Hospitals have a pivotal role in providing effective health services during critical incidents; they are expected to manage extra admissions while continuing to provide care for existing patients.Reference Tang, Fitzgerald and Hou1,Reference Vugrin, Verzi and Finley2 Zhong et al. define hospital resilience as the ability to resist, absorb, and respond to disasters’ consequences by providing additional services (eg, on-site rescue, prehospital care, emergency treatment, critical care, decontamination and isolation), and then to recover or to adapt to a new situation.Reference Zhong, Hou and Clark3
Research on hospital resilience and its potential impact on risk reduction and community resilience have increased over the years.Reference Chand and Loosemore4-Reference Cimellaro, Malavisi and Mahin6 Hospital resilience is as crucial as maintaining other lifeline services, such as water and electric power supply. It minimizes the impact of disasters on vulnerable populations.Reference Bruneau, Chang and Eguchi7 A report published by the World Health Organization (WHO) showed the importance of applying a resilience approach in enhancing the capacity of health systems through “decreased vulnerability” and “improved choices and opportunities” in an unstable and changing climate.8
To achieve resilience in a hospital, it is essential to coordinate major related processes, resources, and technologies with the aim of managing expected and unexpected changes.Reference Zhong, Clark and Hou9,Reference Samsuddin, Takim and Nawawi10 It is also important to consider the main factors that can affect hospital resilience, preparedness, adaptive capacity, and rapid response to an unexpected incident.Reference Chand and Loosemore4,Reference Adini, Goldberg and Laor11,Reference Barbera, Yeatts and Macintyre12
Using concepts like preparedness and continuity, there have been a variety of studies conducted on the issue of coping strategies and resistance during disasters.Reference Samsuddin, Takim and Nawawi10,Reference Schreiber, Yoeli and Paz13,Reference Jafar and Taneja14 The issue has also been raised increasingly in hospital-related topics.Reference Chand and Loosemore4,Reference Cimellaro, Malavisi and Mahin6,Reference Zhong, Clark and Hou9,Reference Takim, Samsuddin and Nawawi15 Although the WHO considers it an important issue and has published various reports on hospitals’ infrastructure preparedness and safety, the organization has not provided a comprehensive framework for conceptualizing and measuring resilience in hospitals.
Many different factors affect hospital resilience with complex relationships. Therefore, it is essential to develop a general framework to address the issue. Elaborating on the concept and critical issues of hospital resilience, Zhong et al. have presented a framework along with an assessment tool.Reference Zhong, Clark and Hou16 The objective of the present study is to investigate the influencing factors on hospital resilience and consider the resilience process and the key components of hospitals.
METHODS
This systematic review of the existing literature followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelinesReference Moher, Liberati and Tetzlaff17 and the framework proposed by Xiao et al. and Jesson et al. for conducting systematic reviews.Reference Xiao and Watson18,Reference Jesson, Matheson and Lacey19
After clarifying the purpose of the study and formulating the research questions, proper key words and search strings were selected. In line with other systematic reviews on hospital resilience,Reference Zhong, Clark and Hou16 several key words were searched in online databases. The search strings were formulated by using the words “hospital” combined with “resilience,” “resilient,” “resiliency,” “resilient*,” “preparedness,” “risk mitigation,” and “continuity” by AND/OR connectors. The key words were searched in the titles and abstracts of published articles in Scopus, Web of Science, EBSCO, SAGE, Google Scholar, and PubMed. These databases are highly widespread and have been frequently used in the literature.Reference Tang, Fitzgerald and Hou1,Reference Tukamuhabwa, Stevenson and Busby20 Table 1 shows more details of the search protocol.
TABLE 1 Search Protocol

The following inclusion criteria were used to select the related papers for the present study:
The papers published in 2000–2018 were included because the issue of resilience has appeared in the related literature since 2000.
The papers published in English were included because English is the dominant language of research in the field of resilience and hospital resilience.
Different types of papers were included (eg, empirical, literature review, conceptual) to have a more comprehensive systematic literature review. Since this study intended to identify and synthesize various approaches to the factors that influence hospital resilience, all articles dealing with statistical analysis, documentation and qualitative composition, and hospital experiences from various disasters were examined disregarding their research methods.
