fujioka, Young and Girdany6, Reference Elwany7 However, the literature is not definite as to the generally accepted normal size limits of the adenoids and nasopharyngeal airway, and the objective criteria used for the diagnosis of pathological enlargement. The classification of degree of nasopharyngeal airway obstruction used in this study was similar to that used in previous reports.Reference Fujioka, Young and Girdany6, Reference Elwany7
The strong correlation between symptomatology score of adenoidal obstruction and roentgenographic rating of nasopharyngeal airway obstruction found in this study allows confidence in the reliability of the symptomatology score. It shows that graded assessment of adenoidal obstruction symptomatology is comparable to roentgenographic assessment in evaluating the severity of nasopharyngeal airway obstruction by enlarged adenoids. The reliability of the symptomatology score was quite good at the extreme of gross obstruction, reasonably good for minimal obstruction, but poor for moderate obstruction. Similar findings were observed in another study which compared clinical signs with roentgenography in the assessment of adenoidal obstruction.Reference Paradise, Bernard, Colborn and Janosky10
In this study, the adenoidal symptoms and the roentgenographic ratings of the degree of nasopharyngeal obstruction were found to be significantly more severe in younger children than in older ones. This concurs with the reports of other researchers.Reference Fujioka, Young and Girdany6, Reference Bitar, Rahi, Khalifeh and Madanat11, Reference Haapaniemi17 It has been shown that the adenoid has a relatively higher growth rate than the nasopharynx between the ages of two and five years. However, these growth rates begin to reverse between the ages of seven and nine years, when the adenoid begins to regress while the nasopharynx continues to grow.Reference Johannesson18, Reference Jeans, Fernando, Maw and Leighton19
Conclusion
Clinical ratings of adenoidal symptoms in children provide a reasonably reliable assessment of the presence and severity of nasopharyngeal airway obstruction. The technique of assessment is easy to use and is particularly valid when obstruction is either minimal or gross. Such symptomatic assessment may be of value to primary care physicians and paediatricians when deciding which patients to refer for an otolaryngological opinion. However, because clinical assessment is not infallible, it would seem sensible for the otolaryngologist to obtain roentgenographic confirmation of the degree of adenoidal obstruction for those children with high symptom scores who are being considered for adenoidectomy. Those children with low symptom scores could be treated with reassurance, without the need for roentgenography.






