Introduction
Idiopathic sudden sensorineural hearing loss (SNHL) usually occurs suddenly and unilaterally. Although its cause has not been clarified, various possible aetiologies have been proposed, such as viral infection, vascular dysfunction, neurological disorder or autoimmune disease.Reference Chang, Park, Lee, Rah and Choi1 Previous studies have reported the effectiveness of various treatments as well as prognostic markers for idiopathic sudden SNHL; however, the treatments remain controversial and biomarkers for accurately predicting the prognosis of idiopathic sudden SNHL are not well established.Reference Attanasio, Russo, Di Porto, Cagnoni, Masci and Ralli2,Reference Nonoyama, Tanigawa, Shibata, Nakao, Horibe and Katahira3 Therefore, more effective treatment options or biomarkers for predicting the final outcomes in the early stage of the disease would be very valuable.
There is a growing interest in the association between iron metabolism and neurodegenerative disorders because it has been reported that iron plays a fundamental role in maintaining neural biological functions, including oxygen transport, mitochondrial respiration, and cell growth and differentiation.Reference Beard4 However, in the inner ear, iron may exert not only neuroprotective effects but also neurotoxic effects, such as acceleration of reactive oxygen species production, resulting in reduction of cochlear blood flow and apoptotic cell death in the organ of Corti.Reference Henderson, Bielefeld, Harris and Hu5 Although the role of iron in the cochlea has not been clearly established, maintaining vascular oxygen supply and mitochondrial respiration and reducing reactive oxygen species production in the cochlea is critical for improvement from cochlear damage.Reference Shi6,Reference Tabuchi, Nishimura, Tanaka, Hayashi, Hirose and Hara7
Considering the above, the prognosis of idiopathic sudden SNHL may potentially be positively or negatively influenced by serum iron levels. It has been reported that hearing loss caused by iron deficiency may gradually progress and that iron deficiency may be associated with the pathogenesis of idiopathic sudden SNHL.Reference Schieffer, Chuang, Connor, Pawelczyk and Sekhar8,Reference Chung, Chen, Lin and Hung9 Nonetheless, the relationship between the serum iron level and the prognosis of idiopathic sudden SNHL has to date not been studied. Accordingly, the purpose of this study was to investigate the association between serum iron levels and prognosis of idiopathic sudden SNHL and its usefulness as an independent prognostic biomarker in patients with idiopathic sudden SNHL.
Materials and methods
Ethical considerations
The protocol of this study (B20–056) was approved by the Institutional Review Board of Kitasato University Hospital, Tokyo, Japan. The requirement for informed consent was waived because of the retrospective nature of the study.
Patients
The medical records of patients with idiopathic sudden SNHL who underwent pure-tone audiometry at Kitasato University Hospital from 2015 to 2018 were retrospectively reviewed. The inclusion criteria were as follows: (1) idiopathic sudden SNHL of 30 dB or greater in at least three consecutive frequencies; (2) age over 18 years; (3) early therapeutic management initiated within 2 weeks from symptom onset; and (4) follow-up duration longer than 6 months. The exclusion criteria were as follows: (1) age under 18 years; (2) middle-ear or retro-cochlear pathology; (3) history of Ménière's disease or autoimmune hearing loss; (4) history of genetic or fluctuating hearing loss; (5) history of hearing aid use or otological surgery; and (6) history of intratympanic steroid injection for salvage treatment after systemic steroid administration.
Audiological evaluation
Pure-tone audiometry was performed using a conventional device (AA–78; Rion, Tokyo, Japan) in a soundproof room. Thresholds were obtained across all frequencies between 0.125 to 8 kHz, and the average bone conduction and air conduction thresholds were calculated from the thresholds at 0.25, 0.5, 1, 2 and 4 kHz. Bone conduction thresholds were used for the exclusion of conductive or mixed hearing loss.