Hence, articles on the resilience of nurses, doctors, patients, and hospital buildings, the ones examining patients’ personal resilience in the face of illness or individual resilience of doctors and nurses in the face of patients were excluded. Furthermore, articles that investigated seismology due to geographical and geological specialization were excluded because they were outside the scope of the present study. Thus, only the studies that considered general hospital resilience with all of its components were selected to be analyzed
RESULTS
A total of 391 articles were retrieved through searching the key words in the selected online databases. In addition, 2 more papers were found by hand-searching and searching for cross-referencing citations. Duplicate papers (71) were removed from the results of the searches. Then, screening the titles of the papers, 213 were irrelevant because they investigated the resilience of nurses, doctors, patients, hospital buildings, and seismology, and thus they were excluded. Afterward, the abstracts of the remaining 109 articles were examined; 49 articles were selected to be reviewed. After that, 33 articles were excluded for the absence of eligible criteria for exclusion and inclusion. Finally, the selected articles were reviewed after applying the inclusion and exclusion criteria. According to the inclusion and exclusion criteria, these 16 articles (14 journal articles and 2 reports by the WHO) had dealt with factors that might have an influential role in hospital resilience (Figure 1). Moreover, the Critical Appraisal Skills Program (CASP) tools21 were used to assess the quality of the selected articles. CASP tools present a number of questions that deal with some principles or assumptions of qualitative research. Figure 1 shows the strategy for searching and selecting the articles according to the PRISMA guidelines.
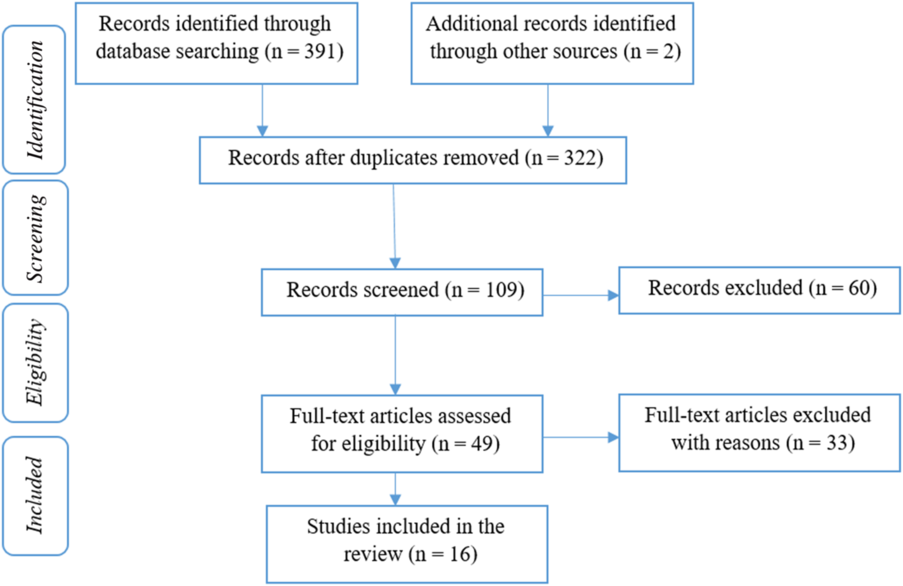
FIGURE 1 Flow Diagram.
Details of each article and their special features, including authors, publication year, research method, and research population were evaluated. Table 2 provides the details of each article.
TABLE 2 Data Extraction Sheet

Data synthesis was performed through using content analysis to recognize what factors affect hospital resilience and how those factors might enhance and reduce hospital resilience. Content analysis describes some phenomena systematically and objectively and attempts to quantify phenomena.Reference Evans and FitzGerald22 In the present study, the theories from hospital resilience as well as resilience studies were used to codify and construct the primary framework. To achieve more reliability, 2 researchers independently read and coded the articles. Although the coding results were close to each other, they discussed the results and negotiated with each other about codes. Then, the articles were coded for the second round and the results improved. As coding proceeded, the primary framework was developed and refined; first, the emerging themes were identified, and then the factors influencing hospital resilience were specified based on the developed framework. Finally, the studies that described the challenges and drivers of hospital resilience were analyzed.
Review of the finally selected papers showed a steady growth of articles addressing hospital resilience, with a significant increase after the year 2013 (Figure 2). In addition, authors of the articles used the word preparedness more in the years before 2013 to convey the concept of hospital resilience. Moreover, when hospital resilience started to appear in the literature, the focus of the articles was on hospital preparedness; afterward, the focus shifted to measuring the general resilience and the lessons learned from hospital experiences. Preparedness relies exclusively on structural measures (eg, human, equipment) while it has little concern for hospital infrastructural safety and emergency services.Reference Nelson, Lurie and Wasserman23 Hospital resilience includes structural components (eg, facility safety), non-structural components (eg, staff, medication, and equipment), emergency medical functions (eg, continuity of medical services) and disaster management capacity (eg, plan and procedure, crisis communication, community linkage).Reference Zhong, Clark and Hou16

FIGURE 2 Number of Studies Based on the Published Year.
Regarding the methodologies used in the published papers, although some of them had used multiple methods (Figure 3), 4 major categories were identified: theorizing and conceptualization (7%), survey (43%), review (29%), and case study (21%). Our findings indicated that the survey method has received more attention, because this type of research describes the basic characteristics of the study population through investigating a sample and then generalizing the results to the whole population.Reference Fowler24 In addition, the survey is a good methodology to measure resilience in hospitals. The review method collects and submits documents through using a qualitative approach.Reference Barrett and Bolt25 The review articles investigated hospital preparedness. Case study research is an inquiry that focuses on describing, understanding, predicting, and/or controlling an individual.Reference Woodside26 This type of article investigated hospital infrastructure.

FIGURE 3 Research Method.
The results also revealed that Southeast Asian countries had a special interest in hospitals’ resilience compared with other countries. These countries are highly populated and they are highly exposed to disasters. In addition, according to the 2016 disaster report,Reference Guha-Sapir, Hoyois and Wallemacq27 the countries reported to have the highest incidents are China, the United States, India, Indonesia, the Philippines, Vietnam, Japan, Pakistan, and Mexico. Therefore, it is justified why hospital resilience and preparedness are important to these mentioned countries. Table 2 provides more details on the special features of the reviewed articles, including author, publication year, research method, and research location.
To discuss the content of the existing literature on hospital resilience, the present study employed a comprehensive matrix as a conceptual framework. This matrix will help the readers get an overview of the study. A process perspective was observed in the literature on hospital resilience. The articles in the sample were clearly distributed according to the different process stages (ie, preparedness, response, and recovery and growth) and key components of hospital resilience (staff, infrastructure, management and logistics; Table 3). This framework can be used by hospital managers as a checklist of key factors that influence hospital resilience at different stages. It enables the hospital to keep providing health care services at the time of disaster.
TABLE 3 Impact Factors Matrix.

Some papers showed that resilience consists of 3 stagesReference Chand and Loosemore4,Reference Sheffi and Rice28 of preparedness, response, and recovery and growth. Through preparedness, the hospital maintains its function during disaster and provides predictions and awareness of the disturbances that will occur. In the response phase, the hospital’s performance is at its lowest. The effective functioning of a hospital at this stage depends on its proper preparedness. After the disaster, the hospital should return to its original state and provide services to the patients (see Table 3).
In each stage, there are 4 areas of staff, infrastructure, management, and logistics, which constitute the Impact Factors Matrix (see Table 3). Each sheet of matrix shows the factors that influence hospital resilience. The following sections present these sheets.