Based on air conduction thresholds of the initial pure-tone audiogram data, the severity of hearing loss was categorised into four grades using the criteria proposed by the Acute Severe Hearing Loss Study Group of the Ministry of Health, Labour and Welfare of Japan (Table 1).Reference Yanagita, Nakashima, Ohno, Kanzaki and Shitara10 Evaluation of hearing recovery was based on the initial and final pure-tone audiogram data obtained prior to and six months after initial treatment, respectively, according to the hearing outcome criteria proposed by the Acute Severe Hearing Loss Study Group of the Ministry of Health, Labour and Welfare of Japan (Table 2).Reference Yanagita, Nakashima, Ohno, Kanzaki and Shitara10
Table 1. Criteria for the grading of hearing loss in idiopathic sudden SNHL according to the guidelines of the Acute Severe Hearing Loss Study Group of the Ministry of Health, Labour and Welfare of Japan

Pure tone average (PTA) was calculated based on pure-tone thresholds at 0.25, 0.5, 1, 2 and 4 kHz. SNHL = sensorineural hearing loss
Table 2. Final treatment outcomes according to the guidelines of the Acute Severe Hearing Loss Study Group of the Ministry of Health, Labour and Welfare of Japan

Pure tone average (PTA) was calculated based on pure-tone thresholds at 0.25, 0.5, 1, 2 and 4 kHz
Haematological evaluation
Blood samples were collected from all patients at the first visit to obtain the baseline haematological parameters so that any adverse effects of the steroid treatment could be prevented. Red blood cell count and levels of haemoglobin, haematocrit and serum iron were measured. The mean corpuscular volume was calculated as a simple ratio between the haematocrit and absolute red blood cell count.
Treatment
All patients underwent a 10-day course of systemic corticosteroid treatment (betamethasone 8 mg via intramuscular injection on the first day and betamethasone 4 mg via oral administration in the following 3 days, tapered to 2 mg in the next 3 days and to 1 mg in the last 3 days) with oral administration of vitamin b12 (1.5 mg daily) and adenosine triphosphate (300 mg daily).
Statistical analysis
Statistical analysis was performed using GraphPad Prism 8 statistical software (GraphPad Software, La Jolla, USA) or JMP (version 14.2) statistical software (SAS Institute Japan, Tokyo, Japan). The chi-square test was used to evaluate the clinical characteristics and possible prognostic factors. The t-test and non-parametric Mann–Whitney U test were applied to investigate continuous variable prognostic factors. The parameters that were statistically significant in the univariate analysis were included in the binary logistic regression for multivariate analysis. For comparisons among more than two groups, one-way analysis of variance was used followed by Dunn's multiple comparisons for post hoc test. A p-value of less than 0.05 was considered statistically significant.
Results
Patient characteristics and treatment outcome
In total, 103 patients (58 men and 45 women) were considered eligible for this study. The characteristics of all patients are presented in Table 3. The mean age was 59.3 ± 15.8 years. The mean interval between symptom onset and initial treatment was 4.0 ± 3.0 days. As accompanying symptoms and complications, 45 (43.7 per cent) patients exhibited vertigo and 32 (31.1 per cent) had diabetes. The mean hearing level threshold at the initial examination was 80.6 ± 23.3 dB. In the initial audiological evaluation, 7 ears had grade 1, 14 had grade 2, 40 had grade 3 and 42 had grade 4 hearing loss (Table 1). With regard to the final recovery, the proportion of patients with complete recovery, partial recovery, slight recovery and no improvement was 16.5, 31.1, 30.1 and 22.3 per cent, respectively (Table 2).
Table 3. Clinical characteristics of all patients
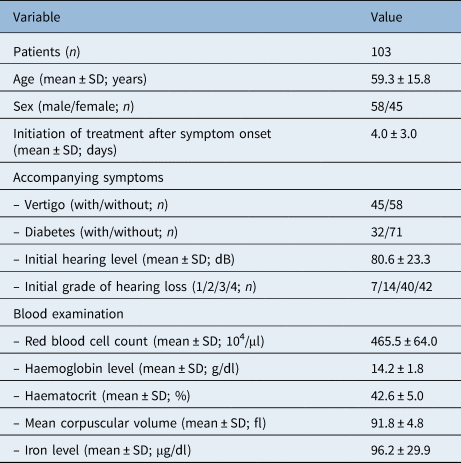
SD = standard deviation
Iron deficiency and anaemia
Iron deficiency leads to iron-deficiency anaemia, and a previous study reported that iron-deficiency anaemia was associated with the progression of age-related hearing loss.Reference Schieffer, Chuang, Connor, Pawelczyk and Sekhar8 Therefore, we next investigated the relationship among serum iron level, haemoglobin level and treatment outcome in patients with idiopathic sudden SNHL. Of the 103 patients, 9 were iron deficient (serum iron level less than 50 μg/dl), and all 9 failed to recover completely (Figure 1). Although the serum iron level decreased slightly as the prognosis worsened (Figure 1a), this change was not significant (p = 0.19). Furthermore, the haemoglobin level exhibited a statistically significant positive correlation with the serum iron level (p = 0.0005, r = 0.11; Figure 1b). However, no statistically significant correlation was observed between the haemoglobin level and the prognosis of idiopathic sudden SNHL (p = 0.52; Figure 1c).

Fig. 1. Relationship among serum iron level, haemoglobin level and disease prognosis in each prognostic group. (a) Serum iron level decreased slightly as the prognosis worsened; this change was not significant. The grey area indicates serum iron level less than 50 μg/dl. (b) The haemoglobin level exhibited a statistically significant positive correlation with the serum iron level. (c) There was no statistically significant correlation for the haemoglobin level with disease prognosis. CR = complete recovery; MR = marked recovery; SR = slight recovery; NR = no recovery
Prognostic factor
Based on the treatment outcomes, patients were divided into two groups: complete recovery and non-complete recovery (non-complete recovery: partial, slight and no recovery) groups (Table 4). In the univariate analysis, the initial hearing threshold was significantly lower in the complete recovery than in the non-complete recovery group (p < 0.01; Table 4). Moreover, the serum iron level was significantly higher in the complete recovery than in the non-complete recovery group (p < 0.05; Table 4). There were no statistical differences between the two groups in any other variates, such as age, sex, initiation of treatment, vertigo and complications of diabetes. Variables with a p-value less than 0.05 in the univariate analysis were included in the multivariate analysis. Multivariate analysis showed that a higher initial hearing threshold and the serum iron level were significantly associated with a poor prognosis in patients with idiopathic sudden SNHL, indicating that these variables might be potential independent prognostic factors for idiopathic sudden SNHL.
Table 4. Prognostic factors in idiopathic sudden sensorineural hearing loss

*n = 17; †n = 86; ‡p < 0.01; **p < 0.05
Discussion
The major finding of this study was that the serum iron level, but not haemoglobin level, was significantly higher in the complete recovery than in the non-complete recovery group, despite the significant correlation between the serum iron and haemoglobin levels. This result indicates that the serum iron level might be a novel independent biomarker for predicting the prognosis of patients with idiopathic sudden SNHL. Moreover, we demonstrated that higher initial hearing threshold was associated with a poor prognosis in idiopathic sudden SNHL, which is consistent with the findings of previous studies.Reference Kuhn, Heman-Ackah, Shaikh and Roehm11
Currently, a treatment strategy for idiopathic sudden SNHL has not been established because the aetiology of idiopathic sudden SNHL is still not fully understood. Blood circulatory disorders, hypoxia, oxidative stress and elevated intracellular levels of reactive oxygen species have been considered to be one of the crucial causes of idiopathic sudden SNHL.Reference Hsu, Hu, Chiu, Lee and Huang12 Because the cochlear tissues are supplied with oxygen and nutrients by the labyrinthine artery without collateral circulation, obstruction of the blood supply by thrombosis may cause cochlear ischemic damage, resulting in the symptoms of idiopathic sudden SNHL. Furthermore, oxidative stress was found to play a major role in cochlear damage in an animal model of hearing loss.Reference Kurioka, Matsunobu, Satoh, Niwa and Shiotani13 Considering the above, various empirical treatments, such as vasodilators, anticoagulants or antioxidant agents have been applied for idiopathic sudden SNHL to improve blood circulation and oxygen supply and reduce oxidative stress. Accurately predicting the prognosis is also extremely important in clinical practice to determine whether additional intensive treatment, such as intratympanic steroid injection, should be applied. However, there are still no treatments or prognostic factors that show unequivocal evidence of efficacy for patients with idiopathic sudden SNHL.