PREPAREDNESS
Staff
Competency plays a significant role in the resilience and continuity of hospital services before, during, and after the occurrence of any disaster.Reference Adini, Goldberg and Laor11,Reference Labarda, Labarda and Lamberte29 With competent staff, the provision of hospital services never stops.Reference Labarda, Labarda and Lamberte29 Thus, it is important to ensure that staff are efficient because they have a positive effect on the preparedness of the hospital in emergency situations.Reference Adini, Goldberg and Laor11 Staff training should focus on enabling them to manage patients’ evacuation plans, to use activating alarms appropriately based on the type of incident, and to increase their responding speed.Reference Adini, Goldberg and Laor11,Reference Jafar and Taneja14 These competencies should be built and improved by repeated emergency simulations and drills that involve a large group of staff, based on different natural and man-made scenarios.Reference Barbera, Yeatts and Macintyre12,Reference Jafar and Taneja14 Moreover, staff capacity building should encompass networking with different stakeholders, team working, and sharing experiences.Reference Chand and Loosemore4,Reference Zhong, Clark and Hou16,Reference Sam, Geroy and Pesigan30
Hospital Infrastructure
It includes different aspects like architectural, non-architectural (electrical systems, communication systems, emergency exit systems, etc.), and functional (access, internal circulation, security systems, utility systems, etc.).Reference Samsuddin, Takim and Nawawi10 According to the WHO, fostering standard protocols and operating procedures in hospitals is among the factors that have a great impact on resilience.Reference Jafar and Taneja14,Reference Labarda, Labarda and Lamberte29 In addition, determining similar codes of signals in hospitals to communicate important messages can result in faster response and cooperation in case of a crisis involving an area.Reference Jafar and Taneja14
Management
In the preparedness phase, developing a plan for hospital disaster management by competent individuals has a great impact on hospital resilience.Reference Jafar and Taneja14 Meanwhile, it is suggested to focus on the probable demands and capacity of available resources, as well as hospital in-crisis policies and procedures, and activation schemas in different anticipated scenarios.Reference Sam, Geroy and Pesigan30-Reference McDaniels, Chang and Cole32 In addition to the necessary planning, enough funds should be allocated for the training of human resources and maintaining essential equipment.Reference Barbera, Yeatts and Macintyre12 Fostering a knowledge and experience sharing system between managers at different levels of the hospital hierarchy is also of great value regarding hospital resilience.Reference Chand and Loosemore4 Frequent assessment of the hospital emergency response planReference Adini, Goldberg and Laor11 can develop warning and surveillance systemsReference Tang, Fitzgerald and Hou1,Reference Zhong, Hou and Clark3 and lead to more relevant response plans.Reference Zhong, Clark and Hou9
Logistics
The hospital should prepare, store, maintain, and upgrade the required resources before an event occurs so that it can take care of many victims and continue service delivery.Reference Barbera, Yeatts and Macintyre12,Reference Cristian31 Surge capacity for staff, equipment, pharmaceutical products, and physical space should also be considered in any disaster preparedness plan.Reference Tang, Fitzgerald and Hou1,Reference Zhong, Hou and Clark3,Reference Djalali, Castren and Khankeh33
RESPONSE
Staff
When an incident occurs, the hospital needs more staff to serve the growing number of victims. Therefore, organizing volunteer staffs or other eligible people in the response phase is crucial in hospital resilience.Reference Labarda, Labarda and Lamberte29
Infrastructure
Hospitals should be accessible from different directions during a disaster.Reference Chand and Loosemore4,Reference Djalali, Castren and Khankeh33 In addition, they should develop strategies for patients’ protection and evacuation when necessary. Usually, emergency medical services performs patients’ evacuation according to the priorities that have been set before.Reference Zhong, Hou and Clark3,Reference Chand and Loosemore4,Reference Adini, Goldberg and Laor11,Reference Zhong, Clark and Hou16,Reference Djalali, Castren and Khankeh33
Management
The hospital must have an appropriate hierarchical command system, and the existence of a leader for the command system is essential to prevent chaos.Reference Zhong, Hou and Clark3,Reference Labarda, Labarda and Lamberte29 Establishing a communication system with other hospitals is required for the continuity of medical care or referring patients that need specific services. Moreover, communicating with other social and civic organizations (governmental or non-governmental), the hospital can help victims with other non-medical needs.Reference Tang, Fitzgerald and Hou1,Reference Zhong, Hou and Clark3,Reference Bruneau, Chang and Eguchi7
Logistics
The performance of various supporting systems in a hospital (ie, water supply, electricity, and communication systems) is very influential in the process of service delivery.Reference McDaniels, Chang and Cole32,Reference Achour, Miyajima and Pascale34 A large number of medical equipment, lighting, hospital information systems, and computers are dependent on electricity. Therefore, it must be determined whether the hospital has an emergency alternative for those supporting systems.Reference Zhong, Clark and Hou9 Other organizations and hospitals can facilitate medical services through networking and sharing equipment, staff, and other necessary resources.Reference Labarda, Labarda and Lamberte29 A lack of proper interorganizational coordination will restrict the availability of sparse resources in a time-sensitive response to a disaster.Reference Zhong, Clark and Hou16
RECOVERY
Staff
Hospital management can use lessons learned from past disasters to improve its resilience. They should incorporate the lessons in future staff training. In addition, such experiences can contribute to better planning for preparedness in future disasters.Reference Barbera, Yeatts and Macintyre12,Reference McDaniels, Chang and Cole32
Infrastructure
It is important to check the hospital infrastructure as well as supplies and equipment in the recovery phase of an incident. Rapid replacement and maintenance of essential infrastructure, along with ensuring their efficacy, are crucial to restore hospital resilience.Reference Bruneau, Chang and Eguchi7,Reference Labarda, Labarda and Lamberte29
Management
The hospital should benefit from a rigorous recovery strategy to adapt to a new situation and be prepared as it was before.Reference Chand and Loosemore4
Logistics
Recovery needs time and sufficient resources. It is important for a crisis-hit hospital to gain the support of the government and other organizations. Hospitals need financial resources to return to their former optimal condition. Usually, government and the international community provide funds for the hospitals.Reference Sam, Geroy and Pesigan30 Moreover, the cooperation of other service-providing organizations can decrease the pressure on the hospital and provide the necessary time for the hospital to recover.Reference Barrett and Bolt25
DISCUSSION
This research has systematically reviewed the literature on the factors influencing hospital resilience. After reviewing the articles in detail, it became clear that recent articles have focused on all 3 resilience process phases (preparation, response, and recovery), whereas previous articles had only focused on hospital preparedness. It is indicated that, although the preparation phase is the most important phase of the resilience process, the response and recovery phases also need proper consideration. Focusing on factors that influence hospital resilience creates a pathway for hospitals to prevent disturbances and continue providing services during an event, and return to the pre-disaster situation as well. The degree to which a hospital considers those factors can affect the success or failure of the hospital resilience. Content analysis of the reviewed articles highlighted a lack of papers concerning each key component of hospitals that influence its resilience. The gap allowed us to present our framework that brings attention to 2 dimensions of hospital resilience: the resilience process phase (preparation, response, and recovery) and the key components of a hospital (staff, infrastructure, management, and logistics). By putting these 2 dimensions beside each other and identifying the factors that influence hospital resilience, we provided strategies for the development of hospital resilience. These strategies can be subsumed under the rubric of proactive, concurrent, and reactive strategies to manage hospital resilience. The presented framework will help readers get an overview of the study. In addition, it can be used by hospital managers as a checklist for key factors that influence hospital resilience in different phases; therefore, they can take actions to keep providing services in the time of disasters.
The results also show that proper training and drills directed to empower hospital staff have gained the most attention in many papers. Developing standard policies and procedures for maintaining hospital infrastructure in the preparedness phase has also been shown to be of great interest. Proactive disaster management planning has been underlined in many studies. Moreover, advancing surge capacity by providing rapid access to necessary resources has been considered in the logistics section.
There are some limitations to this study. Exclusion criteria were focused on the overall resilience of the hospital; while obtaining more precise results, some other factors such as the resilience of individuals, structural resilience, and so forth, were to be considered. Since the concept of resilience has been taken from the management field, it was not used to search for online medical databases. This limits the scope of this search.
CONCLUSIONS
This study presents a conceptual framework for understanding hospital resilience. The framework links different phases of the resilience process (preparedness, response, and recovery) with different dimensions of hospitals (staff, infrastructure, management, and logistics) to mention the factors influencing hospital resilience. The findings will have implications for hospital managers. While in recent years, disruptive events (of domestic or foreign origin) have significantly been increased, the framework can be used to create a comprehensive plan for promoting hospital resilience. In addition, the present authors suggest that future research can address the social determinants influencing the resilience of the hospital (eg, economics, politics, and culture), as well as the hospital supply chain.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.