Iron is a critical and indispensable element for maintaining the metabolic requirements of neuronal tissues. Recently, it was reported to have a central role in the association between neurodegeneration and oxidative stress in neurodegenerative diseases.Reference Belaidi and Bush14 The auditory system is also affected by iron metabolism.Reference Castiglione, Ciorba, Aimoni, Orioli, Zeri and Vigliano15 Hearing loss caused by iron deficiency may gradually progress, and iron deficiency may be associated with the pathogenesis of idiopathic sudden SNHL.Reference Brissot, Ropert, Le Lan and Loreal16
Iron deficiency impairs energy production and, consequently, myelin production. Damage to the myelin surrounding the auditory nerve impairs the conduction velocity, resulting in auditory impairment. It has been reported that iron supplementation contributed to maintaining the integrity of the blood-labyrinth barrier and homeostasis in the cochlea.Reference Liu, Zheng, Wu, Shen, Jing and Yu17 Accordingly, iron homeostasis could be potentially associated with idiopathic sudden SNHL and be a central pathway involved in its pathophysiology.
Moreover, iron deficiency impairs erythropoiesis, resulting in iron-deficiency anaemia and leading to impaired capacity for oxygen supply. Iron-deficiency anaemia has also been demonstrated to be significantly associated with age-related hearing loss.Reference Schieffer, Chuang, Connor, Pawelczyk and Sekhar8 In contrast, iron may exert not only neuroprotective but also neurotoxic effects, such as acceleration of reactive oxygen species production, resulting in apoptotic cell death in the organ of Corti.Reference Henderson, Bielefeld, Harris and Hu5 These findings indicated that the prognosis of idiopathic sudden SNHL may potentially be positively or negatively influenced by the serum iron level.
Our findings that decreased serum iron levels were associated with poor prognosis in idiopathic sudden SNHL indicate that iron plays important roles in the recovery of idiopathic sudden SNHL mediated by promotion of vascular oxygen supply and mitochondrial respiration in the inner ear. Although none of the patients in our study had serum iron overload (more than 180 μg/dl), serum iron overload might lead to acceleration of reactive oxygen species production, resulting in poor outcome of idiopathic sudden SNHL.
Regarding iron status, we only measured haematological data, including red blood cell count, haemoglobin, serum iron level, haematocrit and mean corpuscular volume. Although these variables are not optimal for reflecting the iron status of patients with idiopathic sudden SNHL, the findings of this study have some clinical implications that are significant in terms of the understanding and management of patients with idiopathic sudden SNHL. Our results might indicate that patients with idiopathic sudden SNHL with low levels of serum iron might preferably receive comprehensive and intensive treatment in order to prevent poor results. Although the role of iron in idiopathic sudden SNHL is not well known, its effects need to be considered in the management of idiopathic sudden SNHL in clinical practice.
• Prognostic biomarkers for idiopathic sudden sensorineural hearing loss (SNHL) are not established
• Higher initial hearing threshold was associated with a poor prognosis in idiopathic sudden SNHL
• Patients with higher serum iron levels exhibited better prognosis of idiopathic sudden SNHL
• The serum iron level might be a novel independent blood biomarker to predict the prognosis of patients with idiopathic sudden SNHL
This study has some limitations. First, it was performed at a single hospital, and the sample size was relatively small. Second, ferritin, the major iron storage protein accumulating great amounts of iron, was not included in the haematological variables measured in this study. Therefore, further studies with larger populations that include the ferritin level are warranted to determine the effects of the iron metabolism on the prognosis of idiopathic sudden SNHL.
Conclusion
Higher initial hearing threshold was associated with a poor prognosis in idiopathic sudden SNHL. Moreover, the serum iron concentration was significantly higher in the complete recovery than in the non-complete recovery group. The serum iron level might be a novel independent blood biomarker to predict the prognosis of patients with idiopathic sudden SNHL.
Competing interests
None declared
Funding
This work was supported by a GSK Japan Research Grant 2019, JSPS KAKENHI grant (Grant Number 19K24052) and JSPS KAKENHI grant (Grant Number 20K18263) (all to T.K).







